Andrew Alaya MD MSc
Urgent Message: Abdominal pain is a common urgent care complaint that may result from a variety of benign to life-threatening etiologies, which can pose diagnostic and therapeutic difficulty for the clinician. Ureteral calculi are able to be diagnosed and managed in the urgent care setting.
Citation: Alaya A. Detection and Management of Urinary Calculi in the Urgent Care Setting. J Urgent Care Med. 2023;18(2); 31-38
Introduction/Epidemiology
Formation of calculi in the urinary system (ie, nephrolithiasis) is a very common issue. The propensity for urinary stone formation is a metabolic disease caused by various exogenous and endogenous factors and is often hereditary.
Urinary calculi (ie, stones) may be asymptomatic, however, many patients experience severe pain, hematuria, and vomiting. The prevalence of urinary calculi has been increasing globally and presently affects an estimated 5–15% of the world’s population.[1] In the United States, for example, prevalence has more than doubled in the last two decades. The lifetime risk of symptomatic urinary stones is approximately 13% in men and 7% in women.1 The prevalence is highest in older Caucasian males and lowest among African American females.[2] Symptomatic passage or uroliths occurs most frequently during warmer months.2
Urinary calculus formation is frequently chronic with an estimated 50% risk of recurrence.2 Risk factors for recurrent nephrolithiasis include a positive family history, dietary factors such as low intake of water, increased intake of animal protein, sodium, and underlying medical conditions, such as hyperparathyroidism.2
Urinary calculi are among the most economically impactful urologic conditions for direct and indirect costs, such as missed work days and temporary disability due to the pain.[3] More than 70% of urinary calculi are diagnosed by the use of computerized tomography (CT) scan currently, which has added further expense associated with nephrolithiasis.[4]
The experience of severe pain often results in emergency department (ED) presentation. However, in recent years the number of visits to urgent care (UC) centers due to urinary calculi has also increased. While not specifically studied, it’s likely that UC presentations for ureterolithiasis have also increased because of growing number of UC centers in the US. Therefore, it is increasingly important for UC clinicians to be familiar with initial diagnosis and management of urinary calculi as well as appropriate referral practices for follow-up and possible urologic intervention.
This article will outline the basics of different imaging modalities, their sensitivity and specificity for detection of caculi in the urinary system, advantages, disadvantages, and cost considerations. The article will synthesize clinical guideline recommendations from three organizations: the American Urological Association (AUA), European Association of Urology (EAU) and the American College of Radiology (ACR).
Clinical Presentation and Pathophysiology
Clinical presentation of patients suffering with urinary calculi is typically with “renal colic,” or severe flank pain, radiating to the groin when stone passage from the kidney to the ureter occurs. Nausea and vomiting may also occur. Dysuria and frequency of micturition are common, particularly when the stone progresses to the lower urinary tract or there is co-existent infection.3 Microscopic or gross hematuria is usually present and renal angle tenderness may be elicited on examination.3
Urinary calculi are most often asymptomatic when they are growing in the renal calyces. However, when stones become dislodged and pass into the ureter, they can obstruct the flow of urine, which leads to hydronephrosis.[5] As the ureteral peristalsis encounters the obstruction, intense waves of intermittent, visceral pain results which is termed “renal colic.”5 Flank pain, nausea, vomiting and hematuria are often associated with these severe bouts of pain.5
The diagnosis and location of kidney calculi may often be anticipated without imaging modalities but is based on patients’ history and physical examination. When the calculus causes obstruction approximately at the ureteropelvic junction (UPJ), it often causes pain radiating to the flank. If the ureterolith manages to pass through the first part of the ureter it commonly next will lodge at the distal part of the ureter, referred to as ureterovesical junction (UVJ). The UVJ region has two points of narrowing, one at the intersection across the iliac vessels and the other entering the bladder. In the former narrowing, obstruction causes pain radiating down into the groin of lower abdomen. In latter narrowing, obstruction causes pain radiating into the scrotum or labia, inner thigh or urethra and often creates urinary frequency, urgency, and dysuria as the calculus irritates the urinary bladder.5
Although patients presenting to the UC center with flank pain and hematuria are likely to have urinary calculi, even if a clinical estimation of the location of the stone can be made, abdominal imaging is still considered appropriate as part of the initial workup with severe/active symptoms.4 A wide differential diagnosis is still advisable for patients with severe abdominal and/or flank pain, especially if older or without known history of nephrolithiasis.
