Published on
Urgent message: Between the current – and still growing – volume of H1N1 flu cases and fast-approaching influenza season, the urgent care physician will be challenged to distinguish among a variety of common cold and influenza-like conditions.
Gary Klein, MD, MPH, MBA, CHS-V, FAADM
Introduction
The mainstream media have certainly accomplished the mission of alerting the public to the dangers of H1N1 flu – perhaps to the point that many are tempted to dismiss their dire predictions as “hype.”
Here are the facts: As of September 4, 2009, the Centers for Disease Control and Prevention was reporting 9,079 patients hospitalized with H1N1; 593 deaths had been attributed.
In the very near future – if not today, even – the urgent care physician will be faced with many patients who present with influenza-like symptoms or concerns that they have “the flu.”
As is the case with other urgent care concerns, appropriate and timely diagnosis will depend on history of present illness, history of recent travel, history of close family members’ illnesses, and a thorough physical examination.
The use of the latest rapid urgent care tests is also important, but these tests should be used to support one’s clinical judgement, not as a substitute for the exam.
Epidemiology
Influenza is classified as an acute respiratory illness caused by influenza A or B viruses, which occurs in outbreaks throughout the world to varying degrees each year. This epidemiologic pattern reflects the rapidly changing nature of the antigenic properties of the influenza viruses; spread of the viruses depends upon the susceptibility of the population at large.
Influenza “A” virus, in particular, has the remarkable ability to undergo quick changes in the antigenic characteristics of its envelope glycoproteins, in the hemagglutinin and neuraminidase (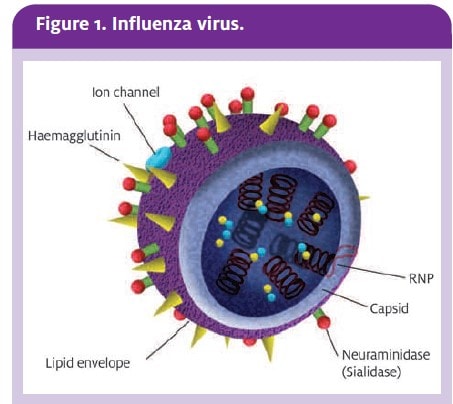 ).
).
Influenza hemagglutinin is a surface glycoprotein that binds to sialic acid residues on respiratory epithelial cell surface glycoproteins. It is this interaction that is key for initiation of infection. Once viral replication takes place, the new virions are also able to bind to the host cell, and it is the neuraminidase which cleaves these links and liberates the new virions.
Major changes in these glycoproteins, called antigenic shifts, are associated with epidemics and pandemic of influenza A. Minor changes referred to as antigenic drifts are associated with more regionalized, local outbreaks.
Clinical Findings
Urgent care physicians have to rely on their clinical acumen when diagnosing influenza because of the variety of signs and symptoms that are presented. These signs and symptoms can be caused by a variety of bacteria, cold viruses, and influenza viruses (Table 1).
ere Here Patients usually present with additional symptoms such as ocular injection and photophobia, as well as a decrease in leukocyte count. Typically, a chest x-ray, ordered to rule out pneumonia if hilar rales or wheezes are noted, will be negative.
Table 1. Comparison of Influenza and the Common Cold |
||
| Symptoms | Influenza | Common cold |
| Onset | Sudden and abrupt | Gradual |
| Fever | High (upwards of 101° F to 104°F) | Usually not present or very mild elevation of 1° |
| Myalgia | Common | Not common |
| Anorexia | Common | Not common |
| Headache | Common | Mild if at all present |
| Malaise | Common | Mild if at all present |
| Sore throat | Mild | Very common |
| Sinus symptoms | Mild | Very common |
Rapid Testing: Point-of-Care Tests
The newer rapid influenza tests available on the market, based on viral antigen detection and immunofluorescence, can assist in the difficult task of diagnosing influenza. This assumes the urgent care clinician understands their use and limitations, however.
Prompt diagnosis is important because antiviral therapy, if chosen, is more effective within 36 to 48 hours of onset of illness. Proper use of the new rapid tests may also be beneficial in curbing inappropriate use of antibiotics, by virtue of reducing the risk of misdiagnosis.
In patients presenting to the urgent care center with fever, cough, and ear pain, testing for influenza is indicated:
- when the clinical presentation and diagnosis is not clear
- if antiviral therapy is an option
- in cases of pandemic influenza.
A rapid laboratory diagnosis of influenza can be made by the detection of influenza viral antigen or nucleic acid within the respiratory tract.
Other laboratory methods include influenza viral isolation, which takes anywhere from 72 hours to a week, and serological detection of influenza antibodies, which takes two weeks to confirm. The choice of which test to order is up to the clinician based on the patient’s duration of symptoms, prevelance of influenza in the community, and the proximity to a lab testing facility.
The urgent care physician must be cognizant of the type and quality of the specimen during collection, as this may affect the sensitivity of the test. Nasal aspirates in young children and paired nasal and throat swabs in adults using the specialized viral swabs are best. A good quality respiratory tract specimen is very important for rapid antigen detection, which relies on the presence of adequate numbers of infected respiratory epithelial cells.
