Published on
Urgent message: While management of infection is often guideline-dependent, studies have revealed disparities in the treatment and management of several infections among clinical sites in the United States. Current literature suggests social determinants of health and other factors may also influence treatment and management of disease states.
Derrick Murcia, BS; Ryan Loh, PhD; Omar Samara, BS; Anthony Monzon, MBA; Sterling Lee, BA; Alex Nguyen, BS; and Lindsey E. Fish, MD
Citation: Murcia D, Loh R, Samara O, Monzon A, Lee S, Nguyen A, Fish LE. Investigation of healthcare disparities in the treatment of bacterial infections: an assessment of a single urgent care clinic. J Urgent Care Med. 2023;17(4):27-35.
Key words: antibiotics, infection, disparities
ABSTRACT
Background: Treatment for infections can vary among institutions, leading to differences in patient outcomes. Despite several studies in emergency departments and primary care clinics that have identified healthcare disparities in treating infections, research is needed to verify if similar disparities exist in the urgent care setting. This study investigates a single urgent care clinic to assess for antibiotic prescribing differences in seven common bacterial infections.
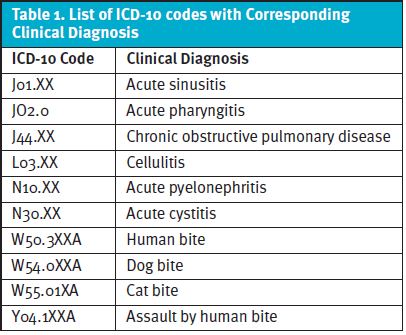
Methods: Medical records from a single urgent care clinic were screened to a set of inclusion and exclusion criteria from January 1, 2017 to December 31, 2020, using the selected ICD-10 codes. The conditions were: acute cystitis, acute pyelonephritis, bacterial sinusitis, chronic obstructive pulmonary disorder exacerbation, group A strep infections, bacterial infection secondary to bites, and cellulitis. The primary outcome was whether patients received guideline-concordant treatment. The secondary outcome was 14-day return rates following the urgent care clinic visit. Multivariable logistic models were employed to make comparisons across several demographical variables and their impact on 14-day return rates.
Results: Minimal differences were observed across guideline-concordant and guideline-discordant treatment groups. Significant differences were observed across age for bacterial sinusitis, with older patients less likely to receive guideline-concordant care. Significant differences were observed in patients diagnosed with cellulitis in that Hispanics were less likely to receive guideline-concordant treatment and older patients were more likely to receive guideline-concordant treatment. Lastly, significant differences were observed in patients diagnosed with acute cystitis in that older and non-Medicaid patients were less likely to receive guideline-concordant treatment. Fourteen-day return rates were significant in at least one demographic variable category for all infections except pyelonephritis, which did not converge.
Discussion: Research is needed to evaluate whether healthcare disparities exist in urgent care clinics. Our findings demonstrate minimal difference in the treatment of seven bacterial infections when examined for demographic variables at this single urgent care clinic. This suggests that excellent antibiotic stewardship plays a role in mitigating these types of healthcare disparities. Future investigation is needed to identify potential causes of disparities, additional ways to address those disparities, and the impact of 14-day return visits following urgent care clinic visits.
INTRODUCTION
The management of infection is largely dependent on guidelines used by the provider or hospital institution. Despite these systematic pathways, studies have demonstrated disparities in the treatment and management of several infections among clinical sites located in the United States.1–4
Current literature suggests other factors, including social determinants of health, as variables that also influence treatment and management of disease states.5–14 Overall, there are four key findings ascertained from recent studies: 1) In general, prevalence and outcomes for illness are negatively influenced by lower socioeconomic status (SES), lower-quality health insurance, and patients belonging to a minority group; 2) Hispanic and African-American patients are more likely to be seen at for-profit institutions that offer a lower quality of care for common medical conditions; 3) A concerted effort to increase access of medical care to these at-risk populations is an ideal step towards reducing disparities; 4) There is a need to integrate SES into prognostic calculations for management and treatment of illness.15
Being able to identify these disparities is the first step toward reducing those differences, with the end goal being total resolution.
While many clinical settings have been examined regarding healthcare disparities that exist within those sites, the urgent care clinic (UCC) has not been thoroughly investigated. With a better sense of which populations are most vulnerable in the urgent care setting, providers can be better equipped to give the best possible care.