Role of Imaging
Imaging considerations are central to the evaluation for suspected urinary calculi. Imaging may confirm diagnosis or demonstrate alternate diagnoses. If ureterolithiasis is identified, clinicians may stratify the likelihood of spontaneous calculus passage without intervention based on the calculus size and location.[6] The likelihood of stone passage is multifactorial and the probability of spontaneous passage decreases with larger size and improves when located more distally in the ureter.6 Pain is not always a reliable marker, as pain may vary and even resolve completely despite continued obstruction from the stone. Persistence of the asymptomatic obstruction can occur and lead to permanent loss of renal function. This is the justification for why imaging is generally recommended when a stone is suspected to have been passed, but the patient has not actually seen the stone.6
Urinary Calculi in Pregnancy
The urinary tract undergoes certain anatomical and physiologic changes during pregnancy that may increase the risk of development of urinary calculi. In pregnancy, ureterolithiasis is the most common cause of abdominal pain related to the urinary system.[7] The increased progesterone associated with pregnancy increases smooth muscle relaxation and reduces peristalsis in the ureter. The enlarging gravid uterus compresses the ureter, especially later in pregnancy. Gestational hydronephrosis occurs in 90% of pregnant women beginning from 6 to 11 weeks of pregnancy and resolving by 4 to 6 weeks after delivery. The right side is generally more dilated than the left, possibly as a result of dextro-rotation of the uterus, and the protective effect of the sigmoid colon over the left ureter. However, the incidence of renal calculi in pregnancy is quoted to be 1 in 1,500, which is similar to non-pregnant women.[8]
Urinary calculi may present with similar symptoms as other acute conditions such as appendicitis, diverticulitis and even placental abruption, thereby leading to misdiagnosis and delays in appropriate treatment.8 Calculi appear to be more common in multiparous women and in the later stages of pregnancy, with 80–90% of calculi occurring in the second and third trimester. Ureteral calculi are encountered equally on the right and left side among pregnant patients despite greater dilatation of the right renal tract.7 The incidence rates of recurrent urinary calculi is up to 50%.8
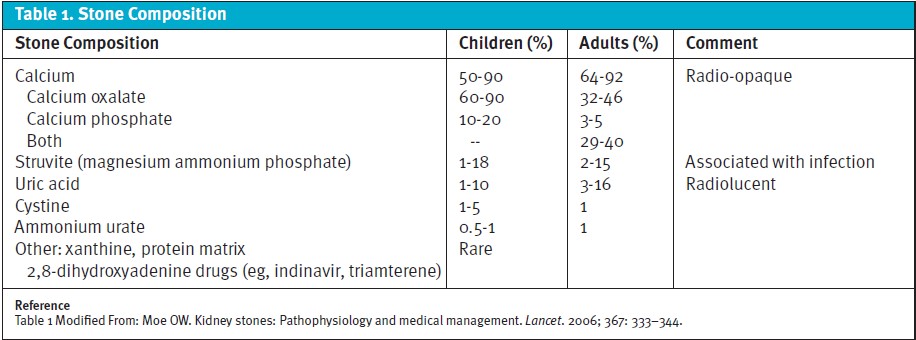
Calcium stones account for over 80% of calculi in the general population (see Table 1). They are also the most common calculi found in pregnancy. However, up to 74% of pregnant patients with nephrolithiasis have calcium phosphate calculi, in contrast to the general population, where calcium oxalate is more common. This is thought to be secondary to the renal excretory changes and the higher pH of urine in pregnancy.6
Diagnosis
Laboratory Assessment
Urinalysis (UA) is a critical test in the evaluation of potential urinary calculi. UA can offer clues to the diagnosis of urinary calculi and is critical for excluding concurrent infection (eg, nitrites, large number of leukocytes).[9] It is important to note that, while microscopic hematuria is common in patients with urinary calculi, the absence of blood in the urine does not exclude the presence of stones.[10] Additionally, certain crystals may be seen on urine microscopy further suggesting the diagnosis, and even composition, of the stone.10
Testing may be conducted with a one-time urine sample provided in the UC center although this is often non-diagnostic for the stone’s likely composition. A 24-hour urine collection test may show the patient excreting too many calculi-forming minerals or too few stone-preventing substances and is often part of outpatient urological work-up.10
Dipstick and/or microscopic analysis of a midstream specimen of urine should be performed to assess for underlying infection.[11] An alkaline pH may suggest infection with a urea-splitting organism.[12] Positive nitrites has the highest specificity for concomitant urinary infection (85-98%).[13] Leukocytes or leukocyte esterase on the dipstick are also concerning for infection, but less specific.13 In cases of obstructive urinary stones with concern for infection (ie, pyoureter), immediate ED referral is prudent as patients may require urgent nephrostomy tube or ureteral stent to prevent progression to bacteremia and sepsis.[14] Such patients will require, at a minimum, close ongoing monitoring and rapid administration of appropriate antibiotics.[15] Women are at higher risk of sepsis related to ureterolithiasis.15
