Urgent message: Often, patients that could safely be treated for lacerations in the urgent care center are referred to the emergency room due to the quest for expediency, or even providers being out of practice with treating such wounds on site during the COVID-19 pandemic. However, doing so contributes to the degradation of acuity in urgent care while delaying care and raising costs.
Anesthesia for wound repair can be achieved in many ways, typically with injection of local anesthetics or application of topical agents directly to the wound. Direct injection into the wound has the downside of causing tissue distortion, which may affect the ability to properly align tissues. It is also painful, more so with larger lacerations. Topical anesthetics may not provide adequate or timely anesthesia.
Another method of anesthesia that may be less familiar to urgent care clinicians, nerve blocks, is effective in providing anesthesia over a large distribution with a single needle stick. It also helps limit the amount of anesthetic agent provided to avoid any toxicity concerns, especially in children and low-weight (small) patients. A high degree of familiarity with the anatomy is necessary for appropriate use, however. Figure 1 highlights the common nerves utilized. Among those with which urgent care providers should familiarize themselves:
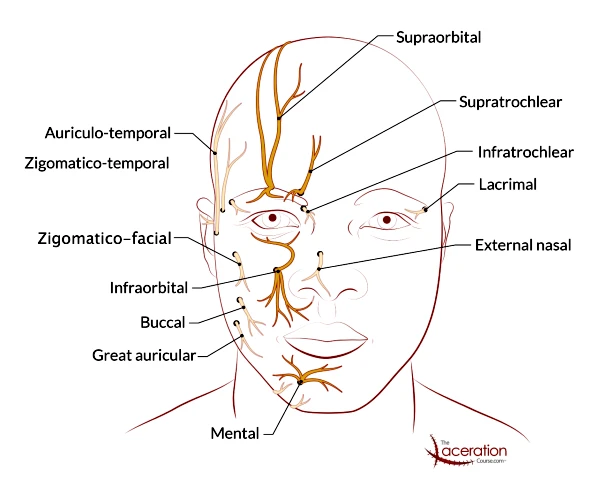
1. Supraorbital and supratrochlear nerves innervate the forehead down to the upper eyelid, to the midline. If the desired field crossed the midline, also block on the contralateral side. The supraorbital foramen can be palpated just medial to midline of the pupil, along the superior orbital rim.
After cleansing the area with alcohol, inject from a lateral approach, inserting the needle just under the lower margin of the eyebrow. It may be necessary to extend the needle medially. Aspirate to ensure you are not in a vascular space, and deposit 2 to 4 mL of anesthetic, either lidocaine or lidocaine with epinephrine, as you withdraw the needle. Make sure you are not in the foramen, as this deposit of volume can cause injury to the nerve if directly into the foramen.
2. The infraorbital nerve innervates the area overlying the midface, extending from the lower lid to the upper lip. The landmark is the infraorbital foramen, palpable externally just medial to the midline of the pupil along the inferior orbital rim.
External approach: After cleansing the area with alcohol, a single injection with the same technique as described above is used to deposit 2 to 4 mL of anesthetic, again being careful to inject into the infraorbital foramen. Pressure may be applied after administration to help diffuse into the nerve.
Intraoral approach: This may also be delivered intraorally. In fact, this is felt by many to be better tolerated than injection into the facial skin. For the intraoral approach, the landmark is the apex of the first premolar. Insert the needle into the buccal tissue near the base or root of the first premolar; angle towards the vicinity of the infraorbital foramen. Use the other hand externally to help identify and palpate the foramen. Again, deposit 2 to 4 mL of anesthetic and withdraw the needle.
3. The mental nerve exits the skull from the mental foramen, lying in line with the root of the first premolar of the mandibular teeth. This may be palpated externally in this location. The mental nerve provides sensory innervation to the lower lip down to the chin. This also lies slightly medial to the midline of the pupil. The external approach is the same as the other blocks described above. Wipe the area with an alcohol pad, insert the needle and deposit 2 to 4mL, taking care to avoid delivery into the mental foramen. The intraoral approach involves inserting the needle in the inferior buccal mucosa, aiming the needle towards the apex or root of the first premolar towards the vicinity of the mental foramen and depositing 2 to 4 mL in this area.
Application of facial nerve blocks is an important skill to be aware of, and to implement into practice. An understanding of the anatomy is key. Familiarity with the diagram above may be helpful in locating these landmarks on yourself and patients while doing a physical exam. Be mindful of pitfalls and risks—such as not injecting directly into the foramen, which may cause damage to the nerve.
RESOURCES
- Moskovitz J, Sabatino F. Regional nerve blocks of the face. Emerg Med Clin North Am. 2013;31(2):517-527.
- Salam G. Regional anesthesia for office procedures: part I. Head and neck surgeries. Am Fam Physician. 2004;69(3):585-590.
Patrick O’Malley, MD is an emergency physician at Newberry County Memorial Hospital, Newberry, SC, and the creator/owner of The Laceration Course lecture series.