As you can see from Table 2, point-of-care tests are the most useful during the influenza season when the prevalence of influenza is high and the positive predictive value of the test is greatest. A positive test result in this situation is highly suggestive of influenza infection. Patients who are suspected of having influenza and have negative point-of-care tests during the influenza season should be referred for further testing with more sensitivity.
Alternatively, during periods of low influenza activity, point-of-care tests have a low positive predictive value and a false positive result is more probable. In the urgent care setting, these point-of-care tests should be utilized during high influenza periods.
Table 2. Rapid Tests for Influenza1 |
|||||
| Test | Time to results | Sensitivity | Specificity | Advantages | Disadvantages |
| Point-of-care | 15-25 min | 60% – 94% | 76% – 100% | Fast; easy to perform; no lab needed | False positive; lower sensitivity; limited shelf life |
| Immunofluorescence assay | 2-4 hours | 7% – 90% | 90% | Fast; inclusion of other respiratory virus; subtyping for influenza A is possible | Labor intensive; lab tech needed; less sensitive than nucleic acid tests |
| Nucleic acid test | 24-48 hours | 99% | 99% | Highly sensitive; specimen quality; less crucial typing and subtyping possible | Expensive; may be affected by viral genetic drift; high infrastructure requirements |
Immunofluorescence Assays
These tests are based on the same concepts as point-of-care tests (i.e., detecting and interaction between viral antigens and specific antibodies), but must be performed in a laboratory.
The direct method of immunofluorescence assays involves placing the sputum specimen onto a slide and then straining with specific antibodies fixed to a fluorescent dye.
The indirect method of immunofluorescence adds the additional step of a second fixed antibody, which increases both the sensitivity of the test and the time to obtain results. Both tests require that the slides be viewed with a fluorescence microscope to detect nuclear and cytoplasmic fluorescence straining.
Influenza immunofluorescence assays have a rapid turnaround time of three to five hours, with the additional bonus of screening for other respiratory viruses, allowing alternative diagnosis or detection of viral co-viruses.
The sensitivity of immunofluorescence assays is 70% to 90%, with specificity at 90%.2 However, performing these tests requires a specialized laboratory equipped with a fluorescence microscope and pathologists with technicians, making it more labor intensive and more costly.
Urgent care clinicians should employ this potion during severe pandemics or when diagnosis is not easily concluded.
Nucleic Acid Tests
Today, there are a variety of commercially available assays for the detection of the influenza virus nucleic acid. In addition, different nucleic acid tests (NATs) may detect and characterize the influenza virus by type (A or B), usually targeting the matrix protein, or by the subtype using primers directed against the hemagglutinin or neuraminidase genes. Commonly, the test involves a reverse transcriptase polymerase chain reaction.
Nucleic acid tests are the most sensitive diagnostic tests for influenza with sensitivity and specificity approaching 100%.1 Due to the very high sensitivity and specificity to detect both the viable and non-viable virus, the quality and timing of specimen collection is not as important as with the other antigen detection technique; though it is less labor intensive than immunofluorescence assays, the NAT is most expensive, secondary to the extremely expensive equipment and technical expertise.
Bottom Line Thoughts
The public health and urgent care benefits of a rapid diagnosis of influenza cannot be overstated. Quick detection of influenza is important not only for the patient, who may benefit from early diagnosis and the starting of antiviral medications, but also for the area served by the urgent care setting, which will help reduce the outbreak and transmission of the virus. This will, in turn, help reduce the already over-burdened emergency rooms, as well.
While rapid point-of-care tests can be very convenient, the urgent care clinician must remember that they can miss a significant number of true infections. Though a positive result is infected, a negative result is not very useful.
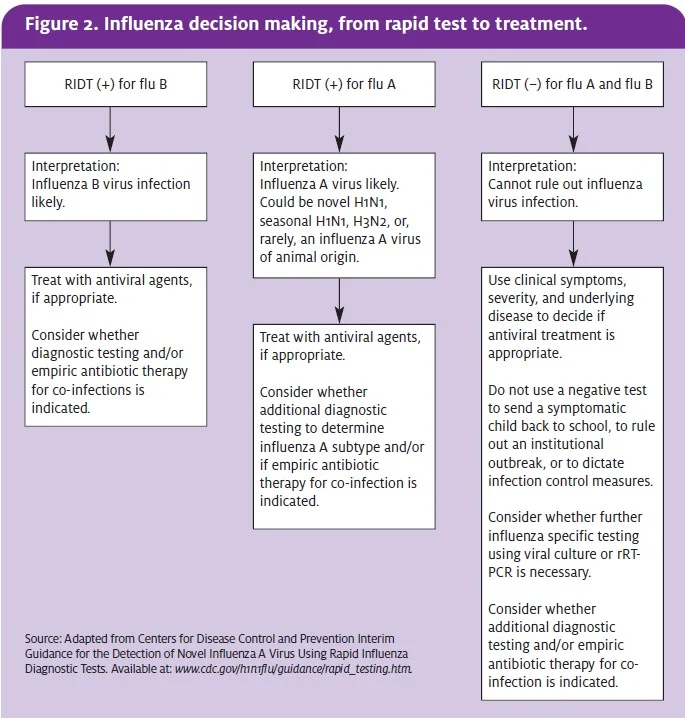
In the end, the practitioner must use his or her clinical acumen, along with the patient’s risk factor, as the best way to judge a case of influenza. Figure 2 summarizes the clinical decision-making process.