Blood tests in urgent care are often not immediately available, however, no routine blood lab testing is necessary in uncomplicated cases of kidney stone passage.9 In fact, many lab results may be misleading or lead to unnecessary further testing due to their lack of specificity. For example, mild leukocytosis is common in patients presenting with ureterolithiasis due to pain-related stress demargination.[16] Creatinine also has been shown to return to baseline in most cases when elevated and, therefore, can be reasonably deferred if close follow-up is ensured.[17] Patients with urinary calculi have twice the risk of chronic kidney disease (CKD) compared to those without nephrolithiasis, however, and therefore do benefit from urologist guided monitoring of renal function.[18]
Diagnostic Imaging
The appropriate imaging modality for evaluating for suspected urinary calculi depends on many factors including the clinical setting, patient body habitus, cost, and risk of ionizing radiation exposure. While there are multiple modalities to choose from, those used clinically are generally limited to CT, ultrasound (US) and plain film radiography (ie, KUB).4
Computerized Tomography
CT of the abdomen and pelvis has become the most widely used modality for diagnosing urinary calculi over recent decades.4 By the end of the 20th century, there was a rapid rise in the use of CT for many indications and CT use has increased from around 3 million per year in 1980 to over 62 million in 2006.16 However, increasing evidence has demonstrated the risks associated with cumulative ionizing radiation exposure from CT scans, most notably as it relates to lifetime risk of malignancy. Patients with urinary stone disease are at a particularly high risk of excessive diagnostic radiation exposure given the recurrent nature of calculi formation.[19]
Sensitivity and Specificity
CT is the most sensitive and specific modality for imaging when suspecting urinary system calculi. The ACR estimates the sensitivity of CT to be ~95% and the specificity of CT to be 98% in patients with acute flank pain.[20],[21] Almost all calculi are radiopaque on CT except for the rare exception of stones caused by the precipitation of protease-inhibitor medications (eg, ritonavir) in the urine.20 CT imaging can also provide information regarding the composition of calculi by using the Hounsfield unit measurement of their attenuation.20 CT, while often not immediately available in UC, does have the additional benefit of identifying alternate diagnoses that may mimic ureterolithiasis with high sensitivity (eg, diverticulitis, appendicitis).[22]
Relevant Guidelines
Standard CT of the abdomen and pelvis without contrast is the imaging modality of choice for obese (ie, BMI >30) patients according to the ACR, AUA, and EUA.[23],20,21 The ACR and AUA both recommend CT scan as the first-line investigation for adult patients presenting with symptoms suggestive of obstructive nephrolithiasis. The EAU recommends that CT be used to confirm a stone diagnosis for cases in which ultrasonography is equivocal.23
Low-dose Radiation CT
Low-dose CT is a method of reducing radiation exposure by lowering the tube current to the radiation source. A low-dose CT study provides similar information to that provided by standard CT when evaluating for suspected urinary stones. Data regarding calculus size and location are still easily assessed and the Hounsfield units (HU) can still be measured predict stone composition.20
Relevant Guidelines
Currently, the ACR, AUA and EAU do not recommend low-dose CT scans for patients with a BMI >30 as they are believed to have inferior sensitivity and specificity in this patient population.20,21,23 When considering low-dose protocols, clinicians should be mindful of the patient’s age, BMI, and degree of clinical suspicion of calculi in order to choose the optimal imaging option.23
Kidney, Ureter, Bladder Radiography
KUB radiography can provide clues about the cause of renal colic if a calcification is detected in the anticipated area of the ureter on the side where the patient is experiencing pain. However, it is important to note that not all stones are visible on radiographs. Moreover, some calcifications that appear on XR may not be located in the ureter (eg, phleboliths or other types of vascular calcifications). Distinguishing between these entities can be challenging when viewing a single two-dimensional image.
