Published on
Urgent message: Establishing respiratory outpatient clinics has been shown to decrease reevaluation rates for patients with bronchiolitis, especially in children aged <12 months and/or those who receive suctioning during their initial urgent care encounter.
Prema D. Souza, MD; Aimy Patel, MD; Brian Lee, PhD; and Amanda Nedved, MD
Citation: Souza PD, Patel A, Lee B, Nedved A. Do Respiratory Outpatient Clinics Decrease Bronchiolitis Reevaluation Rates? Observational Data for a Quality Improvement Project. J Urgent Care Med. 2021;15(7):30-33.
INTRODUCTION
Bronchiolitis is a ubiquitous respiratory illness in the urgent care setting during the winter months. Children present with varying degrees of symptoms ranging from simple upper respiratory tract infection to respiratory failure requiring ventilator support.1 For those under 12 months of age, bronchiolitis is the most common cause of hospitalization,2 with approximately 100,000 admissions annually in the United States at a cost of approximately $1.73 billion.3 Of the annual readmissions for bronchiolitis, 80% are estimated to be potentially preventable.4
As infants are obligate nose breathers, nasopharyngeal secretions caused by bronchiolitis that block the nostrils may cause transient decreases in SpO2 andlead to respiratory distress.5 Suctioning of the nasopharynx to remove mucus and secretions is a common practice in both the inpatient and outpatient management of bronchiolitis. Nasal suction may be associated with an improvement in SpO2 in infants with bronchiolitis presenting to the emergency department.6 However, due to insufficient data, the American Academy of Pediatrics was unable to make a recommendation about suctioning in its most recent guidelines.7
Our institution opened its first respiratory outpatient clinic (ROC) in 2014 within one of our pediatric EDs. In 2019, the ROC model was expanded into all three metro area urgent care centers at our institution. Each ROC is staffed by a registered pediatric respiratory therapist (RT) who provides an airway assessment, suction intervention, and education. The RT also screens patients for complications of bronchiolitis that require further evaluation and management by a provider, such as dehydration, prolonged fever, or respiratory distress, and if necessary will recommend patients to one of our urgent care centers or EDs.
The impact of ROC referrals in the urgent care setting has not been evaluated. This report describes baseline ROC referral patterns. This information will identify gaps and opportunities for improving referrals with the overall aim to decrease reevaluation rates in patients discharged from the urgent care with a diagnosis of bronchiolitis.
Method
Setting
There are three freestanding pediatric urgent care centers at the authors’ institution located within a large metro area. The urgent care centers are staffed with general pediatricians and advanced-practice registered nurses who have approximately 90,000 patient encounters annually.7
Project design
Baseline data were obtained via retrospective chart review of patients discharged from the urgent care center with a diagnosis of bronchiolitis from November 1, 2018 through February 29, 2020. All children aged 8 weeks to 24 months seen at an urgent care center with a documented discharge diagnosis of bronchiolitis (ICD-10 J21.1, J21.8, J21.0, J21.9, and J84.115) as one of the top three diagnoses were included in the study. We excluded infants less than 8 weeks of age and those who were admitted or transferred from urgent care during the same visit.
Data analysis
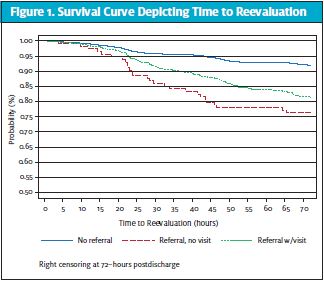
Patients were assigned to mutually exclusive groups for the analysis: A, ROC referral with visit (ROC visit group); B, ROC referral without visit (ROC referral/no visit); and C, no ROC referral. Reevaluation was defined as a documented patient encounter within the authors’ institution’s ED, urgent care center, or inpatient unit within 72 hours of discharge from the index urgent care visit. Frequency distributions of patient demographics, suction treatment during the urgent care encounter, and reevaluations were compared across the ROC groups using Pearson’s chi-square test. Nonparametric summary distributions of respiratory rate and oxygen saturation levels were calculated, and the Kruskal-Wallis test was used to compare across groups. A Kaplan-Meier survival analysis was performed to evaluate the time from urgent care encounter discharge to reevaluation for the three ROC referral groups; survival times were compared using the log-rank test for equality, and patients were right-censored after 72 hours postdischarge. Unadjusted logit models, stratified by select patient demographics (ie, patient age, gender, race, and insurance type), were used to evaluate for the presence of effect modification of the relationship between ROC referral group and reevaluations; contrasts between referral groups were adjusted for multiple comparisons. All analyses were completed using Stata (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC).