The aim of this study was to investigate a single urgent care clinic to assess for antibiotic prescribing differences in seven common bacterial infections.
The data for this study came from patients treated at a single urgent care clinic associated with a large safety net urban hospital in Denver, CO. The urgent care clinic resides at the intersection of four Denver neighborhoods which have a high concentration of medically underserved populations including: 20% non-English speaking adults, 70% identifying as Latinx, 51% low-income-households, and a 20% poverty-stricken population.16 The clinic also draws patients from across the Denver metro area, therefore serving a racially, ethnically, and economically diverse population. Integration within a federally qualified heath center community health clinic allows this urgent care clinic to provide treatment to patients regardless of age, language, insurance status, or ability to pay.
On average, the urgent care clinic sees approximately 25,000 visits annually. The hospital shares many resources with the urgent care clinic, an important one being a comprehensive antibiogram, which provides guidance as to the common pathogenic bacterial infections in the community and its associated recommended susceptible antibiotics.
An example of an algorithm in the treatment of infections commonly used at institutions providing medical care is the antibiogram. These institution-specific tables depict the preferred first-line antibiotic treatment for bacterial infections based on several factors, including susceptibility, efficacy, and cost.17–19 Antibiograms are important in mitigating unnecessary expenses while also establishing systematic treatments for infections. With the development of the affiliated safety net hospital smartphone antibiogram in 2014, the application has seen increased usage over the years, including in the urgent care clinic studied. This indicates a concerted effort towards adherence to guideline-concordant treatments (ie, prescribed first-line antibiotic for infection as stated on the affiliated hospital’s antibiogram).17
Despite several studies investigating healthcare disparities, the question of whether these healthcare disparities persist in UCCs has not been investigated. We previously published a pilot study examining healthcare disparities for antibiotic prescribing for the treatment of bacterial pneumonia, which demonstrated no statistically significant differences.20 Therefore, to expand upon this, we performed a retrospective cohort study investigating whether demographic differences between guideline-concordant treatment and guideline-discordant treatment (ie, prescribed any other antibiotic) with respect to several other bacterial infections.
The infections considered here are: acute cystitis, acute pyelonephritis, bacterial sinusitis, chronic obstructive pulmonary disease exacerbation, group A strep (GAS) pharyngitis, bacterial infection secondary to bites, and cellulitis (purulent and nonpurulent). Furthermore, we used 14-day return rates to assess the impact of guideline-discordant therapies on patient outcomes.
METHODS
Study Characteristics This is a retrospective cohort study that examines provider adherence to antibiotic guidelines for patients diagnosed with bacterial infections, including acute cystitis, acute pyelonephritis, bacterial sinusitis, COPD exacerbations, GAS pharyngitis, bites complicated by bacterial infection, and cellulitis at an urgent care clinic based on diagnostic ICD-10 codes (Table 1).
Data were collected from the electronic health record for encounters at a single urgent care clinic in Denver, CO with encounters spanning the dates January 1, 2017, to December 31, 2020.
Inclusion criteria consisted of the following: adults 18 years of age or older and with one of the noted diagnoses and an associated antibiotic prescription.
Exclusion criteria consisted of the following: patients less than 18 years old, pregnant patients, patients with an allergy to guideline-concordant antibiotic, and medical records not indicating race/ethnicity, patients not prescribed an antibiotic associated with the noted diagnoses.
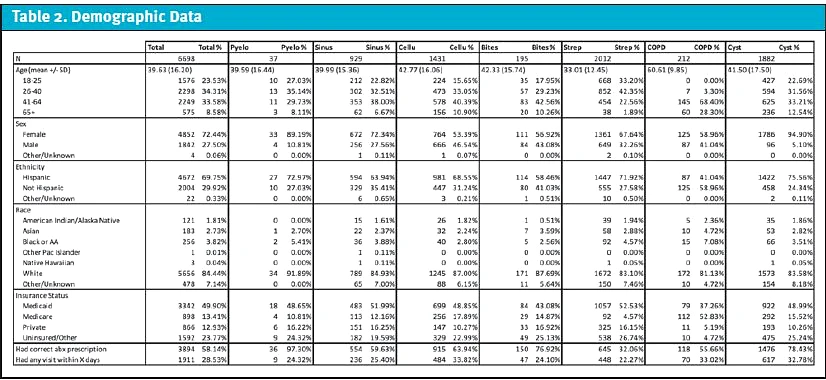
Medical records were stratified into two cohorts (guideline-concordant and guideline-discordant) and compared against different demographic variables including gender, age, race, ethnicity, and payor source (Table 2). Patients were excluded if they received a first-line antibiotic plus an additional antibiotic or no antibiotic prescription.
