Urgent message: A systematic approach to evaluating, diagnosing, and treating low back pain in the urgent care setting reduces unnecessary hospital visits, identifies red flag symptoms that warrant further diagnostic or neurosurgical evaluation, promotes returning to work quicker, and helps to reduce the number of opioid prescriptions that are prescribed for episodic exacerbation and/or chronic conditions.
Ashley Clay, MS, PA-C
Introduction
Up to 80% of the United States population experiences back pain at some point; however, most complaints resolve within 1-4 weeks without any additional treatment aside from the initial history and physical examination.1
Statistics
In the late 1990s, chronic conditions such as back pain and arthritis were being treated by opioid prescriptions; this resulted in increases in dosage and frequency. National opioid prescription rates began escalating in 2006, hitting a peak of 255 million in 20122; retail opioid prescriptions increased to 81.3 per 100 persons.2 In 2016, more than 42,000 people lost their lives to opioid overdoses; of those deaths, 40% were from prescriptions.3 According to the CDC, taking even low doses of opioid medication for greater than 3 months increases the risk of addiction 15 times2.
Anatomy
The vertebral column, whose essential functions are support, protection, and ambulation, is a flexible network of fibrocartilaginous discs and 33 vertebrae. It can be broken down into five sections:4
- Cervical (seven vertebrae)
- Thoracic (12 vertebrae)
- Lumbar (five vertebrae)
- Sacral (five vertebrae, which fuse in adults to form the sacrum)
- Coccygeal (four vertebrae, which fuse to form the coccyx after roughly 30 years)
The C7 vertebra serves as a landmark for determining the end of the cervical spine and the beginning of the thoracic region. It has the longest spinous process, is easily palpated when the neck is flexed, and results in a bony structure that protrudes out further than the others.4
The lumbar region has the largest moveable vertebrae, L5. L4-5 and L5-S1 represents the location where >90% of herniated discs occur.5 Locating the spinous processes of L4 and L5 may prove more difficult, as these are shorter than other lumbar processes.
Common Disorders
Mechanical origins constitute the most common causes of low back pain and typically involve problems with muscles, tendons, ligaments, and discs.5 Several common disorders can affect the lumbar region, including: lumbosacral strain, postural backache, lumbar degenerative disc disease (LDD), herniated disc, and spinal stenosis. Differentiation among these etiologies can be difficult with physical exam alone; however, understanding the presenting symptoms can be of value.
- Lumbar strain is often caused by strenuous work and presents as a sudden, localized pain in individuals aged 20─50 years.5 Pain is experienced during motion, but not straining or coughing. This is frequently associated with occupational twisting and lifting. On physical exam, the straight leg raise (SLR) will cause back but not leg pain; diagnostic imaging is generally not warranted.
- Postural backache is common in obese individuals and produces vague complaints that increase as the day progresses. Typically, on physical exam the patient will present neurologically intact, SLR will result in back but not leg pain, and anterior/posterior range of motion is commonly limited.5
- Degenerative changes commonly affect individuals over 50 years of age and are commonly encountered when arthritis is present in other joints.5 The pain is axial in nature, of gradual onset, worse in the morning, and does not generally radiate. X-ray evidence reveals spurring and narrowing of the disc spaces. Evidenced by autopsy reports, 80% to 90% of individuals show signs of degenerative disc disease (DDD) by age 50, and DDD is considered the most common cause of disability in those under 45 years of age.5
- Typically, herniated discs affect males more than females and cause sudden, radiating pain that may involve the buttock and leg. Pain typically radiates in the posterolateral aspect of the leg with some weakness of leg muscles. Coughing, sneezing, and hyperextension of the lumbar spine can exacerbate symptoms. Physical findings may include: asymmetrical limitation of motion, tenderness over the sciatic notch, restricted SLR, and neurologic manifestations of the lower limbs.5 When sciatica accompanies the LBP, this is often associated with a herniated disc, spinal stenosis, and chronic low back pain.
