Urgent message: It is common for patients with injuries to the upper extremity due to falls on outstretched hands to present to urgent care. As such, evaluation, appropriate imaging, and initial treatment should all be within a clinic’s capabilities.
Michael Bartuseck, MSN, ARNP, FNP-C, EP-C
Introduction
Urgent cares centers play an integral role in providing care for patients who have sustained injuries due to falls on outstretched hands (FOOSH). While complex anatomy of the wrist, hand, and elbow often lead to confusion and misdiagnosis of FOOSH injuries, the high prevalence of these injuries makes it is imperative for urgent care providers to be proficient in diagnosis and management. Adequate treatment, follow-up, and patient education are essential to minimize risk for long-term complications. Such complications include avascular necrosis of scaphoid, scapholunate advance collapse (SLAC), and scaphoid non-advanced collapse (SNAC) wrist, as well as avascular necrosis and chronic pain. These can lead to significant morbidity and decreased quality of life.
In this article, we provide a simple and concise approach to evaluation, assessment, and treatment of common FOOSH injuries in the urgent care setting.
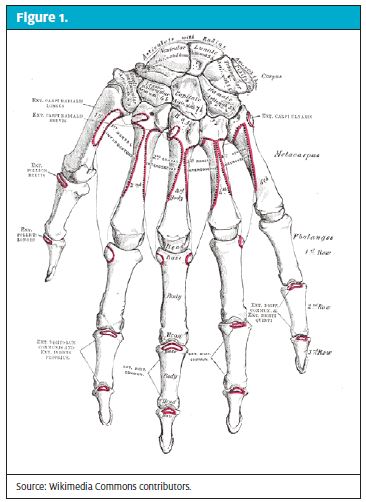
Anatomical Overview
While elbows and hands may be affected, FOOSH injuries typically impact the wrist, which is relatively complex and composed of eight carpal bones and the distal radius and ulna. Joining these bones are multiple ligaments and cartilaginous components. Our focus will be directed most at the proximal carpal row (scaphoid, lunate, triquetral), specifically the scaphoid.
Scaphoid
The scaphoid presents diagnostic challenges and can be difficult to treat, at least partly due to the fact that its vascular supply limits its ability to heal after injury. The main blood supply is retrograde, with the more proximal 70% to 80% supplied by the dorsal scaphoid branches entering along the dorsal ridge.1,2 This slow flow of blood supply makes the scaphoid prone to osteonecrosis after injury, especially of the proximal pole, which has been reported to occur in 13% to 50% of such patients regardless of treatment.2,3
Medical History
Medical history taking is greatly enhanced with attentive listening followed by focused questions to help guide examination; this is certainly never truer than when examining a patient for FOOSH injury. In such situations, history should focus on the following:
- How injury occurred: high impact, light impact, sporting event, car accident, replicating FOOSH, etc.
- Any previous falls or pertinent information regarding that extremity (osteoarthritis, surgery, previous fractures)
- Medications or illness which predispose patient to musculoskeletal injuries (eg, osteoporosis, dementia, autoimmune disorders, fluoroquinolones)
- Location of pain: ulnar, radial, volar, dorsal, elbow, hand
The inspection, which is taking place throughout the entire history, should focus on key identifiers regarding FOOSH. These include:
- Edema, ecchymosis, abrasions, lacerations, visible deformities, erythema, guarding, patient facial expressions, visible signs of distress or pain, and inspection of nonverbal cues from significant others in the room
After the inspection period, evaluate the patient’s ability regarding range of motion. There is conflicting research on performing motion on patients with injuries, as it can in some instances lead to adverse outcomes. Rather, simply asking the patient to demonstrate range of motion can aid in assessing severity and guide your next steps.
Examination, Diagnosis, and Management
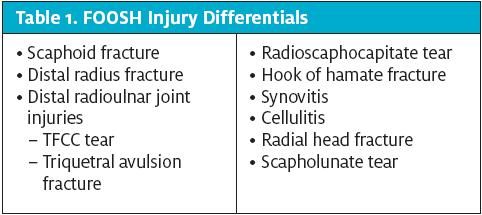
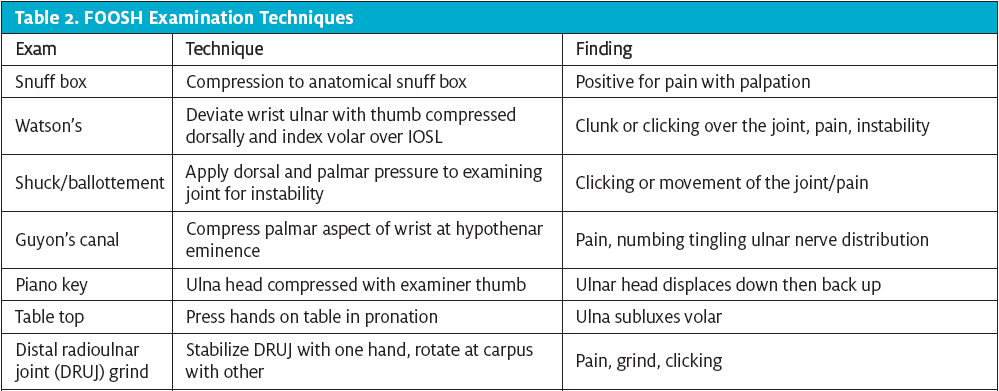
When examining a FOOSH injury (or any orthopedic injury), palpate with a purpose. It is inherent in our role as urgent care clinicians to distinguish among injuries which need immediate stabilization, injuries which need immediate consultation, and injuries that need prompt, but not immediate follow-up. It is important to consider all differentials, as it is common for more than one injury to be present after a FOOSH (Table 1; Table 2 shows examination techniques to consider).
