Urgent message: Cervical necrotizing fasciitis and necrotizing mediastinitis may ultimately occur in patients presenting with symptoms of odontogenic infection. While severe illnesses rarely present in urgent care, it is important to establish a prompt diagnosis and implement rapid medical management for these patients, in order to improve survival.
Vitoria Regina Nunes Maia, MS and Lindsey E. Fish, MD
ABSTRACT
Cervical necrotizing fasciitis (CNF) is a rapidly progressive infection that can be fatal. This condition can develop from odontogenic infections that spread to the deep fascial planes of the neck, including cervical fat and muscle, resulting in necrosis. When the disease progresses into the thorax, the course is complicated by descending necrotizing mediastinitis (DNM) which carries a much higher risk for septic shock.
CASE PRESENTATION
Mr. S is a 60-year-old man who presented to the urgent care clinic with a chief complaint of sore throat and phlegm in the throat. Symptoms started 6 days earlier and were improving after getting antibiotics for presumed strep throat following a telephone visit with his primary care physician. He reported that he continued to feel like he had phlegm in his throat despite the sore throat improving. He also reported a cough with chest pain. A home COVID-19 test was negative. Patient’s wife reported that he had started to act confused the day prior to presentation. PMH includes diabetes, high cholesterol, and hypertension. Current medications included amoxicillin/clavulanic acid, dexamethasone (just completed), atorvastatin, glimepiride, linagliptin, lisinopril, metformin, and pioglitazone. The patient is a current smoker with a 40 pack-year smoking history.
Physical exam
- Vitals: T 37°C, BP 74/47, HR 74, RR 24, SpO2 90%.
- Constitutional: well-developed, no distress, fatigued
- HENT:
- Mouth – moist mucus membranes
- OP – erythematous without exudates, 1+ B tonsils
- Eyes: PERRL, EOMI
- CV: RRR nl S1, S2 no M/R/G
- Chest nl effort, no respiratory distress, bibasilar rales
- Skin: warm and dry
- Neurological: alert and oriented x 3, slow to answer questions and unable to give clear history
- Psychiatric: behavior normal, sluggish.
Due to chest pain, hypotension and confusion, an EKG was ordered (Figure 1).
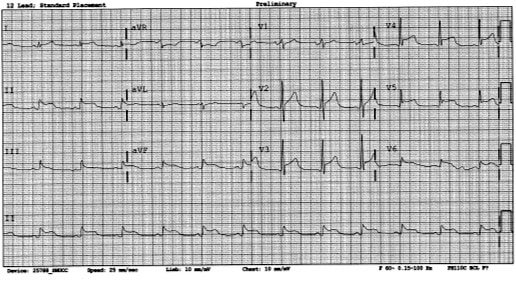
After review of the EKG by the urgent care physician, the local emergency department was notified, and the patient was transferred by ambulance emergently for presumed ST-elevation myocardial infarction. The catheterization lab was activated, and the patient received emergent cardiac catheterization which did not demonstrate an obstructive coronary artery lesion.
The patient was transferred to the medical intensive care unit (MICU) for management of hypotension. Labs in the MICU demonstrated:
- CBC: WBC 10.6, H 14.2, Hct 39.1, Pts 100
- BMP: Na 121, K 4.6, Cl 85, CO2 17, BUN 116, Cr 5.52, Glu 462, anion gap 19,
- troponin: 0.07
- BNP: 5,570
- B-hydroxybutyrate: 4.3 H
- SARS-CoV-2 PCR: Negative
- Lactate: 2.6, D-dimer: 3.16.
A chest X-ray demonstrated significant subcutaneous gas in the cervical neck and mediastinum (Figure 2).
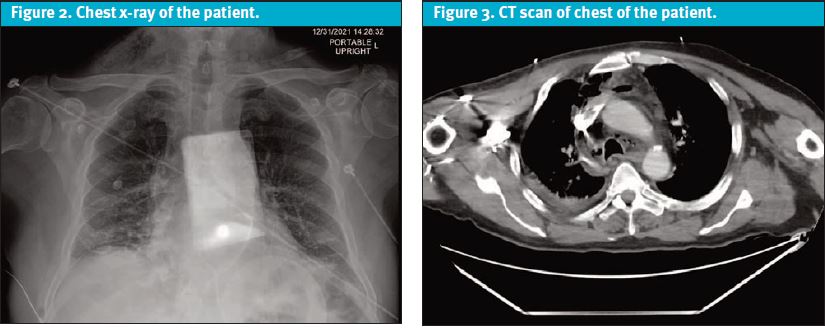
Neck exam performed following the chest x-ray: + crepitus on right.
The patient received extensive fluid resuscitation and antibiotics. Blood pressure remained low over the evening.
The CT neck and chest demonstrated findings concerning for descending necrotizing mediastinitis including fluid, fat stranding, and gas foci in the bilateral supraclavicular regions extending inferiorly into the mediastinum (Figure 3).
ENT and General Surgery were consulted, and the teams made the final diagnosis of septic shock due to necrotizing fasciitis of the neck and necrotizing mediastinitis. After obtaining further history from the patient, the presumed source was several recent dental extractions. The patient had a prolonged hospitalization with multiple surgeries and made a complete recovery.
