Published on
Download the article PDF: High Pressure Paint Gun Finger Injury A Case Report
Urgent Message: While the initial clinical presentation of a high-pressure paint gun injury may not elicit concern, it is truly high-risk and requires emergent recognition and surgical intervention.
Key words: High-Pressure Injection Injury, Paint Gun Injury, Finger Trauma, Pyogenic Tenosynovitis, Occupational Injury, Subcutaneous Paint Infiltration, Finger Compartment Syndrome, Finger Emergency
Abstract
Introduction: High-pressure injection injuries of the hand are rare but represent true surgical emergencies. Despite often appearing deceptively mild on initial presentation, these injuries can rapidly progress to extensive soft tissue damage, compartment syndrome, and tissue necrosis. The mechanism of injury—frequently involving industrial equipment—should immediately raise concern for deep structural involvement, even in the absence of significant pain or visible trauma. Urgent care providers must maintain a high index of suspicion when evaluating apparently benign puncture injuries with this mechanism.
Case Presentation: An 18-year-old construction laborer presented to a rural clinic 15 hours after sustaining a high-pressure paint gun injection injury to the right middle finger. Initially painless, the injury evolved over several hours with progressive swelling, erythema, and aching discomfort limiting movement of the finger. Physical exam revealed puncture wounds at the volar base of the finger, fusiform swelling, pain with passive extension, and erythema extending to the dorsal hand and wrist.
Diagnosis: Although features of Kanavel’s signs were present, the clinical concern centered on evolving compartment syndrome and extensive soft tissue injury, given the mechanism of high-pressure paint injection. Radiographs confirmed the presence of radiopaque foreign material, further supporting the need for emergent surgical management.
Case Resolution: The patient underwent surgical decompression, fasciotomy, and removal of injected material, followed by staged debridement and soft tissue reconstruction with rotational flap closure. Early surgical intervention, combined with antibiotic therapy and occupational rehabilitation, led to preservation of the digit and restoration of hand function.
Conclusion: This case illustrates the critical importance of prompt recognition and surgical referral for high-pressure injection injuries, with the mechanism of injury serving as a key diagnostic indicator. While certain physical findings may overlap with other pathologies such as flexor tenosynovitis, the risk of compartment syndrome and irreversible soft tissue injury mandates emergent evaluation. Delays in diagnosis and treatment are strongly associated with infection, tissue loss, and amputation.
Introduction
High-pressure injection injuries to the hand are uncommon but represent a true surgical emergency.[1] They frequently present to urgent care or outpatient settings with deceptively mild symptoms.[2],[3] Typically affecting working-age men engaged in industrial or maintenance work,[4],[5] these injuries result from accidental contact with high-pressure devices such as paint, grease, or hydraulic guns.2,[6] Despite appearing as small puncture wounds, high-pressure devices—often generating pressures ranging from 1,000 to over 15,000 pounds of force per square inch (psi)—can force substances deep into tissue planes, resulting in extensive and potentially devastating damage.1
Clinical severity depends on the injected material’s cytotoxicity, volume, and pressure.2 Organic solvents like paint and grease are particularly destructive, carrying amputation rates of up to 50% when surgical intervention is delayed.2,3 Even water or air, though less toxic, can cause compartment syndrome and tissue necrosis if not recognized early.1
Initial symptoms may be minimal, often leading to delayed diagnosis.[7] However, rapid progression to ischemia, infection, and necrosis can occur within hours. Urgent care providers play a crucial role in early recognition.1 Any suspected injection injury should prompt tetanus prophylaxis, intravenous antibiotics, imaging, and immediate surgical consultation. Referral within 6 hours is ideal to reduce morbidity and preserve hand function.[8]
Case Presentation
An 18-year-old right-hand dominant construction worker presented to a rural clinic 15 hours after sustaining a high-pressure paint gun injection injury to his right middle finger. While cleaning the nozzle of a paint sprayer, he inadvertently triggered a burst of paint onto his finger. Initially asymptomatic without any apparent skin lesion, he noticed swelling after 5 hours, which progressed overnight to throbbing pain and discoloration.
On exam, the right middle finger was flexed and swollen, with 2 puncture wounds (1 mm) at the volar base of the proximal phalanx. The wounds showed purple discoloration with surrounding erythema. Pain limited passive and active range of motion. Capillary refill was delayed, and sensation was reduced without signs of lymphangitis. Radiographs revealed radiopaque material in the volar soft tissue (Figure 1).