Sensitivity and Specificity
The effectiveness of a KUB in detecting urolithiasis can be influenced by various factors, including the composition, location, and size of the stone, as well as the patient’s body habitus and the presence of bowel contents overlying the area. One study has demonstrated only 63% of stones >5 mm and only 8% of stones ≤5 mm being visualized by KUB when comparted to CT.[24] Additionally, calculi such as cystine and struvite are often poorly visible on KUB radiography, and uric acid and matrix calculi are usually fully radiolucent.24
Relevant Guidelines
The American College of Radiology (ACR) recommends CT scan as “usually appropriate” in patients with a suspicion of stone disease, compared to a KUB which “may be appropriate.”21 These authors recommend that while KUB is more widely available, it holds relatively limited clinical utility in the UC setting.21
Ultrasound
US is generally a lower cost imaging modality and does not rely upon ionizing radiation. It has become the primary alternative to CT as clinician training in point-of-care US (POCUS) has increased and US technology has become more widely available.21 A wide range of sensitivities and specificities for US have been reported, probably owing to variations in technique, body habitus, patient population and reference standards.[25] Imaging calculi in the renal pelvis and in the ureter also present different challenges due to artifact and interference from bowel gas.25
Sensitivity and Specificity
A review of the literature suggests that US has a pooled sensitivity and specificity of 45% and 94%, respectively, for detection of ureteral calculi and 45% and 88%, respectively, for renal calculi.25 Sensitivity is reduced for calculi < 3 mm, and calculi can be missed in a decompressed renal pelvis owing to the difficulty in distinguishing echogenic calculi from echogenic central sinus fat in the kidney.25 Sensitivity can be improved by combining ultrasonography with KUB radiography. Sensitivity and specificity for these combined studies range from 58% to 100% and 37% to 100%, respectively.[26]
Relevant Guidelines
The ACR and AUA recommend CT evaluation as a first-line investigation of patients with suspected kidney calculi, whereas the EAU recommends starting with US.21,23,[27] To reduce the cumulative effects of ionizing radiation, especially in pediatric and young adult patients and those who are pregnant, the ACR, AUA and EAU recommend US as a first-line imaging modality.21,23,27 US also has increased accuracy in children owing to their small body size meaning that the distance between the US probe and anatomy of interest is reduced.[28]
Useful Additional Ultrasound Technique
In pregnant women, signs of obstruction such as a lack of ureteral jets can be used as a surrogate marker of an obstructing calculus.[29] Use of the twinkling artefact assists in identifying calculi and can improve the specificity of US by differentiating calculi from other echogenic structures.[30] B-mode and Doppler US can be used to induce a twinkling artifact. The twinkling artifact is the appearance of a mosaic of colors in a Doppler US image.30
Patients with Recurrent Stones
Immediate imaging is not typically advised for patients displaying symptoms suggestive of recurrent and uncomplicated ureterolithiasis. This recommendation takes into consideration the patient’s prior history of kidney or ureter stones. If a patient has a well-documented history of such stones, and their symptoms align with a typical stone episode, healthcare providers might initially rely on the patient’s medical history and clinical presentation to establish a diagnosis.