Scaphoid Fracture
Scaphoid fractures are challenging to diagnose and treat. Patients who report radial-sided wrist pain that is either acute, subacute, or now chronic should be assessed as follows to help guide the clinician to diagnosis:
- Snuff box testing; compression of the anatomical snuff box is highly sensitive for scaphoid pathology. Should be performed on all FOOSH injuries. Pain is a positive finding4-8
- Pain on palpation of the scaphoid tubercle. The tubercle is located on the volar aspect of the wrist where the scaphoid is located radially4-8
- Thumb axial loading pressure4-8
- Thumb range of motion causing pain at wrist4-8
Diagnostic imaging to assess for scaphoid pathology should consist of multiple views; there should be a lateral, PA, oblique, and ulnar deviation. The ulnar deviation view, also known as the scaphoid view, will open up the waist of the scaphoid for easier viewing for pathology. Despite best efforts with plain imaging, >20% of acute scaphoid fractures go undetected on initial imaging.8
Management for confirmed fracture via diagnostic imaging, or even suspicion with history and examination findings as listed above, should be treated as a fracture until proven otherwise. Acute scaphoid injuries are often occult on first radiologic imaging and require further investigation in a week with an orthopedic specialist for repeat imaging. In the interim, the patient should be placed into a thumb spica splint (or short arm splint if no thumb spica is available).
It is imperative to explain the reasoning for splinting even without clear diagnosis to the patient. The explanation will help the patient understand the risk for detrimental outcomes if the scaphoid fracture is not treated properly. Those adverse effects include: avascular necrosis, osteoarthritis, chronic pain, decreased range of motion, and need for surgery. Follow-up examination with either repeat x-ray or advanced imaging with MRI or CT scan will be required.
Source: Wikimedia Commons contributors.
Distal Radius Fracture
Colles fractures are the most common type of distal radius fracture. They usually present with obvious deformity. Some however, may be more subtle and require further investigation. Palpation over the dorsal aspect of the distal radius will elicit significant pain. There will be pain with range of motion of the wrist, and it is likely the patient will decline to perform motion. Diagnostic imaging will be required. Splinting with wrist control or Colles splint is effective with prompt follow-up to an orthopedic specialist. If displacement is present, closed reduction with splinting should be performed (presuming the provider is experienced with closed reduction technique). Postreduction imaging should be obtained.
Red flag: it is imperative to assess the neurovascular components distal to the fracture. If there is any compromise, ED evaluation should be initiated. Assess for motion of the thumb as the extensor tendon (extensor pollicis longus) can be ruptured due to fracture fragments.2
Radial Styloid Fracture
Fractures of the radial styloid will typically present in a fashion similar to a fracture of the scaphoid or distal radius. Management is similar to the distal radius fracture, with splinting and orthopedic referral.
Red flag: With radial styloid fractures, also assess the scaphoid. Radial styloid fracture often present with obvious or occult scaphoid pathology. Palpation over the distal radius will elicit pain; thumb motion will also be very painful. Treat as a combination of scaphoid and radial styloid until proven otherwise.
Radial Head Fracture
Radial head fractures often occur with FOOSH injuries. Patients will complain of wrist pain, as well as elbow pain, and be hesitant to perform range of motion. However, pain with supination and pronation at the elbow is imperative for diagnosis. Palpation at the lateral aspect of the elbow will elicit pain; you also may feel crepitus at the radial head with supination pronation. X-rays should be ordered, with a minimum of two views (AP and lateral). Radial head fractures can be difficult to recognize on x-ray. Assess for a sail sign or effusion on the image. A positive fat pad sign aids in diagnosis, as well. If image is inconclusive, but exam is consistent, treat until proven otherwise.