This study was deemed nonhuman subject research by the Children’s Mercy Kansas City Institutional Review Board.
Results
There were 4,034 patient encounters thatmet inclusion criteria during our study period. Of the patients in these encounters, 656 (16.3%) had an ROC visit, 114 (2.8%) had an ROC referral but no visit, and 3,264 (80.9%) had no ROC referral. Characteristics of the patient encounters are included in Table 1. The majority of patients (72%) were <12 months of age, and 59.6% were male. Patients with commercial insurance were more likely to present for a ROC visit than patients with other types of insurance. ROC referral was highest among patients who received nasopharyngeal (NP) suctioning during their index visit (28.2%). Patients who received no suctioning during the index visit were least likely to visit the ROC following their index visit (5.9%) (p <0.001). The median respiratory rate at the index visit differed across groups (p <0.001) and was highest among patients with a ROC visit (group A, 44 breaths per minute; interquartile range: 36, 52). Oxygen saturation, however, was not significantly different among the three groups, with a median of 98% in all groups.
Reevaluation within 72 hours occurred in 415 (10.3%) of the encounters. Among these reevaluations, 220 (53.0%) occurred in the urgent care sites, 122 (29.4%) in the ED, and 73 (17.6%) resulted in patient admission. Seventy-eight percent of those reevaluated were under the age of 12 months. Additionally, 12.8% of patients who received NP suctioning were reevaluated, compared with 10.4% of patients receiving NA suctioning and 6% of those who received no suctioning. Only 17.4% of patients who were reevaluated were admitted to an inpatient unit (Table 2).
Table 1. Patient Demographics and Referral Type
| ROC visit | ROC referral, no visit | No referral | p-value | |
| Age (months) 0.0-3.99 months 4.0-7.99 months 8.0-11.99 months 12.0-15.99 months 16.0-19.99 months 20.0-23.99 months | 107(15.9%) 291(21.6%) 139(15.7%) 74(13.2%) 28(7.7%) 17(8.3%) | 30(4.5%) 43(3.2%) 24(2.7%) 9(1.6%) 4(1.1%) 4(1.9%) | 537(79.7%) 1013(75.2) 722(81.6%) 476(85.2%) 331(91.2%) 185(89.8%) | <0.0001 |
| Gender Female Male | 264(16.2%) 392(16.3%) | 49(3.0%) 65(2.7%) | 1316(80.8%) 1948(81.0%) | 0.848 |
| Race American Indian or Alaska Native Asian Black or African American Declined/refused Hispanic Multiracial Native Hawaiian or Pacific Islander Other Respondent not available Unknown to respondent White Blank | 0(0.0%) 9(12.0%) 58(11.8%) 7(15.6%) 34(13.9%) 53(16.0%) 0(0.0%) 10(15.4%) 0(0.0%) 0(0.0%) 485(17.8%) 5 | 0(0.0%) 8(10.7%) 14(2.8%) 1(2.2%) 6(2.5%) 10(3.0%) 1(4.0%) 2(3.1%) 1(8.3%) 0(0.0%) 71(2.6%) | 9 (100.0%) 58 (77.3%) 420 (85.4%) 37 (82.2%) 204 (83.6%) 268 (81.0%) 24 (96.0%) 53 (81.5%) 11 (91.7%) 13 (100.0%) 2,162 (79.5%) | 0.001 |
| Insurance type Commercial Medicaid Other Self-pay Unknown | 413 (21.4%) 212 (13.8%) 13 (19.4%) 16 (7.9%) 2 (0.7%) | 63 (3.3%) 47 (3.1%) 0 (0.0%) 2 (1.0%) 2 (0.7%) | 1455 (75.3%) 1278 (83.1%) 54 (80.6%) 184 (91.1%) 293 (98.7%) | <0.0001 |
| Referral Location BV Urgent Care EC Urgent Care NC Urgent Care | 285 (20.1%) 229 (14.0%) 142 (14.6%) | 43 (3.0%) 45 (2.7%) 26 (2.7%) | 1092 (76.9%) 1367 (83.3%) 805 (82.7%) | <0.0001 |
| Suction treatment in UC Nasopharyngeal suction Nasal aspirator No suction | 42 (4.9%) 350 (24.4%) 264 (15.2%) | 9 (1.0%) 54 (3.8%) 51 (2.9%) | 810 (94.1%) 1031 (71.8%) 1423 (81.9%) | <0.0001 |
| Vitals Respiratory rate SpO2 | 44 (36,52) 98 (97,100) | 40 (33,48) 98 (97,100) | 40 (32,48) 98 (97,99) | 0.0001 0.6594 |
The rate of reevaluations was highest for patients who received a referral but no ROC visit (23.7%). Patients with no ROC referral had the lowest rate of reevaluation (8.1%). The follow-up time to reevaluations differed across groups (p-value <0.001), with patients who received a ROC referral but no visit having the shortest time to reevaluation. Patients without an ROC referral had the longest time to reevaluation (Figure 1).