It is crucial to understand that this recommendation is not an absolute rule and can vary depending on individual patient factors and the clinical judgment of the healthcare provider. If the patient’s symptoms do not improve, worsen, or if there is any suspicion of complications, such as infection or complete blockage, then imaging may be promptly conducted to aid in making treatment decisions. In such cases, it is advisable to refer the patient to a urologist urgently (or an ED if severe symptoms) for a determination regarding the necessity of imaging.
Urgent Care Considerations
While CT is the preferred first-line imaging modality for most patients with suspected urinary stones based on the ACR and AUA guidelines, it is not often readily available from UC. Additionally, immediate US is also rarely accessible from UC as well. POCUS provides a useful option, if available, and has been widely adopted in emergency medicine practice. However, it is unclear to what extent UC clinicians have access and proficiency with this technology.[31]
While no specific guidelines exist for UC evaluation and management of patients with suspected ureterolithiasis, it is reasonable to forego any immediate imaging if CT and US are not immediately available in patients with reassuring vitals and urinalysis who are minimally symptomatic and can follow-up quickly with a urologist. Given the natural history of uneventful passage in the majority of patients, ED referral can generally be reserved for patients who develop intractable symptoms or concerns for concomitant infection.24
Treatment and Management
Acute Renal Colic Management
For management of acute renal colic, pain relief is the top priority.[32] Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ketorolac 15-30 mg intramuscularly (IM) are effective and have fewer adverse effects than opioids.[33] In patients tolerating oral fluids well, oral ibuprofen (usually at doses between 400-600mg) can provide similar relief to IM ketorolac.[34] Increased oral fluid intake or intravenous fluid administration is generally not therapeutic in the acute management of pain related to renal colic.[35]
Many suspected or confirmed ureteral calculi may be watched conservatively after UC presentation with close urologist follow-up arranged. For stones <5 mm in size, the chance of passage without intervention is ~90%. Medical expulsive therapy with alpha-blockers (eg, tamsulosin) is controversial. A recent Cochrane Review demonstrated a modest effect in improving passage for larger stones (>5mm) but also increased rates of adverse reactions (mostly orthostatic hypotension) in patients treated with alpha-blockers.[36] As it is rare that the size of a calculus will be known in UC, use of medical expulsive therapy is reasonable in patients at low risk of harm from orthostasis (eg, younger patients, patients not at risk for falls, etc.).
Any suggestion of coexisting urinary infection should be treated with antibiotics. This may be simple cystitis but in patients with fever, severe flank pain, or other systemic symptoms, pyoureter must be considered.31
Immediate referral to the ED is appropriate if:
- Adequate analgesia cannot be achieved with oral agents
- Intractable vomiting
- Pyoureter and/or sepsis is suspected
- Bilateral urinary obstruction or unilateral obstruction with solitary kidney is suspected
- Older patients or those with significant comorbidities in which other life-threatening diagnoses such as abdominal aortic aneurysm cannot be excluded[37]
Figure 1 shows an algorithm for the diagnosis and management of acute kidney stones.37