- Lumbar spinal stenosis (LSS) generally affects elderly patients and causes gradual LBP that is worse with extension due to a progressive narrowing of the spinal canal. Neurogenic claudication (pain with ambulation that is relieved with sitting) is the hallmark symptom of LSS; this pain will slowly improve following the cessation of walking.1 A distinguishing characteristic of spinal stenosis is that flexion often alleviates pain; therefore, exercises such as bicycling, which results in spinal flexion, is tolerated well by those suffering from LSS. Pain will slowly improve after cessation of walking.5
Presentation and Evaluation
Complaints of back pain warrant a review of the patient’s medical, personal, occupational, and sexual histories. During the interview, special attention should be given to any chronic back pain complaints and treatments that have previously been attempted, noting any medications, prescribing provider, and confirming opioid prescriptions by accessing the prescription drug monitoring program database.
Signs and symptoms
History should include the onset (activity performed when pain began), location (specifically addressing any radiating complaints), duration, aggravating/alleviating activities, and the character (sharp, dull, throbbing). Attention should be given to any exaggerated pain mannerisms or discrepancies on the prescription drug monitoring records to identify individuals with secondary gains and/or drug-seeking behavior.
Social and psychological histories are important aspects to obtain. Concurrent diagnoses of depression and/or chronic pain may cause variations in reported severity and findings on physical exam.5 Resolution of pain is found to be more challenging in those with concurrent mental disorders such as depression or a history of substance abuse.6 Identifying conversion disorder, depression, or psychosis as a root cause for psychogenic pain disorders often directs treatment at the source of pain and may differ from nonpsychogenic management.
Occupational history is beneficial in identifying secondary gain issues, occupational risks, and potential causes of complaints such as strenuous or heavy lifting jobs. If a work-related injury is suspected, additional documentation should include: whether complaint is new or an exacerbation, date/time of incident, witnesses to injury, action being performed, if place of employment was notified, Worker’s Compensation claim number (if available), job satisfaction rating, if personal protection equipment was utilized/available, and if focus is placed on ergonomics and job rotation.
During a thorough history and physical exam, certain findings differentiate the source of complaints. For instance, infectious processes are unlikely if the pain complaints are related to posture, activity, trauma, or if episodic presentation relieved by rest.5
Physical examination
In addition to inspection and palpation of the back, evaluate for range of motion (cervical/lumbar spine, hip joint, upper and lower extremities), gait, reflexes, strength, sensation of light touch, peripheral pulses, and nerve root testing. Nonorganic, psychogenic causes of LBP should be suspected if physical examination is out of proportion to findings. Waddell’s tests are a group of five categories that can be quickly assessed and used to identify those with underlying psychosomatic disease. If three signs are positive, follow-up is warranted.7 Positive findings do not rule out organic cause, but help identify symptom magnification and/or malingering. Waddell’s signs include:
- tenderness to light touch that is nonspecific and diffuse
- simulation tests with unexpected results
- distraction tests resulting in contradictory results
- discrepancies when testing strength and sensory
- overreaction of facial expressions7,17 (it is noted that overreaction can cause observer bias and it should be treated carefully)
The SLR is classically used to test L4, L5, and S1 nerve roots (sciatic nerve irritation) by stretching the dura. The test is performed sitting or standing by raising the leg with the knee extended to 30⁰─35⁰. When the dural attachments are inflamed, stretching of the sciatic nerve causes pain experienced in the lower leg, foot, and ankle. The SLR is considered positive when the radicular complaints are reproduced. If the patient experiences only back pain during the test, this would be considered negative. Observation of gait, heel, and toe walking proves beneficial to assess foot drop as well as motor function. Sensory, motor strength, and reflex testing help to reinforce the suspected diagnosis.
Diagnostic studies
The American College of Radiology recommends no imaging studies within the first 6 weeks unless red flag symptoms are present.1 As a general rule, imaging studies are not used to make a diagnosis but to confirm one already made based on history and physical examination findings; this is likely due, in part, to the fact that approximately 80% of LBP cases resolve within 2 weeks and 90% resolve within 6 weeks.1 For an acute presentation, plain radiographs are generally not helpful for the evaluation of nontraumatic back pain in otherwise healthy individuals between 20 and 50 years of age as discs, muscles, and ligaments are not readily visualized by radiographs. Exceptions include suspicion of infection or neoplasia.