DISCUSSION
In our study, most patients who received an ROC referral visited the ROC at least one time during the referral period. ROC visits were associated with longer duration between index visit and reevaluation, as well as an overall decrease in reevaluation rates for encounters in which an ROC referral was provided.
Although suctioning was associated with increased ROC referral, 77% of patients for whom suctioning at the urgent care was ordered did not receive an ROC referral. Patients who received NP suctioning at the index visit and were <12 months of age were more likely to receive an ROC referral; however, they were also more likely to be reevaluated. These data suggest that encounters for patients who are <12 months or receive suctioning at the index visit are more likely to be reevaluated during their bronchiolitis illness. These patients may benefit the most from an ROC referral when available.
Clinical research on suctioning in bronchiolitis is limited,8 but our preliminary data suggest that ROC referrals can reduce reevaluation. This study supports previous findings that early interventions can mitigate the risk of prolonged hospitalization in bronchiolitis and reduce the rate of reevaluation.9 Patients for whom an ROC referral was ordered but no ROC visit was recorded were more likely to be reevaluated and had the shortest duration of time between the index visit and reevaluation. Patients who did not receive a referral were the least likely to require reevaluation within 72 hours. This finding is probably related to a selection bias, as those patients may have had a milder degree of illness. However, some patients in this group were reevaluated. Providing an ROC referral to eligible patients, regardless of illness severity at the index visit, may further decrease the frequency of reevaluation in the urgent care center or ED.
Table 2. Reevaluation rates by patient demographics and referral type
| ROC visit | ROC referral, no visit | No referral | p-value | |
| Overall | 123 (18.7%) | 27 (23.7%) | 265 (8.1%) | <0.001 |
| Age (in months) 0.0-3.99 months 4.0-7.99 months 8.0-11.99 months 12.0-15.99 months 16.0-19.99 months 20.0-23.99 months | 27 (25.2%) 50 (17.2%) 28 (20.1%) 13 (17.6%) 3 (10.7%) 2 (11.8%) | 6 (20.0%) 13 (30.2%) 3 (12.5%) 2 (22.2%) 2 (50.0%) 1 (25.0%) | 65 (12.1%) 74 (7.3%) 58 (8.0%) 36 (7.6%) 21 (6.3%) 11 (5.9%) | 0.002 <0.001 <0.001 0.008 0.015 0.106 |
| Gender Female Male | 52 (19.7%) 71 (18.1%) | 15 (30.6%) 12 (18.5%) | 104 (7.9%) 161 (8.3%) | <0.001 <0.001 |
| Race American Indian or Alaska Native Asian Black or African-American Declined/refused Hispanic Multiracial Native Hawaiian or Pacific Islander Other Respondent not available Unknown to respondent White Blank | 1 (11.1%) 10 (17.2%) 1 (14.3%) 8 (23.5%) 8 (15.1%) 3 (30.0%) 92 (19.0%) | 2 (25.0%) 1 (7.1%) 0 (0.0%) 0 (0.0%) 5 (50.0%) 0 (0.0%) 0 (0.0%) 0 (0.0%) 19 (26.8%) | 0 (0.0%) 5 (8.6%) 26 (6.2%) 3 (8.1%) 19 (9.3%) 24 (9.0%) 2 (8.3%) 3 (5.7%) 0 (0.0%) 0 (0.0%) 183 (8.5%) 0 (0.0%) | —— 0.246 0.013 0.557 0.056 0.001 0.999 0.075 —— —— <0.001 —— |
| Insurance type Commercial Medicaid Other Self-pay Unknown | 71 (17.2%) 48 (22.6%) 3 (23.1%) 1 (6.3%) 0 (0.0%) | 14 (22.2%) 12 (25.5%) 1 (50.0%) 0 (0.0%) | 132 (9.1%) 115 (9.0%) 3 (5.6%) 12 (6.5%) 3 (1.0%) | <0.001 <0.001 0.082 0.149 0.999 |
| Referral Location BV Urgent Care EC Urgent Care NC Urgent Care | 56 (19.6%) 42 (18.3%) 25 (17.6%) | 10 (23.3%) 10 (22.2%) 7 (26.9%) | 82 (7.5%) 117 (8.6%) 66 (8.2%) | <0.001 <0.001 <0.001 |
| Suction treatment in UC No suction Nasopharyngeal suction Nasal aspirator | 5 (11.9%) 65 (18.6%) 53 (20.1%) | 1 (11.1%) 11 (20.4%) 15(29.4%) | 46 (5.7%) 107 (10.4%) 112 (7.9%) | 0.129 <0.001 <0.001 |
Limitations