Preparing for Flu Season
Up to this point, we have focused on urgent care, influenza, and the point-of-care testing available for diagnostic purposes. Now, we turn our attention to urgent care’s role and the preparation needed in the event of a global outbreak of influenza.
This could very well include the H5N1 avian influenza, as well.
Imagine a scenario whereby the CDC announces that the avian flu is now a pandemic. Is your urgent care center ready? Have you considered what such an announcement would mean in terms of surge capacity to the clinic?
Each urgent care facility will need to conduct an assessment on current policies and procedures, identify areas that need updating, and create a pandemic/preparedness plan that will establish the way your urgent care clinic will respond during a national crisis.
Areas that need to be viewed as critical include:
- leadership
- clinical care
- human capital
- legal
- operations and supplies.
Careful planning now will be vital to ensure that the urgent care facility has taken the necessary steps to provide clinical care during a pandemic or other disaster situation. Whether an owner or a staff physician at an urgent care center, it is up to the medical director and clinic management to implement and practice a pandemic disaster plan.
By planning ahead, the leadership is ensuring that the clinic is able to respond and assist within the community it services without being disrupted. The leadership will communicate to all staff the benefits of having a plan, the benefits of practicing and implementing the plan, and including all staff members in the development of the plan.
The pandemic/disaster plan at its core will address training for employees, to include individual roles and responsibilities, information about threats, biohazards and protective actions, notification and communication, means for locating family members, emergency response procedures, and location of equipment, as well as clinic shutdown procedures.
Build preparedness into the clinic’s culture. Orientation for new clinic staff should include an overview of the contents and a copy of the clinic’s pandemic/preparedness manual.
Preparing for Vaccinations
This year, urgent care will be concerned about swine, seasonal, and avian flu.
At the time of this writing, the transmission of avian flu virus (H5N1) from person to person is rare.
Also at the time of this writing, the swine flu virus (H1N1) continues to cause illness, hospitalizations, and death in some cases. This has resulted in a rush for a separate and novel vaccine against the H1N1 virus to be developed. This novel vaccine is not intended to replace the seasonal influenza vaccine. The author recommends that each urgent care facility monitor the CDC’s website (www.cdc.gov/h1n1flu/) or stay in close contact with state and local public health officials.
Table 3, which advises on steps to take to prepare for season influenza vaccinations, can serve as an example of preparedness planning.
Table 3. Preparing for Seasonal Flu Vaccinations |
Inventory
Documentation
Reimbursement
Compliance
|
In Consideration of Other Possible Disasters
Many of the pre-emptive steps recommended here in anticipation of a surge related to seasonal or other flu outbreaks will be useful in helping the urgent care center prepare for many disasters.
Part of writing a clinic disaster plan is thinking of all the things that could possibly go wrong and to have a contingency plan in place. The goal is not to create a separate plan addressing every possible risk, but to create one overarching plan. For example, creating a plan that addresses pandemic influenza but not a hurricane or mass casualty situation does not make sense.
Your urgent care center needs one plan that can address all realistically imaginable disaster scenarios. Table 4 offers examples of what should be included in your disaster and pandemic plan.
Table 4. Analyzing Risks: Factors to Consider |
|
| Recent | What types of disasters, such as the flu, are occurring now in your area, or in nearby states? |
| Historical | What types of disasters have occurred recently, such as hurricanes, fires, and floods? |
| Geographic | Where is your urgent care center situated? Is it near a flood zone, power plant, nuclear plant, hazardous chemical production plant, or transportation hub (airport, train station, or freight rail)? |
| Physical | How is your urgent care constructed? Does the facility have enhanced construction, or store hazardous or biologic material? Are there proper exit and evacuation routes? Is there shelter nearby? |
| Technology | What happens if your computers crash? Do you have the ability to handwrite the details of a patient encounter? Do you have patient superbills? |
| Other | What happened if you lose electricity or a ruptured gas pipe explodes? |
A Final Word About Insurance
Make sure that your urgent care center has adequate insurance coverage to cover your losses in the event of a particular disaster, and be certain to check whether the coverage is for replacement value vs. current fair market value. Medical equipment might be old, and the actual value, factoring depreciation, may not be even close to the replacement costs for such expensive items. The same may hold true for the building itself.
As with the clinical consideration discussed earlier in this article, however, awareness coupled with preparation is the best insurance for keeping your patients healthy and your practice safe.
References
- Petric M, Comanor L, Petti CA. Role of the laboratory in diagnosis of influenza during seasonal epidemics and potential pandemics. J Infect Dis. 2006; 194 (Suppl 2): S98-110.
- Hurt AC, Alexander R, Hibbert J, et al. Performance of six influenza rapid tests in detecting human influenza in clinical specimens. J Clin Virol. 2007; 39(2): 132-135.