Radiography would be useful to aid in diagnosis of compression fractures, cancer, Paget’s disease, or multiple myeloma. Magnetic resonance imaging (MRI) is the most comprehensive way to evaluate degenerative changes, detection of tumors, and the most sensitive for herniated discs, but should be delayed in lieu of conservative treatment for nonemergent presentations. In comparison, computed tomographic (CT) scans are valuable in location of herniation or tumor5 and would be acutely warranted for concerns such as compression. Lab studies such as erythrocyte sedimentation rate (ESR) and alkaline phosphate (ALP) levels should be obtained if uncommon causes LBP are suspected.5 CT or MRI studies are warranted for any patient with worsening neurological state or suspicion of a systemic illness.6
One indication for radiographs is, following a trauma, AP and lateral views should be obtained. Lumbosacral radiographs cause 20 times the dose of radiation of a chest radiograph.1 Electromyography (EMG) studies are also out of the scope of an urgent care setting; such testing should be deferred to the clinician managing chronic pain in those presenting with radiculopathy or peripheral neuropathy complaints. MRI should be reserved for those considering surgical intervention or have evidence of a systemic disease.1
An MRI is the diagnostic study of choice for anyone presenting with symptoms consistent with cauda equina syndrome, tumor, or epidural mass. An MRI should not be ordered for those believed to have a routine disk herniation, as most will improve over 4─6 weeks with conservative treatment.1
Figure 1 summarizes the prevalence of findings on MRIs in asymptomatic patients. The studies concluded that MRI findings were routinely discovered even in the absence of symptoms.8
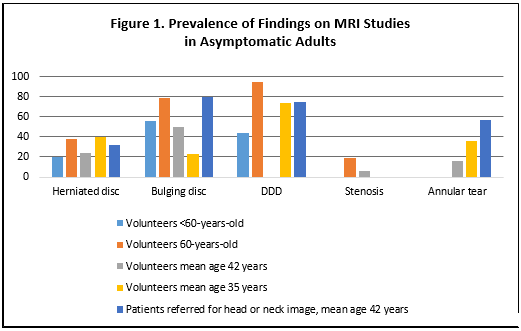
Adapted from Deyo RA, et al. N Engl J Med. 2001;344:363-370.
Another study found that 25% of asymptomatic individuals younger than 60 years of age and 33% older than 60 had MRI evidence of herniated discs.6 Asymptomatic pathology does not warrant treatment, reinforcing that MRI should be reserved for the appropriate patient. Potential issues adapted from The Agency for Health Care Policy and Research that warrant an MRI are outlined in Table 1.1
| Table 1. Potential Issues Warranting MRI | |
| Possible fracture | Major trauma Minor trauma in those <50-years Long-term corticosteroid use Osteoporosis >70 years |
| Possible tumor/infection | >50 years <20 years History of cancer Constitutional symptoms Recent bacterial infection Injection drug use Immunosuppression Supine or nocturnal pain |
Unless certain risk factors are present suggesting infection or tumor, MRIs should be reserved for those refractory to conservative measures. Indications for emergent MRI include:
- signs and symptoms consistent with cauda equina syndrome, including loss of sphincter tone, incontinence, saddle anesthesia, urinary retention, and impotence
- fever accompanied by immunosuppression
- unexplained weight loss
- history of IV drug use with concern for epidural abscess
- concern for metastatic disease, including advanced age or back pain unrelieved by rest5
Warning signs/red flag symptoms
Evaluating for “red flag” symptoms is imperative in eliminating serious etiologies such as cancer, infection, cauda equina syndrome, aneurysm, and fracture. Such symptoms include bowel and bladder dysfunction, impotency issues, loss of sphincter tone, fever, pain described as “tearing,” saddle anesthesia, progressive motor weakness, unexplained weight loss, and pain not improved with rest. Any history of intravenous drug abuse must be documented.5
Cancer and/or infection should be suspected in anyone presenting with unexplained weight loss, immunosuppression, history of IV drug abuse, age >50 years, febrile illness, or no improvement of LBP complaints with rest.
Cauda equina syndrome is a rare surgical emergency that presents with rapid progression; patients should undergo surgical intervention within 48 hours for the best outcome. Typical signs and symptoms of acute cauda equina syndrome include bowel or bladder incontinence, saddle anesthesia, weakness of the lower extremities, or acute paraplegia.