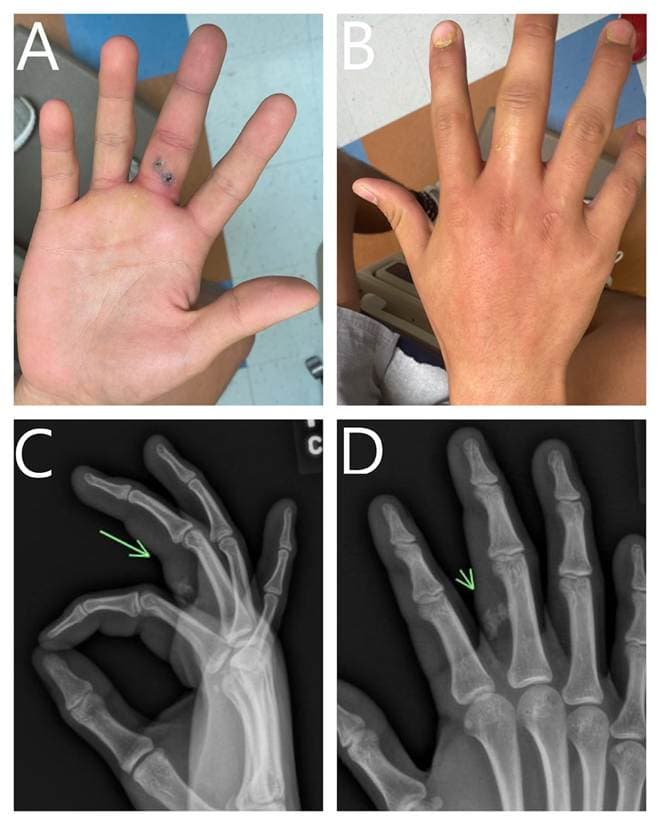
A: Small punctate entrance wounds with purple margins on the volar aspect of the right middle finger. B: Erythema extending from the dorsal hand to the wrist with dry yellow paint visible on the skin and fingernails. C, D: Lateral and anteroposterior radiographs showing radiopaque foreign material in the volar soft tissue of the middle finger.
Images courtesy of the authors.
Medical Decision Making
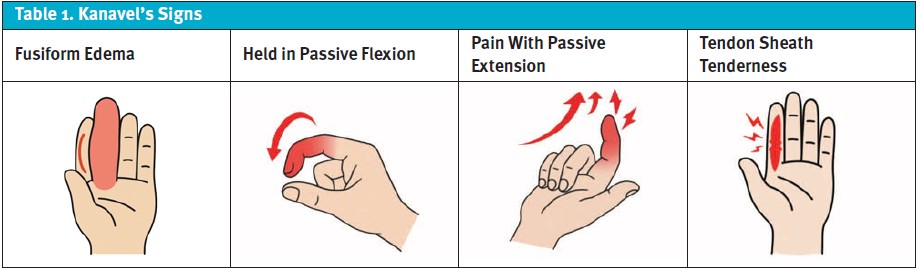
Initial concern centered on flexor tenosynovitis due to the presence of all 4 Kanavel’s signs (Table 1). However, the history of high-pressure paint exposure, delayed onset, and radiographic evidence of foreign material raised urgent suspicion for a high-pressure injection injury with possible compartment syndrome. The patient was emergently transferred to a trauma center.
| Key History Elements | Clinical Relevance | Prognostic Importance |
|---|---|---|
| Time from injury to treatment | Early recognition and referral are critical; delays can lead to progressive tissue damage and infection risk | Delays >6–10 hours are linked to increased risk of infection, necrosis, and amputation |
| Type of material injected | Organic/caustic (eg, paint, grease, solvents, oil) are cytotoxic Water and air are less harmful but not always benign | Organic/caustic: highest risk of necrosis, infection, and amputation Water: increased infection risk; delayed care increases compartment syndrome risk Air: low risk; may cause tissue emphysema |
| Volume injected | Larger volumes elevate compartment pressure and tissue disruption | Larger volumes increase risk of compartment syndrome and poor outcomes |
| Injection pressure | Higher pressure (eg, industrial sprayers) drives deeper material dispersion and soft tissue trauma | Higher pressure increases injury severity, compartment risk |
| Injury location | Fingers (especially index finger) have less tissue compliance and volume buffering | Finger injury increases risk of tissue loss due to confined anatomy compared to palm/thumb |
Differential Diagnosis and Final Diagnosis
The initial differential diagnosis included pyogenic flexor tenosynovitis, cellulitis, and retained foreign body. Emergent surgical exploration confirmed a high-pressure injection injury with retained paint, resulting in secondary compartment syndrome and flexor tenosynovitis.