Absolute counts of return visits to any clinical site within the hospital and clinic system (<14 days) were also identified.
Statistical Analysis
Each data point represents one visit encounter in which someone was given a selected diagnosis. No corrections were made to account for the same individuals having multiple encounters. Data were analyzed by diagnosis (acute cystitis, acute pyelonephritis, etc.). Data were modeled independently by diagnosis as a multivariable logistic model using a logit link. Data with multiple levels (ie, race, ethnicity, payor) were converted to binary data points to reduce degrees of freedom loss and increase interpretability of odds ratios (OR) except for age which remained linear. Data analysis was performed using SAS Enterprise Guide V. 7.1 (Cary, NC). A p-value ≤ 0.05 was considered statically significant. Confidence intervals were reported with 95% confidence.
RESULTS
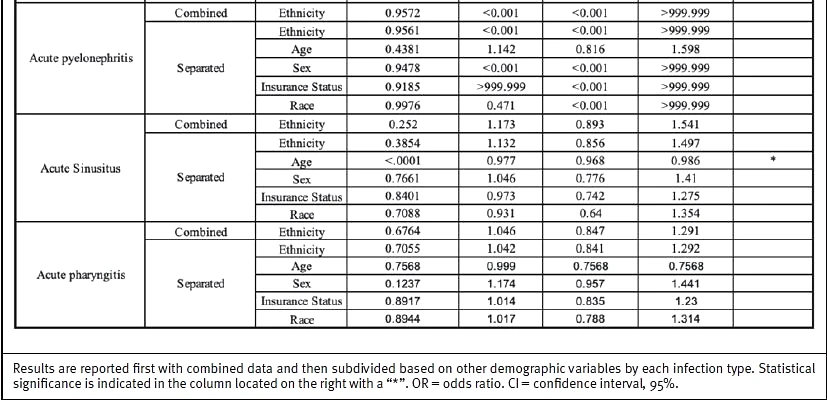
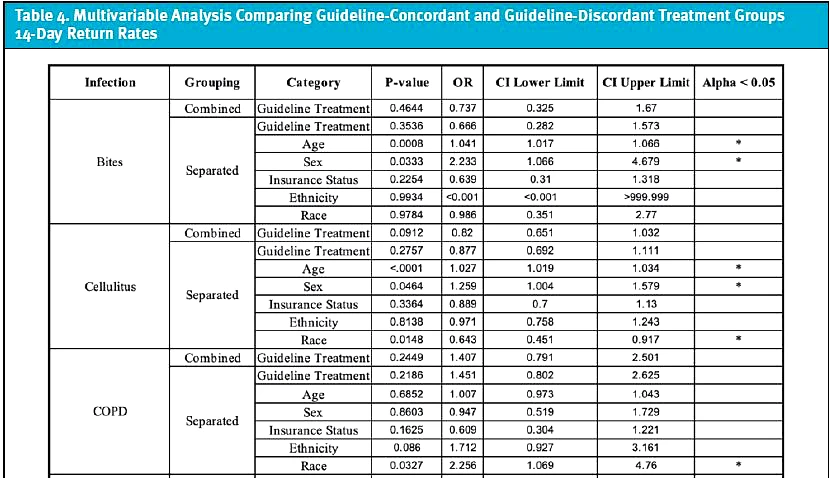
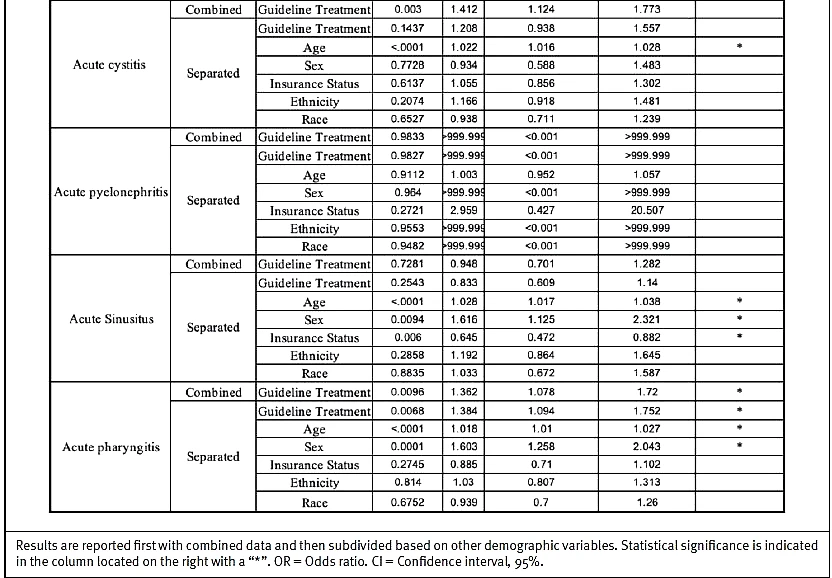
Disparities in treatment between guideline-concordant and guideline-discordant cohorts were evaluated across seven infections and compared across demographic variables. Results are reported with the primary outcome (difference between antibiotic prescribing among both treatment groups) and are then subdivided based on other possible confounding demographic variables (Table 3). Additionally, 14-day follow-up rates were compared between guideline-concordant and guideline-discordant treatment groups across seven infections, including possible confounding demographic variables (Table 4).
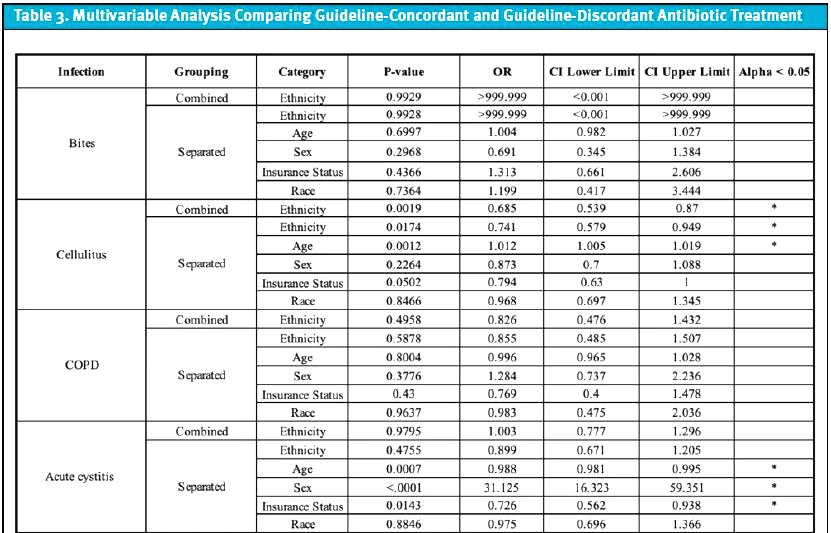
Acute Cystitis
A total of 1,882 patient visits with a primary diagnosis of acute cystitis were identified. There was not a significant difference between non-Hispanic and Hispanic patients in regard to who received guideline-concordant treatment (p = 0.9795, OR = 1.003, CI = 0.777, 1.296). When considering potential confounding factors, older (p = 0.0007, OR = 0.988, CI = 0.981, 0.995) and non-Medicaid-insured (p = 0.0143, OR = 0.726, CI = 0.562, 0.938) patients were less likely to receive guideline-concordant treatment. Female patients were more likely to receive guideline-concordant treatment (p = <.0001, OR = 31.125, CI = 16.323, 59.351). No significant differences were found when comparisons were made among race (p = 0.8846, OR = 0.975, CI = 0.696, 1.366) and ethnicity (p = 0.4755, OR = 0.899, CI = 0.671, 1.205) variables. Fourteen-day return visits were significant (p = 0.003, OR = 1.412, CI = 1.124, 1.773) with higher rates of return for guideline-discordant treatment. When considering potential confounding factors, older (p <0.0001, OR = 1.022, CI 1.016, 1.028) patients were more likely to have return visit within 14 days.