Our study is limited by its retrospective design. There is significant variation in diagnostic labeling of patients with lower respiratory tract infection,10 and the data set is entirely dependent on the diagnoses chosen by the treating providers. Because this is a single-center study, results may not be generalizable to all care settings. It is likely that this study population is a representative sample with rates of repeat hospitalization similar to those found in real practice. Patients were not eligible for ROC referral if they had chronic pulmonary conditions, such as chronic aspiration or cystic fibrosis; airway abnormalities, such as cleft palate, choanal atresia, or laryngomalacia; cardiac history, such as cyanotic heart disease; or home medical device use, such as nasogastric tube or gastrostomy tube. However, due to the complexity of identifying these patients, they were not excluded from the study.
CONCLUSION
The ROC is a novel care model for the medical neighborhood to provide supportive management of bronchiolitis in a timely manner. Our baseline data suggest that ROC referrals decrease the rate of reevaluation to the urgent care center or ED in patients who receive the referral at the index visit. These preliminary data will be used to improve ROC referral rates for patients with bronchiolitis. Future Plan-Do-Study-Act cycles will focus on encouraging ROC referrals in eligible encounters regardless of illness severity.
References
- Lambert L, Sagfors AM, Openshaw PJ, Culley FJ. Immunity to RSV in early-life. Front Immunol. 2014;5:466.
- Hasegawa K, Tsugawa Y, Brown DF, et al. Trends in bronchiolitis hospitalizations in the United States 2000-2009. Pediatrics. 2013; 132(1):28-36.
- Hall CB, Weinberg GA, Blumkin AK, et al. Respiratory syncytial virus-associated hospitalization among children less than 24 months of age. Pediatrics. 2013; 132(2):e341-348.
- Gay JC, Agrawal R, Auger KA. Rates and impact of potentially preventable readmissions at children’s hospitals. J Pediatr. 2015;166(3):613-619.e5.
- Piedimonte G, Perez MK. Respiratory syncytial virus and bronchiolitis. Pediatr Rev. 2014; 35(12);519-530.
- Moschino L, Mario F, Carraro S. Is nasal suctioning warranted before measuring O2 saturation in infants with bronchiolitis? Arch Dis Child. 2016;101(7):114-115.
- Children’s Mercy Kansas City. Annual Report 2017. Available at: https://www.childrensmercy.org/siteassets/media-documents-for-depts-section/documents-for-about-us/quality-and-safety/annual-report.pdf. Accessed March 8, 2021.
- Ralston SL, Lieberthal AS, Meissner HC, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014;134(5):e1474-e1502.
- Weisgerber MC, Lye PS, Li SH, et al. Factors predicting prolonged hospital stay for infants with bronchiolitis. J Hosp Med. 2011;6(5):264-270.
- Mansbach JM, Espinola JA, Macias CG, et al. Variability in the diagnostic labeling of nonbacterial lower respiratory tract infections: a multicenter study of children who presented to the emergency department. Pediatrics. 2009;123(4):e573-e581.
Author affiliations: Prema D. Souza, MD, Children’s Hospital, Kansas City, MO,University of Missouri Kansas City School of Medicine’ Aimy Patel, MD, Children’s Hospital, Kansas City, MO,University of Missouri Kansas City School of Medicine; Brian Lee, PhD, Children’s Hospital, Kansas City, MO; Amanda Nedved, MD, Children’s Hospital, Kansas City, MO, University of Missouri Kansas City School of Medicine. The authors have no relevant financial relationships with any commercial interests.
Read More Original Research Articles
- COVID-19 Is Not Only Surging–It’s Striking More Children Than Ever
- Urgent Care Provider Awareness Of The Canadian Computed Tomography Head Rule: A Descriptive Cross-Sectional Survey Study
- Original Research: HIV Screening In The Urgent Care Setting