Ruptured abdominal aneurysm is another medical emergency that must be ruled out. Dizziness, “tearing” pain, or a pulsatile mass in the abdominal area may be present.9 Acute medical emergencies must be identified during the physical examination and completion of the medical history as prompt care dictates patient outcomes.
Management
Initial presentations of acute or chronic low back pain exacerbation in an urgent care setting should focus on conservative approaches unless physical examination and history suggest a serious, red flag etiology. A conservative treatment protocol should be followed for up to 6 weeks when a patient under 50 years of age presents without progressive weakness or acute constitutional symptoms. Patient education should focus on preventing re-injury, nonpharmacologic treatment options, avoidance of opioid analgesics, ergonomic discussions, management of patient expectations, and treatment of underlying psychosocial issues.
From July 2015 until August of 2016, a randomized clinical trial of 416 patients 21 to 60 years of age who presented to the emergency department with acute lower extremity pain were given a single dose of oral analgesics in order to compare opioid and nonopioid treatment outcomes. No clinically significant reduction in pain occurred at 2 hours among groups given three different opioid and acetaminophen combinations when compared with groups given only ibuprofen and acetaminophen combinations.10 This study supports the use of ibuprofen and acetaminophen combinations in lieu of opioid analgesics for acute pain in the ED setting.
| Table 2. Effective Treatment Options vs Those to Be Avoided | |
| Conservative treatment options to utilize | Treatment options with little to no value that should be avoided |
| NSAID therapy Multimodal treatment strategy Nonpharmacologic options Patient education Avoidance of opioid analgesics Ergonomic management Expectation management Avoid diagnostic studies unless trauma or “red flag” symptomology |
Opioid analgesic as first-line Single modality strategy Radiographs/diagnostic studies for nontraumatic, nonemergent Prolonged bedrest |
Adapted from Chang AK, et al. JAMA. 2017;318(17):1661-1667.
Nonpharmacologic
Nonpharmacologic options include aqua therapy, physical therapy (PT), stretching exercises, cold/hot therapy, massage, weight loss, smoking cessation, ergonomic adjustments, trigger point injections, and controlled physical activity. Cold therapy initiated within 48 hours of acute injury reduces pain and swelling while promoting peripheral vasoconstriction, resulting in increased blood flow to deeper vessels and tissues. Over time, some recommended first-line treatment modalities have been found to have little or no benefit. For example, traction is no longer recommended for lumbar radiculopathy. In the past, bed rest (controlling physical activity) would last much longer than the now 0 to 2-day recommendations. Studies confirm that prolonged bed rest results in deconditioning and muscle weakness.
A study of five healthy men found that 3 weeks of bed rest caused a decline in cardiovascular and work capacity greater than that of aging 30 years.6 The main principal behind a shortened course of bed rest is that quicker recovery is achieved by avoiding deconditioning.6 Encourage activities that do not exacerbate pain, promote maintaining function, and returning to work quickly.
Pharmacologic
The mainstay, first-line treatment for acute low back pain is nonsteroidal anti-inflammatory medications (NSAIDs) for 2-4 weeks, pending no contraindications. Any patient at risk for peptic ulcer disease should be provided gastrointestinal prophylactic medication and instruction on use.6 Cardiovascular and renal functionality should be reviewed and risks discussed prior to initiating NSAID therapy. Acetaminophen is an alternative for those who cannot tolerate NSAIDs. If NSAIDs fail to achieve adequate pain relief, a short course of systemic steroids gradually tapered may improve LBP and associated radicular symptoms.