Surgical Management
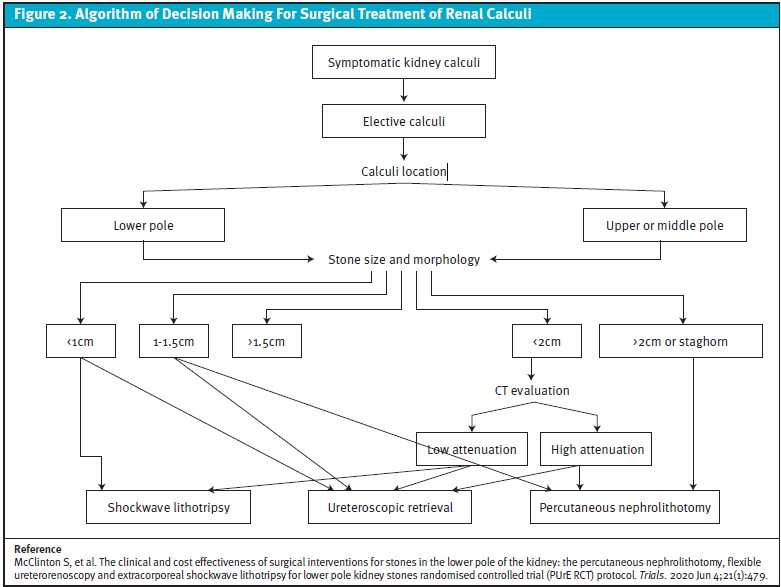
For surgical management, the most common three treatment modalities for renal calculi are extracorporeal shockwave lithptripsy (ESL), ureteroscopic retrieval (with rigid or flexible retrograde ureteroscopy), and percutaneous nephrolithotomy.[38] The advantages and disadvantages of these therapies depends on the experience of the treating urologist, stone factors, such as size, location and composition, and patient characteristics, such as body habitus, medical co-morbidities, and anatomy. With the appropriate patient and procedure selection, there is a high stone clearance rate, low associate morbidity and quick recovery time.38 A general decision-making algorithm for these procedures depends on stone location, size, and density (see Figure 2).
Conclusion
Urinary calculi are a common issue for which many patients may seek care initially in an UC setting. The evaluation of patients with characteristic flank pain suggestive of possible renal colic/ureterolithiasis depends on history, physical exam, and urinalysis. Imaging is recommended in all patients either with CT or US, but may be deferred in mild presentations when rapid urologist follow-up can be assured. Decisions regarding immediate ED referral are case dependent and warrant consideration of severity of symptoms, concerns for infection, and patient co-morbidities, most notably.
Urinary calculi of 5mm or less have 90% chance of passage without intervention. When access to advanced imaging from UC is possible, US is the preferred first-line imaging modality for younger patients and those who are pregnant. For older patients and those with larger body habitus, CT of the abdomen and pelvis without contrast is recommended. In patients with BMI <30, a reduced dose CT scan is preferrable as it offers similar sensitivity and specificity.
Oral ibuprofen has similar efficacy to parenteral ketorolac and is a reasonable agent for ongoing analgesia in patients without contraindications to NSAIDs. Medical expulsive therapy with alpha-blockers may offer a small benefit for passage, especially in stones >5mm, but does carry risk of adverse reactions, which must also be considered.
Patients with confirmed stones should be referred for urology follow-up as this is a chronic condition in many patients which can increase risk of CKD. Appropriate management of current stones and therapies and lifestyle changes that mitigate stone formation can minimize the aggregate lifetime morbidity and symptoms related to urinary calculi.
References
- [1] Patti L, Leslie SW. Acute Renal Colic. Treasure Island (FL): StatPearls Publishing; 2022
- [2] Hill AJ, Basourakos SP, Lewicki P, et al. Incidence of Kidney Stones in the United States: The Continuous National Health and Nutrition Examination Survey. J Urol. 2022;207(4):851-856. doi:10.1097/JU.0000000000002331
- [3] Scales CD, Smith AC, Hanley JM, Saigal CS, Project UDiA. Prevalence of kidney stones in the United States. Eur Urol. 2012;62(1):160-5.
- [4] Weisenthal K, Karthik P, Shaw M, Sengupta D, Bhargaven M. Evaluation of kidney stones with reduced radiation dose CT: progress from 2011-2012 to 2015-2016 not there yet. Radiology. 2018;286(2):370-732.
- [5] Ordon M, Schuler TD, Ghiculete D, Pace KT, Honey RJ. Stones lodge at three sites of anatomic narrowing in the ureter: clinical fact or fiction? J Endourol. 2013;27(3):270-6.
- [6] Meria P, Hadjadj H, Jungers P, Daudon M, Committee MotFUAU. Stone formation: pathophysiological insights gained from morphoconstitutional stone analysis. J Urol. 2010;183(4):1412-6.