Management should include intensive patient education. Compression wrapping for comfort and stability may be used along with a sling. Please note, early light motion is imperative for these patients, as elbow contracture and stiffness are very common after injury, possibly leading to long-term complications. These patients need to be seen by an orthopedic specialist as soon as possible to begin management. Be aware that if displacement or step-off of the radial head is present, this may require surgical intervention, and motion could worsen alignment if not managed meticulously.
Red flags: Patient follow-up is imperative, as elbow stiffness from too little movement and displacement from too much movement/lifting are common, both leading to long-term complications. In addition, remember to assess the elbow, as well, after a FOOSH.
Scapholunate Tear
Scapholunate (IOSL) injuries can occur solely or in combination with other injuries. They are often diagnosed as a simple sprain. They then continue to cause pain or discomfort in patients, causing them to seek further treatment later in life—at which point surgery to improve symptoms due to SLAC wrist or other irreversible damage will be a likely option. Tears to the scapholunate ligament alter the stability and kinematics of the wrist, causing excess stress and weakness to surrounding structures.9 SLAC and SNAC wrist are possible complications which could lead to painful osteoarthritis. Surgery is often required to reduce pain and improve function of the wrist for these patients.10
Exam findings for scapholunate tears include snuff box tenderness, dorsal wrist tenderness, visible edema, and decreased extension of the wrist. Palpation to the dorsal aspect of the wrist at the location of the scapholunate ligament often yields great discomfort. Watson’s test, which is used to assess ligament integrity, is helpful in diagnosis. Weakness of the injured wrist is often present in comparison to contralateral wrist.11
Diagnostic imaging is helpful in determining severity of a confirmed or suspected IOSL tear. Obtain standard views with consideration of closed fist view, as this view will exacerbate an IOSL tear with a widening of the joint spacing in the AP view. Management for scapholunate injury should take into account the commonality of other wrist injuries being possible. Recommendation of a wrist control splint with avoidance of lifting or exacerbating activities and early referral to an orthopedic hand specialist is imperative to avoid long-term complications.
Red flag: It is important to assess contralateral extremity in all cases of FOOSH injuries, as there may be ligament laxity that is normal for that patient. Identifying “normal” ROM for them, as well as grip strength and other findings, such as obtaining imaging bilaterally, can be helpful. Avascular necrosis to the lunate can also occur after scapholunate injury known as Kienböck’s disease.
Distal Radioulnar Joint
DRUJ consists of the articular between the distal radius and the ulna, which is boney in nature, and the triangular fibrocartilage complex (TFCC), which consists of cartilage, ligaments, and other soft tissue stabilizers. Patients with DRUJ injuries will typically complain of ulnar-sided wrist pain after a FOOSH. Often, the patient will complain of pain when lifting objects, along with clicking or a feeling of instability, and when pushing. Special examinations for ulnar-sided wrist pain include the piano key sign, grind test, and tabletop testing.12 There will be pain when the patient supinates, as injury at the TFCC can cause abnormal ulnar head motion. The patient may also have clicking and subluxation of the overlying dorsal extensor carpi ulnar tendon (ECU) as the ulna displaces dorsally in some DRUJ injuries. The TFCC is the most commonly injured structure within the DRUJ, and responsible for most of its stability.
Imaging is needed to rule out fractures, as well as assess the DRUJ joint spacing. Injuries to the triquetrum may be present, most notably as avulsion fractures. The triquetral avulsion fracture is best seen laterally in the x-ray. Patients with associated fractures and gross amount of instability and pain should be referred to orthopedic surgery promptly. Most ulnar styloid and triquetral avulsion fractures can be managed conservatively with splinting/casting. Concomitant soft tissue TFCC injuries are likely, as well. Patients with confirmed DRUJ pathology should be placed into a splint and referred to a specialist. Those without should have prompt follow-up with a primary care provider for reevaluation and possible advanced imaging and referral.
Red flag: DRUJ instability and ulnar-sided wrist pain are complex even for seasoned hand surgeons. Obtaining radiographs, assuring no obvious fracture or instability, will get the ball rolling in diagnosis. This is the essential role for the urgent care provider in patients with ulnar-sided wrist pain. Most of these issues will need advanced imaging if the patient continues to have symptoms.
Hook of Hamate
Patients who suffer numbing or tingling after a FOOSH injury along the small and fourth digit should raise suspicion for fracture of the hook of hamate. Body-of-hamate fractures are uncommon. This projection off of the hamate is in close relation to the ulnar nerve and is often fractured with FOOSH, or in sports that involve bats, sticks, or clubs. The patient will complain of ulnar-sided wrist or hand pain, weakened grip, and pain with flexion of the fifth and fourth digits in wrist ulnar deviation (hamate pull test).13 Examination will require compression of Guyon’s canal, which will elicit pain and sometimes tingling. This area is volar on the ulnar aspect of the palm and represents the area of the hook of hamate. X-ray imaging must encompass a carpal view. This makes the hook of hamate visible and easier to diagnose. Patients should be splinted and sent for reevaluation with primary care for possible advanced imaging if still symptomatic.