Discussion
High-pressure injection injuries of the hand are rare (1 in 600 hand injuries), but carry significant risk of infection, tissue loss, and amputation, particularly if surgical debridement is delayed beyond 6 hours.1 The pathophysiology combines mechanical trauma, chemical irritation, infection, and vascular tamponade, leading rapidly to compartment syndrome and irreversible necrosis. Up to 50% of cases are initially misdiagnosed in urgent care settings because early presentations may appear deceptively benign.1,6
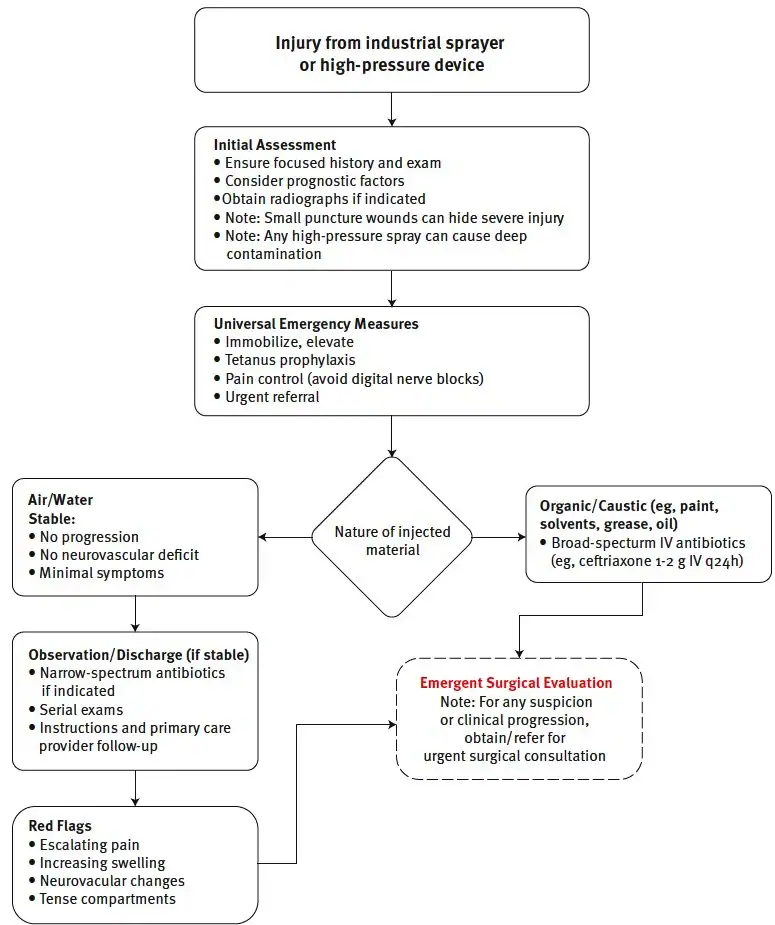
Urgent care providers should obtain a focused history to determine mechanism, material type, estimated pressure if known, time since injury (Table 2) and perform a thorough exam assessing wound size, swelling, erythema, pain with passive motion, and early signs of compartment syndrome (Figure 2). Pain out of proportion and pain with passive stretch are particularly concerning. Kanavel’s signs are not specific and may also indicate compartment syndrome or deep tissue involvement in these injuries.5,[11] Imaging with radiographs can detect radiopaque material; computed tomography (CT) or magnetic resonance imaging (MRI) may assist in complex cases, but diagnosis is primarily clinical.10
Initial management includes immobilization, elevation, tetanus prophylaxis, pain control, and empiric antibiotics. Digital nerve blocks should be avoided as they may increase compartment pressure and exacerbate ischemia in compromised tissues.1 For organic or caustic materials such as paint, solvents, or grease, broad-spectrum intravenous (IV) antibiotics are recommended (eg, ceftriaxone 1–2 g IV q24h) along with urgent surgical consultation for prompt debridement.5,10
For air or water injuries, conservative management may be appropriate if the patient is stable with no progression, no neurovascular deficit, and minimal symptoms. Narrow-spectrum antibiotics may be indicated (eg, cefazolin IV or cephalexin oral [PO] if mild and outpatient) with serial examinations to monitor for escalating pain, swelling, tense compartments, or neurovascular changes requiring urgent reassessment.6,11 Discharge with clear instructions and close primary care follow-up is essential for stable, low-risk cases. Urgent care providers play a critical role in early recognition, initial stabilization, and timely referral to prevent severe morbidity.1,6
Disposition
The patient underwent surgical decompression, debridement, and rotational flap closure, Wound cultures grew Pseudomonas, which was managed with oral antibiotics. The patient underwent 2 additional reconstructive surgeries, occupational rehabilitation, and eventually regained full hand function.