- [7] Blanco LT, Socarras MR, Montero RF, Diez EL, Calvo AO, Gregorio SAY, Cansino JR, Galan JA, Rivas JG. Renal colic during pregnancy: Diagnostic and therapeutic aspects. Literature review. Cent European J Urol. 2017;70(1):93-100.
- [8] Meher S, Gibbons N, DasGupta R. Renal stones in pregnancy. Obstet Med. 2014;7(3):103-10.
- [9] Weinstock M.B., Klauer K.M. Bouncebacks! Critical care: avoid serious mistakes in the ED. USA:Gatekeeper;2021.
- [10] Mitchell T, Kumar P, Reddy T, Wood KD, Knight J, Assimos DG, Holmes RP. Dietary oxalate and kidney stone formation. Am J Physiol Renal Physiol. 2019 Mar 1;316(3):F409-F413. doi: 10.1152/ajprenal.00373.2018. Epub 2018 Dec 19.
- [11] Bafna P, Deepanjali S, Mandal J, Balamurugan N, Swaminathan RP, Kadhiravan T. Reevaluating the true diagnostic accuracy of dipstick tests to diagnose urinary tract infection using Bayesian latent class analysis. PLoS One. 2020 Dec 31;15(12):e0244870.
- [12] Wattengel BA, Schroeck J, DiTursi S, Sellick JA, Mergenhagen KA. 1466. Alkaline Urine: A Cause for Urinary Tract Infection Recurrence. Open Forum Infect Dis. 2019 Oct 23;6(Suppl 2):S535. doi: 10.1093/ofid/ofz360.1330.
- [13] Deville WL, Yzermans JC, van Duijn NP, et al. The urine dipstick test useful to rule out infections. A meta-analysis of the accuracy. BMC Urol. 2004;4:4.
- [14] Reyner K, Heffner AC, Karvetski CH. Urinary obstruction is an important complicating factor in patients with septic shock due to urinary infection. Am J Emerg Med. 2016:34(40):694-6.
- [15] Margolin EJ, Wallace BK, Movassaghi M, Miles CH, Shaish H, Golan R, Katz MJ, Anderson CB, Shah O. Predicting Sepsis in Patients with Ureteral Stones in the Emergency Department. J Endourol. 2022 Jul;36(7):961-968. doi: 10.1089/end.2021.0893. Epub 2022 Apr 22.
- [16] Fwu CW, Eggers PW, Kimmel PL, Kusek JW, Kirkali Z. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;83(3):479-86.
- [17] Haley WE, Enders FT, Vaughan LE, et al. Kidney function after the first kidney stone event. Mayo Clinic Proceed. 2016;91(12):1744-52
- [18] El-Zoghby ZM, Lieske JC, Foley RN, et al. Urolithiasis and the risk of ESRD. Clin J Am Soc Nephrol. 2012;7(9):1409–1415.
- [19] Ferrandino MN, Bagrodia A, Pierre SA, Scales CD, Rampersaud E, Pearle MS, et al. Radiation exposure in the acute and short-term management of urolithiasis at 2 academic centers. J Urol. 2009;181(2):668-72; discussion 73.
- [20] Alsyouf M, Smith DL, Olgin G, Heldt JP, Lightfoot M, Li R, et al. Comparing stone attenuation in low- and conventional-dose noncontrast computed tomography. J Endourol. 2014;28(6):704-7.
- [21] Coursey CA, Casalino DD, Remer EM, Arellano RS, Bishoff JT, Dighe M, et al. ACR Appropriateness Criteria® acute onset flank pain–suspicion of stone disease. Ultrasound Q. 2012;28(3):227-33.
- [22] Sugi MD, Sun DC, Menias CO, Prabhu V, Choi HH. Acute diverticulitis: Key features for guiding clinical management. Eur J Radiol. 2020;128:109026. doi:10.1016/j.ejrad.2020.109026.
- [23] Geraghty RM, Davis NF, Tzelves L, Lombardo R, Yuan C, Thomas K, et al. Best Practice in Interventional Management of Urolithiasis: An Update from the European Association of Urology Guidelines Panel for Urolithiasis 2022. Eur Urol Focus. 2022.