Red flag: Provider must obtain carpal view for accurate assessment of the hook of hamate.
Synovitis
Synovitis is inflammation of the synovial lining of a joint or of the surrounding structure of a tendon or tendinous junction. A patient may present to urgent care with painful swelling of the wrist or hand, which limits motion. Synovitis can sometimes result from FOOSH episodes or from no trauma at all. It is important to investigate potential causes of synovitis, as they are numerous. Patients who display a synovitis may have underlying arthritic or autoimmune disorders. Obtaining thorough history, as well as imaging in these patients, is helpful, as you can assess for acute injury such as fracture and for new or existing arthritis and, in some instances, infection.
Extensor tenosynovitis has a hallmark “V” pattern as swelling occurs following anatomy of extensor wrist tendon sheath. Splinting with anti-inflammatory management is appropriate with no other pathological findings, with referral to PCP for continued management.
When there is flexor tenosynovitis, it commonly occurs with infection and often affects a hand or finger. Patient will be present with swelling, erythema, and decreased range of motion. The finger will be held in slight flexion, have a gross amount of swelling, and be painful along the flexor tendon. Passive extension also will elicit severe pain.
Infective flexor tenosynovitis is an emergency. Prompt recognition and referral to the ED are paramount. Synovitis presentation should immediately raise red flags as to the underlying cause of the inflammation. Rule out infection immediately, then proceed with examination.
Red flag: Provider must recognize infection of flexor tendon sheath, as if not treated promptly this can lead to tendon rupture, skin or tendon necrosis, and loss of digit if severe enough.
Cellulitis
Patients can sometimes develop infection of the skin post FOOSH injury. Those most susceptible include the elderly or immunocompromised, as well as those who have a FOOSH in areas that may be contaminated. Patients should be examined to rule out combined musculoskeletal injury coexisting with infection. Imaging may be needed to rule out boney trauma, as well as to rule out any foreign body if wounds are present. Antibiotic treatment should then be initiated as deemed necessary, assuming no other pathology is found.
Red flag: FOOSH injuries can also accompany puncture wounds. Imaging may show foreign body. Good history taking can help decipher possible foreign body presentation.
Citation: Bartuseck M. Injuries to the upper extremity due to falls on outstretched hands (FOOSH). J Urgent Care Med. February 2018. Available at : https://www.jucm.com/injuries-upper-extremity-due-falls-outstretched-hands-foosh/.
References
- Gelberman RH, Menon J. The vascularity of the scaphoid bone. J Hand Surg Am. 1980;5(5):508-513.
- Meyer C, Chang J, Stern P, et al. Complications of distal radial and scaphoid fracture treatment. Instr Course Lect. 2014;63:113-122.
- Steinmann SP, Adams JE. Scaphoid fractures and nonunions: diagnosis and treatment. J Orthop Sci. 2006;11(4):424-431.
- Freeland P. Scaphoid tubercle tenderness: a better indicator of scaphoid fractures? Arch Emerg Med. 1989;6(1):46–50.
- Grover R. Clinical assessment of scaphoid injuries and the detection of fractures. J Hand Surg Br. 1996;21(3):341–343.
- Parvizi J, Wayman J, Kelly P, Moran CG. Combining the clinical signs improves diagnosis of scaphoid fractures: a prospective study with follow-up. J Hand Surg Br. 1998;23(3): 324–327.
- Phillips TG, Reibach AM, Slomiany WP. Diagnosis and management of scaphoid fractures. Am Fam Physician. 2004,70(5):879–884.
- Suh N, Grewal R. Controversies and best practices for acute scaphoid fracture management. J Hand Surg Eur Vol. Epub 2017 October 13.
- Mugnai R, Della Rosa N, Tarallo L. Scapholunate interosseous ligament injury in professional volleyball players. Hand Surg Rehabil. 2016;35(5):341-347.
- Andersson J. Treatment of scapholunate ligament injury: current concepts. EFORT Open Rev. 2017;2(9):382-393.
- Chim HL, Moran S. Wrist essentials: the diagnosis and management of scapholunate ligament injuries. Plast Reconstruct Surg. 2014;134(2):312e-322e.
- Thomas B, Sreekanth R. Distal radioulnar joint injuries. Indian J Orthop. 2012;46(5):493-504.
- Kadar A, Bishop A, Suchyta M, Moran S. Diagnosis and management of hook of hamate fractures. J Hand Surg Eur Vol. 2017 Jan 1:1753193417729603.