DISCUSSION
This case presents a patient with descending necrotizing mediastinitis (DNM), a serious infection that occurs as a complication of oropharyngeal infection induced cervical necrotizing fasciitis.1,2 This can lead to septic shock with a high mortality rate and an overall poor prognosis. Cervical necrotizing fasciitis (CNF) has a described mortality rate of 7% to 20% which can reach 22% to 41% in cases where the disease extends to the thorax culminating in DNM.3
DNM limited to the area above the carina is defined as type I; that extending into the lower mediastinum is defined as type II. In this case, the patient was defined as DNM type II as the infection spread to the level of the diaphragm.
The pathologic organisms involved may be either anaerobes or aerobes. The most commonly isolated organism is beta-hemolytic oral Streptococcus (a consequence of the fact that most DNM cases are caused by odontogenic infections). Other organisms commonly found include Prevotella, Peptostreptococcus, Fusobacterium, Staphylococcus, and also alpha-hemolytic Streptococcus.4
This case highlights several key learning points. First, it is essential to obtain dental history. In the case described here, several dental extractions were performed prior to presentation. These procedures were the risk factor for DNM.
It is known that a primary odontogenic infection can spread via cervical facial layers and deep cervical infection that can result in mediastinitis. In this setting, establishing control of the upper airway and infection with tracheotomy, surgical drainage of deep cervical spaces and the mediastinum as well as intravenous broad-spectrum antibiotic therapy were required for successful treatment.5 Poor dentition and dental procedures are associated with bacteremia, endocarditis, brain abscess, and other systemic illnesses.
Additionally, this case highlights the importance of obtaining a social history including tobacco use which increases susceptibility to respiratory tract infections, including pneumonia; bacterial vaginosis and sexually transmitted diseases, such as gonorrhoea; Helicobacter pylori infection; periodontitis and postsurgical infections; and nosocomial infections. Tobacco-induced susceptibility to periodontitis is associated with shifts in the microbial composition of complex periodontal plaques.6
Furthermore, this case highlights the importance of a differential diagnosis for the patient´s hypotension. In this case, and EKG was ordered due to hypotension and that cardiac etiologies are included in the differential.
It is known that hypotension is a decrease in systemic blood pressure below accepted low values usually due to decreased effective circulating volume (hypovolemia), flow compromised due to cardiac pump dysfunction (cardiogenic), flow compromised due to cardiac obstruction (obstructive) or lack of peripheral resistance (distributive).7 It is important to understand these etiologies in order to create a differential diagnosis and establish the most appropriate treatment.
In this case, the patient was experiencing septic shock, which is a form of distributive hypotension from the deep tissue infection. Of note, the initial suspected cause of hypotension was cardiogenic in the setting of an EKG consistent with an ST-elevation myocardial infarction; however, the cardiac catheterization did not demonstrate an obstructive lesion.
This case also highlights the risk of a premature closure of diagnosis. This case occurred in the setting of the COVID-19 pandemic, which has demonstrated significant premature closure of diagnosis that resulted in many delays in recognizing and treating diseases. In the present case, the first presentation of the patient with general symptoms such as sore throat and phlegm in the throat could lead to a narrow path of diagnostic hypothesis, resulting in delay of treatment.
Of note, the PCP assumed strep throat based on a telehealth visit; COVID could also have been assumed.
Premature closure is a common type of misdiagnosis which may lead to moderate to severe harm. These errors are related specifically to taking medical histories, performing physical examinations, and ordering tests.8 Therefore, it is essential to make a broad differential diagnosis
CONCLUSION
Overall, this case highlights a rare but very severe condition that must be rapidly diagnosed if presenting in the urgent care clinic. However, lack of key clinical history and physical examination data pieces can contribute to a diagnostic challenge. The creation of a broad differential diagnosis can help to minimize the risk of premature closure. Though they may be rare, it is important to consider severe illnesses in order to establish the correct diagnosis and facilitate coordination of complex advanced medical and improve the likelihood of successful outcomes.
REFERENCES
- Sarna T, Sengupta T, Miloro M, Kolokythas A. Cervical necrotizing fasciitis with descending mediastinitis: literature review and case report. J Oral Maxillofac Surg. 2012;70(6):1342-1350.
- Abbasi Z, Inam H, Das S, et al. Fungal cervical abscess complicated by necrotizing fasciitis leading to descending necrotizing mediastinitis: a case report. Cureus. 2019;11(8):e5369.
- Nazir H, Ying Chieng C, Rogers SN, et al. Outcomes of necrotizing fasciitis in the head and neck region in the United Kingdom-a case series and literature review, Adv Oral Maxillofac Surg. 2022;6.
- Cirino AC, Mathura JR Jr, Jampol LM Resolution of activity (choroiditis and choroidal neovascularization) of chronic recurrent punctate inner choroidopathy after treatment with interferon B-1A. Retina. 2006;26(9):1091-1092.
- Fukuchi M, Suzuki O, Nasu D, et al. Descending necrotizing mediastinitis treated with tooth extractions following mediastinal and cervical drainage. Case Rep Gastroenterol. 2015;9(3):311-316.
- Bagaitkar J, Demuth DR, Scott DA. Tobacco use increases susceptibility to bacterial infection. Tob Induc Dis. 2008;4(1):12
- Sharma S, Hashmi MF, Bhattacharya PT. Hypotension. [Updated 2022 Feb 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022.
- Singh H, Giardina TD, Meyer AN, et al. Types and origins of diagnostic errors in primary care settings. JAMA Intern Med. 2013;173(6):418-425.
Author disclosures: Vitoria Regina Nunes Maia, MS, Federal University of Western Bahia, Barreiras, Bahia, Brazil. Lindsey E. Fish, MD, Denver Health and Hospital, Denver CO; University of Colorado School of Medicine, Aurora, CO.