Patient Perspective
The patient expressed that he underestimated the injury and therefore delayed care. He was surprised by the emergent need for surgical treatment, and following recovery, he expressed gratitude for his care.
Ethics Statement
The patient was unable to be contacted because the contact information on record was no longer active, and therefore, demographics and some details of the case were changed to protect patient anonymity and confidentiality.
Takeaway Points
- All high-pressure injection hand injuries are surgical emergencies, regardless of initial appearance.
- Diagnosis is clinical and hinges on the mechanism of injury—always inquire about the use of high-pressure equipment.
- The type of material injected is a key prognostic factor: organic, caustic, or high-viscosity substances (eg, paint, grease, oil) are associated with higher rates of necrosis and amputation, but even air or water can cause significant morbidity and require close monitoring.
- Document both the time of injury and time of presentation, as prognosis worsens with delays to surgical intervention beyond 6 hours.
- Imaging may help identify foreign material or extent of injury but should not delay surgical evaluation.
- Initiate broad-spectrum antibiotics, tetanus prophylaxis, and pain management (avoiding digital nerve blocks) as part of initial care.
- Prompt referral for emergent surgical evaluation is essential for all cases with early and thorough debridement critical for optimal outcomes.
Manuscript submitted April 23, 2025; accepted July 7, 2025. Referen
- [1]. Cejin MC, Koyfman A, Long B. High-risk and low-incidence diseases: High-pressure injection injury. Am J Emerg Med. 2024;88:120. doi:10.1016/j.ajem.2024.11.066
- [2]. Rosenwasser MP, Wei DH. High-pressure injection injuries to the hand. J Am Acad Orthop Surg. 2014;22(1):38–45. doi:10.5435/jaaos-22-01-38
- [3]. Verhoeven N, Hierner R. High-pressure injection injury of the hand: an often underestimated trauma. Strategies Trauma Limb Reconstr. 2008;3(1):27–32. doi:10.1007/s11751-008-0029-9
- [4]. Dailiana HZ, Kotsaki D, Varitimidis S, Malizos KN. Injection injuries: seemingly minor injuries with major consequences. Injury. 2008;39(1):33–36. doi:10.1016/j.injury.2007.04.008
- [5]. Amsdell SL, Hammert WC. High-pressure injection injuries in the hand. Plast Reconstr Surg. 2013;132(4):586e–591e. doi:10.1097/PRS.0b013e31829f4bb4
- [6]. Johnson CA, Newton W, LaRochelle L, Allen J, Daly CA. High-Pressure Injection Injuries of the Hand in Community and Industrial Settings: Incidence and Trends. Hand. December 2023. doi:10.1177/15589447231218404
- [7]. Neal N, Burke FD. High-pressure injection injuries. Injury. 1991;22(6):467–470. doi:10.1016/0020-1383(91)90131-w
- [8]. Bashir K, Khan K. High-pressure injection injury: role of early detection and aggressive intervention. J Emerg Med Trauma Acute Care. 2017;2017(1):1. doi:10.5339/jemtac.2017.1
- [9]. Sharma R, John JR, Sharma RK. High-pressure chemical injection injury to the hand: usually underestimated injury with major consequences. BMJ Case Rep. 2019;12(9):e231112. doi:10.1136/bcr-2019-231112
- [10]. Vitale E, Ledda C, Adani R, et al. Management of high-pressure injection hand injuries: a multicentric, retrospective, observational study. J Clin Med. 2019;8(11):2000. doi:10.3390/jcm8112000
- [11]. Pertea M, Luca S, Benamor M, et al. High-pressure injection injury of the hand—a rare but true surgical emergency. J Clin Med. 2024;14(1):72. doi:10.3390/jcm14010072
Author Affiliations: Alejandro Bocanegra, MD, FAAFP, DABOM, Rural Health Clinic at Starr County Memorial Hospital, Rio Grande City, Texas; UTRGV School of Medicine. Daniela Santos Cantú, MD, Community Hospital in Grand Junction, Colorado. Evan D. Pérez, MD, CAQSM, UTRGV School of Medicine. Guillermo Tercero Bocanegra Hernández, MD, Unidad de Medicina Familiar 81 IMSS Coahuila, Cd. Acuña, Coahuila, México. Authors have no relevant financial relationships with any ineligible companies.
Read More