Acute Pyelonephritis
A total of 37 patient visits with a primary diagnosis of acute pyelonephritis were identified. There was not a significant difference between non-Hispanic and Hispanic patients in terms of who received guideline-concordant treatment (p = 0.9572, OR = <0.001, CI = <0.001, >999.999). When considering potential confounding factors, no significant differences were found between guideline-concordant vs discordant treatment in the following groups: ethnicity (p = 0.9561, OR = <0.001, CI = <0.001, >999.999), age (p = 0.4381, OR = 1.142, CI = 0.816, 1.598), sex (p = 0.9478, OR = <0.001, CI = <0.001, >999.999), insurance status (p = 0.9185, OR = >999.999, CI = <0.001, >999.999), and race (p = 0.9976, OR = 0.471, CI = <0.001, >999.999). There were no significant differences among 14-day follow-up visits for any groups. Of note, the logistic model for acute pyelonephritis did not converge for either outcome, as the total N was too low.
Bacterial Sinusitis
A total of 929 patient visits with a primary diagnosis of bacterial sinusitis were identified. There was not a significant difference between non-Hispanic and Hispanic patients in terms of who received guideline-concordant treatment (p = 0.252; OR = 1.173, CI = 0.893, 1.541). When considering potential confounding factors, older (p = <0.0001, OR = 0.977, CI = 0.968, 0.986) patients were less likely to receive guideline-concordant treatment. No significant differences were found when comparisons were made among the following groups: ethnicity (p = 0.3854, OR = 1.132, CI = 0.856, 1.497), sex (p = 0.7661, OR = 1.046, CI = 0.776, 1.41), insurance status (p = 0.8401, OR = 0.973, CI = 0.742, 1.275), and race (p = 0.7088, OR = 0.931, CI = 0.64, 1.354). Fourteen-day return visits demonstrated no significant difference when guideline-concordant and guideline-discordant groups were compared (p = 0.7281, OR 0.948, CI 0.701, 1.282). However, older (p = <0.0001, OR = 1.028, CI = 1.017, 1.038), female (p = 0.0094, OR = 1.616, CI = 1.125, 2.321), and Medicaid-insured (p = 0.006, OR = 0.645, CI = 0.472, 0.882) patients were more likely to have a return visit within 14 days.
Chronic Obstructive Pulmonary Disease Exacerbation
A total of 212 patient visits with a primary diagnosis of COPD exacerbation were identified. There was not a significant difference among non-Hispanic and Hispanic patients in terms of who received guideline-concordant treatment (p= 0.4958; OR = 0.826, CI = 0.476, 1.432). When considering potential confounding factors, no significant differences were found between guideline-concordant and guideline-discordant treatment in the following groups: ethnicity (p = 0.5878, OR = 0.855, CI = 0.485, 1.507), age (p = 0.8004, OR = 0.996, CI = 0.965, 1.028), sex (p = 0.3776, OR = 1.284, CI = 0.737, 2.236), insurance status (p = 0.43, OR = 0.769, CI = 0.4, 1.478), and race (p = 0.9637, OR = 0.983, CI = 0.475, 2.036). Fourteen-day return visits demonstrated no significant difference when guideline-concordant and guideline-discordant treatment groups were compared (p = 0.2449, OR 1.407, CI 0.791, 2.501). However, non-white (p = 0.0327, OR = 2.256, CI = 1.069, 4.76) patients were more likely to have a return visit within 14 days.
Group A Strep Pharyngitis
A total of 2,012 patient visits with a primary diagnosis of GAS pharyngitis were identified. There was not a significant difference among non-Hispanic and Hispanic patients in terms of who received guideline-concordant treatment (p = 0.6764; OR = 1.046, CI = 0.847, 1.291). When considering potential confounding factors, no significant differences were found between guideline-concordant vs discordant treatment in the following groups: ethnicity (p = 0.7055, OR = 1.042, CI = 0.841, 1.292), age (p = 0.7568, OR = 0.999, CI = 0.991, 1.006), sex (p = 0.1237, OR = 1.174, CI = 0.957, 1.441), insurance status (p = 0.8917, OR = 1.014, CI = 0.835, 1.23), and race (p = 0.8944, OR = 1.017, CI = 0.788, 1.314). Fourteen-day return visits demonstrated a significant different in that those who received guideline-discordant treatment (p = 0.0096, OR = 1.362, CI = 1.078, 1.72) were more likely to have a return visit within 14 days. However, older (p = <0.0001, OR = 1.018, CI = 1.01, 1.027), guideline-discordant treatment (p = 0.0068, OR = 1.384, CI = 1.094, 1.752), and female (p = 0.0001, OR = 1.603, CI = 1.258, 2.043) patients were more likely to have a return visit within 14 days.