Other pharmacologic treatment options for acute back pain include muscle relaxers and analgesics, both opioid and non-opioid types. Opioids are reserved for severe, intractable pain and treatment duration should be very short as they have a very limited role.1 Per the CDC’s 2016 recommendations, only in rare circumstances should acute pain situations require a supply of opioids >7 days; if warranted, the duration should generally not exceed 3 days.11
A study by Friedman, et al compared the efficacy of pain control and functional outcomes at 1 week in patients with nontraumatic, nonradicular acute pain by utilizing common treatment options, including naproxen, cyclobenzaprine, oxycodone/acetaminophen, or placebo. This randomized, double-blinded, three-group study was conducted in an emergency department setting on patients with pain <2 weeks duration and found no difference between those treated with naproxen alone and those treated with naproxen and oxycodone/acetaminophen.12
Muscle relaxant use is often limited secondary to sedating properties. Anticonvulsants (gabapentin or pregabalin), serotonin and norepinephrine reuptake inhibitors (SNRIs) (duloxetine and venlafaxine), and tricyclic antidepressants (TCAs) (nortriptyline and desipramine) have been recommended by several guidelines as first line medications for neuropathic pain.1,11 Other medications that may be helpful include capsaicin cream, tramadol, tapentadol, lidocaine patch, and medical cannabis strains with high levels of cannabidiol (CBD).1,15 A risk-benefit analysis should be determined with these modalities, as well, specifically in patients with history of depression or concurrent treatment for depression and the elderly population. Anticonvulsants may cause dizziness, confusion, and weight gain. All black-box warnings and assessment of suicidal ideation and serotonin syndrome need to be reviewed when initializing an antidepressant for the treatment of pain.
| Table 3. Nonpharmacologic vs Pharmacologic Options | |
| Nonpharmacologic options | Aqua or physical therapy Ice/heat therapy Massage therapy, trigger point injections, TENS unit application Stretching, ergonomic discussions, limited bed rest (modified activity) Weight loss, smoking cessation Address psychosocial issues, patient expectations |
| Pharmacologic options |
NSAIDs Muscle relaxants Systemic steroids Anticonvulsants SSNRIs vs TCAs |
Multimodal therapies are superior in reducing pain and improving function when compared with single modalities.8 Nonopioid pharmacologic treatments are generally not associated with substance-use disorders or fatal overdoses and are regarded as safer alternatives than opioid options.12
Treatment of an acute exacerbation in the urgent care setting should focus on ruling out serious causes and education to follow up with a provider managing chronic pain or primary care for referral. If considering an opioid prescription in this population, it is imperative to document the board of pharmacy results, listing the last prescription filled by chronic pain; perform a pill count of those medications that are provided by their chronic management team; and send office notes to the pain management provider so they are aware the patient is seeking treatment for pain complaints outside of their practice. If they have opioid prescriptions available, consider not providing additional medication and reinforce that they should only take their medication as prescribed.
Emergent surgical referral is warranted for a presentation consistent with cauda equina syndrome. Routine referral for surgical intervention is warranted if progressive neurologic deficit is present along with back pain that is equal to leg pain, positive SLR, evidence of a surgically amendable lesion that correlates to symptomology, and if unresponsive to conservative measures.
Chronic Low Back Pain
Pain is considered chronic when the duration is >12 weeks.6 Once the pain duration has reached the chronic classification, consider referring to a chronic pain specialist. Ideally, referral to a pain management specialist would occur at the primary care level. This allows appropriate documents to accompany the referral, including previous treatments; PT or attempts at other conservative measures; urine drug screening results; and diagnostics when available. Continuity of care is a crucial factor in management; chronic pain specialists continually review prescription monitoring programs and urine drug screens prior to and during treatment to ensure patient compliance.
Chronic pain specialists may provide management options that include lumbar epidural steroid injections (ESI) for LBP with radicular features extending below the knee (sciatica), facet joint injections for those presenting with axial spine pain accompanied with primarily radiation to the buttocks generally not past the knee, radiofrequency nerve block/ablation for facet arthropathy, trigger point injections for myofascial pain syndromes, medications (NSAIDs, APAP, tricyclic antidepressants, anticonvulsants, muscle relaxers), cognitive behavioral therapy, and implantable devices for refractory pain.
ESIs are considered after failure of more conservative approaches with NSAIDs, activity modification, and muscle relaxers. Typically, these are fluoroscopically guided transforaminal corticosteroid injections. A caudal approach may provide greater relief and easier access for the clinician in a patient with a history of lumbar spinal surgery. The usual precautions regarding steroid use should be followed, and these should be limited to three per year, generally given a few months apart. Typically, ESIs are scheduled in a series allowing 1 month between each if undergoing for the first time. If benefit is appreciated, the ESI may then be repeated and given as a “booster” injection approximately every 4 months. Benefit is variable among patients; some will have complete resolution of radicular symptoms after only 1 injection, while others may not have benefit until the series is complete, and some may experience no relief6.