- [24] Kanno T, Takahashi T, Ito K, Okada T, Higashi Y, Yamada H. The Natural History of Asymptomatic Renal Stones ≤5 mm: Comparison with ≥5 mm. J Endourol. 2020;34(11):1188-1194. doi:10.1089/end.2020.0336.
- [25] Ray AA, Ghiculete D, Pace KT, Honey RJ. Limitations to ultrasound in the detection and measurement of urinary tract calculi. Urology. 2010;76(2):295-300.
- [26] Brisbane W, Bailey MR, Sorensen MD. An overview of kidney stone imaging techniques. Nat Rev Urol. 2016 Nov;13(11):654-662.
- [27] Fulgham PF, Assimos DG, Pearle MS, Preminger GM. Clinical effectiveness protocols for imaging in the management of ureteral calculous disease: AUA technology assessment. J Urol. 2013;189(4):1203-13.
- [28] Strohmair WL. Imaging in pediatric urolithiasis—what’s the best choice?. Tran. Ped. 2015 Jan;4(1).
- [29] Asrat T, Roossin MC, Miller EI. Ultrasonographic detection of ureteral jets in normal pregnancy. Am J Obstet Gynecol. 1998;178(6):1194-8.
- [30] Cunitz B, Dunmire B, Paun M, Sapozhnikov O, Kucewicz J, Hsi R, et al. Improved Detection of Kidney Stones Using an Optimized Doppler Imaging Sequence. IEEE Int Ultrason Symp. 2014;2014:452-5.
- [31] Mills L, Morley EJ, Soucy Z, Vilke GM, Lam SHF. Ultrasound for the Diagnosis and Management of Suspected Urolithiasis in the Emergency Department. J Emerg Med. 2018;54(2):215-220. doi:10.1016/j.jemermed.2017.09.020.
- [32] Türk C, Petřík A, Sarica K, et al. EAU guidelines on diagnosis and conservative management of urolithiasis. Eur Urol. 2016;69(3):468-474.
- [33] Afshar K, Jafari S, Marks AJ, Eftekhari A, MacNeily AE. Nonsteroidal anti-inflammatory drugs (NSAIDs) and non-opioids for acute renal colic. Cochrane Database Syst Rev. 2015(6):CD006027.
- [34] Cai F, Liao Y, Jiang S, Cao Y, Wang Y. Comparison of Ibuprofen with Ketorolac on the Control of Renal Colic Pain: A Meta-Analysis of Randomized Controlled Studies [published online ahead of print, 2023 Aug 19]. Urol J. 2023;10.22037/uj.v20i.7572. doi:10.22037/uj.v20i.7572.
- [35] Worster AS, Bhanich Supapol W. Fluids and diuretics for acute ureteric colic. Cochrane Database Syst Rev. 2012(2):CD004926.
- [36] Campschroer T, Zhu X, Vernooij RW, Lock MT. Alpha-blockers as medical expulsive therapy for ureteral stones. Cochrane Database Syst Rev. 2018;4(4):CD008509. Published 2018 Apr 5. doi:10.1002/14651858.CD008509.pub3.
- [37] Manjunath AS, Hofer MD. Urologic Emergencies. Med Clin North Am. 2018;102(2):373-385. doi:10.1016/j.mcna.2017.10.013.
- [38] McClinton S, Starr K, Thomas R, MacLennan G, Lam T, Hernandez R, Pickard R, Anson K, Clark T, MacLennan S, Thomas D, Smith D, Turney B, McDonald A, Cameron S, Wiseman O. The clinical and cost effectiveness of surgical interventions for stones in the lower pole of the kidney: the percutaneous nephrolithotomy, flexible ureterorenoscopy and extracorporeal shockwave lithotripsy for lower pole kidney stones randomised controlled trial (PUrE RCT) protocol. Trials. 2020 Jun 4;21(1):479.
Author Affiliation: Andrew Alaya MD MSc, HMC in The Hague, The Netherlands. The author has no relevant financial relationships with any commercial interests.