Bacterial Infections Secondary to Bites
A total of 195 patient visits with a primary diagnosis of a bite complicated by bacterial infection were identified. There was not a significant difference among non-Hispanic and Hispanic patients in terms of who received guideline-concordant treatment (p = 0.9929, OR = >999.999, CI = <0.001, >999.999). When considering potential confounding factors, no significant differences were found between guideline-concordant and guideline-discordant treatment in the following groups: ethnicity (p = 0.9928, OR = >999.999, CI = <0.001, >999.999), age (p = 0.6997, OR = 1.004, CI = 0.982, 1.027), sex (p = 0.2968, OR = 0.691, CI = 0.345, 1.384), insurance status (p = 0.4366, OR = 1.313, CI = 0.661, 2.606), and race (p = 0.7364, OR = 1.199, CI = 0.417, 3.444). Fourteen-day return visits demonstrated no significant difference when guideline-concordant and guideline-discordant groups were compared (p= 0.4644, OR = 0.737, CI = 0.325, 1.67). However, older (p = 0.0008, OR = 1.041, CI = 1.017, 1.066) and female (p = 0.0333, OR = 2.233, CI = 1.066, 4.679) patients were more likely to have a return visit within 14 days.
Cellulitis
A total of 1,431 patient visits with a primary diagnosis of cellulitis were identified. When analyzing the combined data, Hispanic (p = 0.0019, OR = 0.685, CI = 0.539, 0.87) patients were less likely to receive the guideline-concordant treatment. When considering potential confounding potential factors, Hispanic (p = 0.0174, OR = 0.741, CI = 0.579, 0.949) and younger (p = 0.0012, OR = 1.012, CI = 1.005, 1.019) patients were less likely to receive guideline-concordant treatment. No significant differences were found when comparisons were made among the following groups: insurance status (p = 0.0502, OR = 0.794, CI = 0.63, 1), sex (p = 0.2264, OR = 0.873, CI = 0.7, 1.088) and race (p = 0.8466, OR = 0.968, CI = 0.697, 1.345). Fourteen-day return visits demonstrated no significant difference when guideline-concordant and guideline-discordant groups were compared (p = 0.0912, OR = 0.82, CI = 0.651, 1.032). However, older (p = <0.0001, OR = 1.027, CI = 1.019, 1.034), female (p = 0.0464, OR = 1.259, CI = 1.004, 1.579) and white (p = 0.0148, OR = 0.643, CI = 0.451, 0.917) patients were more likely to have a return visit within 14 days.
DISCUSSION
UCCs in the United States have demonstrated an increased growth, especially in areas that are comprised of a high population density of minority residents.21 However, other than our pilot study on antibiotic prescribing for bacterial pneumonia, no studies have investigated whether healthcare disparities in antibiotic prescribing are present in UCCs.20 Here, we implemented a rapid, systematic method to check for disparities in antibiotic prescribing across seven bacterial infections at a single urgent care clinic.
These infections were selected for two reasons: disparities in their treatment either exist in other clinical settings or have not been studied well. These seven infections are commonly seen in UCCs and are considered routine visits with which urgent care clinicians should be familiar with management and treatment options.
Overall, this retrospective study demonstrates minimal significant differences in prescribing of guideline-concordant antibiotics for seven common infections when demographic factors are identified in this single urgent care clinic. We attribute this to heavy clinical emphasis on utilization of the institution-specific antibiogram, which is easily available as a cellphone application. There were no identified differences in the treatment of acute pyelonephritis, COPD exacerbation, bacterial infection secondary to bites, and GAS pharyngitis.
Further examination of the results demonstrates the most areas of difference were in the treatment of acute cystitis and cellulitis. The difference in sex for acute cystitis was expected.