Interestingly, double-blinded studies have not found repeated injections to be superior to a single injection and that relief of sciatica is short term and provides no functional improvement.1 Others argue that epidural injections have proved to be 40% effective in alleviating leg pain and may need to be repeated two times allowing 4-6 weeks to lapse before determining efficacy.6 Injection therapy remains controversial for the treatment of spinal complaints, but does appear to be a valid option for those suffering chronic LBP with radiculopathy who have failed more conservative approaches.
Surgical intervention is considered the last line of therapy for nonemergent LBP complaints and is reserved for failure of conservative modalities. It should be noted that only a small number of individuals presenting with a herniated disc require surgery. Indications for surgery vary. The most dramatic presentation of acute disc herniation resulting in surgery is cauda equine compression syndrome, and may present as loss of all neurologic function. If continued progressive neurological deficit is appreciated, it warrants close observation and early surgical intervention to reduce the risk of further impairments. Radicular features, not axial spine pain, are most often relieved by surgery. Prior to surgical consultation, discuss with the patient that while many do not experience relief of spinal pain, relief of leg symptoms can be achieved or reduced.
If surgery is not an option, or after failure of conservative and/or surgical treatments, individuals suffering from intractable pain may be candidates for implantable devices such as spinal cord stimulators (SCS) or intrathecal (IT) drug delivery systems. In the United States, 10% to 40% of patients suffer from persistent pain following lumbosacral surgery.13 A randomized cross-over study conducted at John Hopkin’s hospital found that SCS was superior to reoperation in the treatment of ongoing radiculopathy with or without concurrent low back pain in those with surgically amendable causes.13
Spinal cord stimulation remains controversial; however, the advancement of programmable options and precise epidural placement continue to support implantation. Advancements in stimulator technology have made relief of back pain achievable. Previous relief post implantation was primarily targeted to the lower extremities. Both SCS and IT systems are trialed prior to surgical implantation,13,14 allowing patients to experience the degree of relief that could potentially be obtained with placement.
Intrathecal drug delivery systems allow for a continuous infusion of medication,14 often morphine or hydromorphone (Dilaudid). Micro dosing of medication results in a lower side-effect profile and greater tolerability. After (or at times prior to) implantation, the goal is to wean from all oral opioid medication. An intrathecal catheter is connected to a reservoir typically located in the lower quadrant of the abdomen, storing and delivering medication.14 IT pumps are programmable, and dosing frequency can determine how often a pump refill is required,14 thus decreasing time between office visits. IT pumps can also provide predetermined bolus dosing delivered by the patient when exacerbation of pain is experienced. Patient education focusing on expectation management and overall quality of life should be addressed in conjunction with a psychological evaluation prior to implanting these devices. Patients or family members may mistakenly associate an IT drug delivery system as an end-of-life treatment and reassurance of rational is often warranted.
Lastly, cannabis has been utilized for medicinal purposes across the world for centuries. Now with several states legalizing both medical and recreational use, it is imperative the urgent care provider is aware of this treatment option and is knowledgeable to discuss risk─benefit. Patients will likely present questioning if medical marijuana could effectively treat their conditions. States have varying approved medical conditions (eg, multiple sclerosis, chronic pain, cancer, HIV/AIDS, neuropathic pain, spinal cord injury) and various methods of delivery (vaporization, dry leaf, ointment, patches, and so forth) for medical marijuana use.15 The endocannabinoid system regulates many biologic functions such as pain and appetite. Cannabis (marijuana) produces (exogenous) cannabinoids which mimic endogenous cannabinoids that aid in altering pain signals by suppressing sensitization and inflammation.15
As of February 2018, 29 states, the District of Columbia, Guam, and Puerto Rico allow some form of cannabis use.16 Proponents for medical cannabis in the treatment of chronic pain often cite the opioid epidemic, escalating opioid doses to achieve pain control, and resultant opioid-induced hyperalgesia (increased pain secondary to central sensitization) as a main focus for considering cannabinoid pharmacotherapy.15 Epidemiologists cite reduction in opioid prescription need with increased availability of medical cannabis programs.15
Multiple controlled studies have found cannabis to be effective for pain15; however, research to reflect long-term analgesic effect and potential adverse events is lacking. With the introduction of recreational and medical marijuana policies and programs across the country, longitudinal studies to evaluate cognitive effects with acute and chronic use, success rates of substitutability and/or supplementation from prescription opioids, and management of symptoms will become available and valuable.