According to the antibiogram, the first-line agent for a male with cystitis is cefdinir, as this clinically qualifies as a complicated UTI. However, first-line agents for a female with cystitis are nitrofurantoin or fosfomycin, depending on age and kidney function. Therefore, we validated our methodology by using this demographic variable as a positive control.
Additional differences were seen for ethnicity in cellulitis, age in acute cystitis, bacterial sinusitis, and cellulitis, and payor source in acute cystitis. Specifically, Hispanic patients were less likely to receive guideline-concordant treatment for cellulitis; older patients were less likely to receive guideline-concordant treatment for acute cystitis and bacterial sinusitis; younger patients were less likely to receive guideline-concordant treatment for cellulitis; and non-Medicaid-insured patients were less likely to receive guideline-concordant treatment for acute cystitis. No clear pattern was identified; therefore, it is unknown why specifically these differences exist. However, this indicates that there are still areas of disparity that can be improved upon within this single urgent care clinic as providers are choosing guideline-discordant therapy at higher rates within some infections with the above identified demographic groups.
A difference in 14-day follow-up visits by at least one demographic variable was observed in all infections except for pyelonephritis, in which the data did not converge.
Older patients were more likely to have a 14-day return visit when they were seen in urgent care for bacterial infection secondary to bites, cellulitis, acute cystitis, bacterial sinusitis, and GAS pharyngitis. Some possible causes for this difference include that older patients may be more likely to have severe infections requiring follow-up, and/or older patients may access medical care more frequently due to higher medical complexity.
Female patients were more likely to have a 14-day return visit when they were seen in urgent care for bacterial infections secondary to bites, cellulitis, bacterial sinusitis, and GAS pharyngitis. Some possible causes for this difference include that female patients may have more severe infections requiring follow-up and/or female patients may be more likely to access the healthcare system.
Additionally, receiving guideline-discordant treatment was more likely to result in follow-up for patients diagnosed with GAS pharyngitis. Medicaid patients were more likely to have a follow-up visit compared with non-Medicaid patient after a visit for bacterial sinusitis. Non-white patients were more likely to have a follow-up visit compared with white patients after a visit for COPD exacerbation.
It is unclear why such differences in follow-up visits exist. Future investigation into the data is needed to determine the impact of guideline-concordant treatment as well as demographic variables or other yet-to-be-identified variables on patient follow-up and potential costs to the patient and healthcare system.
Previous studies have demonstrated that the implementation of an antimicrobial stewardship program is useful for providing systematic high-quality care while minimizing incorrect medication administration and unnecessary expenses.17–19 Given that the results demonstrate minimal differences among the guideline-concordant and guideline-discordant treatment groups, our findings suggest that the antibiogram is effective in mitigating unconscious bias when prescribing medications. In fact, these results support implementing an institution-specific antibiogram at UCCs across the United States as a means of promoting equity and minimizing disparities.
LIMITATIONS
This study contains several limitations. The first is that the data are from a single urgent care clinic site which is unique in its operational structure and patient population. The second limitation is that some conditions contain a small sample size, limiting the study’s power to identify healthcare disparities. A third limitation is that our evaluation of an urgent care is restricted to conditions that endorse clear treatment guidelines with a specific first-line recommendation. This limits our investigation towards complex conditions that could be seen at urgent care clinics or other clinical sites. A fourth limitation is that follow-up data were limited to the associated healthcare system, so follow-up to other healthcare systems is not included. Lastly, our study excluded special populations such as pediatric or pregnant patients, which limits our study’s generalizability towards these populations.
CONCLUSIONS
UCCs have recently experienced a massive growth within the United States, but few studies have analyzed data from these healthcare sites, specifically data looking at healthcare disparities. Here, we used a retrospective cohort study focused on bacterial infections to investigate for healthcare disparities. In this study, no consistent disparities were found in the treatment of bacterial infections which we attribute to excellent antibiotic stewardship and clear guidelines.
REFERENCES
- Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(1_suppl2):19-31.
- Dickman SL, Himmelstein DU, Woolhandler S. Inequality and the health-care system in the USA. Lancet. 2017;389(10077):1431-1441.
- Fiscella K, Sanders MR. Racial and ethnic disparities in the quality of health care. Annu Rev Public Health. 2016;37(1):375-394.
- Kerdemelidis M, Lennon DR, Arroll B, et al. The primary prevention of rheumatic fever. J Paediatr Child Health. 2010;46(9):534-548.