Conclusion
Management of an acute on chronic exacerbation of low back pain can be challenging for the urgent care provider. It is essential to define the parameters of the symptoms, establish baseline chronic pain complaints vs variations of an acute exacerbation, list failures of previous treatment modalities, identify diversion tactics, refer chronic management to a pain provider, appropriately manage common causes of LBP, be knowledgeable of available treatment modalities, and identify any red flag symptoms that warrant further diagnostic evaluation and work-up.
Treatment recommendations have continued to evolve, and understanding current pharmacologic and nonpharmacologic options, avoiding opioid analgesics when possible, facilitating appropriate referrals, and managing expectations via patient education can promote better outcomes for this common complaint while aiding in the fight against the opioid epidemic that is occurring nationwide.
Citation: Clay A. Management of acute exacerbation of chronic low back pain in the urgent care setting. J Urgent Care Med. May 2018. Available at: https://www.jucm.com/management-of-acute-exacerbation-of-chronic-low-back-pain-in-the-urgent-care-setting/.
References
- Allegri M, Montella S, Salici F, et al. Mechanisms of low back pain: a guide for diagnosis and therapy. F1000Research. 2016;5:F1000 Faculty Rev-1530.
- S. Prescribing Rate Maps. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/drugoverdose/maps/rxrate-maps.html. Accessed January 17, 2018.
- Centers for Disease Control and Prevention. Opioid overdose. October 23, 2017. Available at: https://www.cdc.gov/drugoverdose/. Accessed April 5, 2018.
- Moore KL, Daley AF.Clinically oriented anatomy. 5th Baltimore, MD: Lippincott, Williams & Wilkins; 2006.
- Levine K. Low back pain. Cleveland Clinic Center for Continuing Education Disease Management. August 2010. Available at: http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/neurology/low-back-pain/. Accessed April 5, 2018.
- Borenstein DG, Wiesel S, Boden S. Low Back and Neck Pain Comprehensive Diagnosis and Management. Philadelphia, PA: Elsevier; 2004.
- Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491.
- Deyo RA, Weinstein JN. Primary care: low back pain. N Engl J Med. 2001;344:363-370.
- Assar AN, Zarins CK. Ruptured abdominal aortic aneurysm: a surgical emergency with many clinical presentations. Postgrad Med J. 2009;85(1003):268-273.
- Chang AK, Bijur PE, Esses D, et al. Effect of single dose of oral opioid and nonopioid analgesics on acute extremity pain in the emergency department: a randomized clinical trial. JAMA. 2017;318(17):1661-1667.
- Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. MMWR Recomm Rep. 2016;65(No. RR-1):1–49.
- Friedman BW, Dym AA, Davitt M, et al. Naproxen with cyclobenzaprine, oxycodone/acetaminophen, or placebo for treating acute low back pain: a randomized clinical trial. JAMA. 2015;314(15):1572-1580.
- North RB, Kidd DH, Farrokhi F, Piantadosi SA. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neurosurgery. 2005;56(1):98–107.
- Wilkes D. Programmable intrathecal pumps for the management of chronic pain: recommendations for improved efficiency.J Pain Res. 2014;7:571-577.
- Hill KP, Palastro MD, Johnson B, Ditre JW. Cannabis and pain: a clinical review. Cannabis and Cannabinoid Research2017;2(1):96–104.
- State Medical Marijuana Laws. National Conference of State Legislatures. Available at: http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx. Accessed March 6, 2018
- Waddell G, McCulloch JA, Kummel E, Venner RM. Nonorganic physical signs in low-back pain. Spine. 1980;5(2):117-125
Ashley Clay, MS, PA-C is Occupational Health and Wellness Clinic Coordinator/Physician Assistant, Medcor at Novartis (Alcon). The author has no relevant financial relationships with any commercial interests.