- Bergmark RW, Ishman SL, Scangas GA, et al. Socioeconomic determinants of overnight and weekend emergency department use for acute rhinosinusitis. Laryngoscope. 2015;125(11):2441-2446.
- Bergmark RW, Hoehle LP, Chyou D, et al. Association of Socioeconomic Status, Race and insurance status with chronic rhinosinusitis patient-reported outcome measures. Otolaryngol Neck Surg. 2018;158(3):571-579.
- Bergmark RW, Sedaghat AR. Presentation to emergency departments for acute rhinosinusitis: disparities in symptoms by race and insurance status. Otolaryngol Neck Surg. 2016;155(5):790-796.
- Soler ZM, Mace JC, Litvack JR, Smith TL. Chronic rhinosinusitis, race, and ethnicity. Am J Rhinol Allergy. 2012;26(2):110-116.
- Itamura K, Hur K, Ference E, et al. Characterization of chronic sinonasal disease symptoms in an urban homeless population. Am J Rhinol Allergy. 2020;34(4):494-501.
- Jha AK, Orav EJ, Li Z, Epstein AM. Concentration and quality of hospitals that care for elderly black patients. JAMA Intern Med. 2007;167(11):1177-1182.
- Jha AK, Orav EJ, Zheng J, Epstein AM. The characteristics and performance of hospitals that care for elderly hispanic Americans. Health Aff. 2008;27(2):528-537.
- Lewis SD, Peter GS, Gómez-Marín O, Bisno AL. Risk factors for recurrent lower extremity cellulitis in a U.S. veterans medical center population. Am J Med Sci. 2006;332(6):304-307.
- Yu JY, McKenna VA, Dumyati GK, et al. Antibiotic prescribing in New York State Medicare part b beneficiaries diagnosed with cystitis between 2016 and 2017. Open Forum Infect Dis. 2020;7(1):ofz544.
- Ren Z, Silverberg JI. Burden, risk factors, and infectious complications of cellulitis and erysipelas in US adults and children in the emergency department setting. J Am Acad Dermatol. 2021;84(5):1496-1503.
- Sahni S, Talwar A, Khanijo S, Talwar A. Socioeconomic status and its relationship to chronic respiratory disease. Adv Respir Med. 2017;85(2):97-108.
- Denver Metro Data: Neighborhood Summaries. Available at: https://denvermetrodata.org/neighborhoods. Accessed May 25, 2020.
- Jenkins TC, Haukoos JS, Young HL, et al. Patterns of use and perceptions of an institution-specific antibiotic stewardship application among emergency department and urgent care clinicians. Infect Control Hosp Epidemiol. 2019;41(2):212-215.
- Young HL, Shihadeh KC, Skinner AA, et al. Implementation of an institution-specific antimicrobial stewardship smartphone application. Proc Int Astron Union. 2018;39(8):986-988.
- Feiring E, Walter AB. Antimicrobial stewardship: A qualitative study of the development of national guidelines for antibiotic use in hospitals. BMC Health Serv Res. 2017;17(1):1-11.
- Murcia D, Fish L. Use of a quality improvement tool for the evaluation of healthcare disparities in urgent care: a case example for bacterial pneumonia. J Urgent Care Med. 2022;16(4):23-27.
- Le ST, Hsia RY. BMJ open community characteristics associated with where urgent care centers are located: a cross-sectional analysis. BMJ Open. 2016;6(4):1-6.
Manuscript submitted May 17, 2022; accepted July 29, 2022.
Author affiliations: Derrick Murcia, BS,University of Colorado School of Medicine, Anschutz Medical Campus. Ryan Loh, PhD,Denver Health and Hospital. Omar Samara, BS,University of Colorado School of Medicine, Anschutz Medical Campus. Anthony Monzon, MBA,University of Colorado School of Medicine, Anschutz Medical Campus. Sterling Lee, BA,University of Colorado School of Medicine, Anschutz Medical Campus. Alex Nguyen, BS,University of Colorado School of Medicine, Anschutz Medical Campus. Lindsey E. Fish, MD,Denver Health and Hospital; University of Colorado School of Medicine, Anschutz Medical Campus. The authors have no relevant financial relationships with any commercial interests.


