Published on
Urgent message: Many urgent care clinics face new competition and the landscape for reimbursement is changing. One tactic for enhancing profitability is to consider the addition of new services. Adding Physical Therapy to your practice can result in more satisfied patients, better clinical outcomes and a stronger bottom line.
LAUREL STOIMENOFF, PT and HILARY HELLMAN, SLP
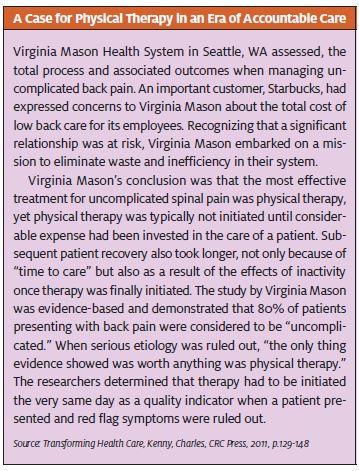
Eighty percent of Americans will experience low back pain at some time in their lives. Many of these patients will present to an urgent care clinic in search of relief, particularly when onset is acute. Some cases may be work-related injuries whereas others will be covered by commercial or other insurance. Early intervention with physical therapy is well documented to influence the most favorable and timely return to prior levels of function for patients and also to mitigate risks of re-injury. For the most cost-effective outcomes, urgent care clinics should either have referral relationships with local therapy clinics that offer same-day or next-day appointments and can make services available to the clinics’ patients or the urgent care clinics should consider providing these early intervention therapy services themselves.
UCA’s 2012 Benchmarking Survey indicated that 13% of reporting organizations included physical therapy as a part of their urgent care business. In addition, 36.8% indicated that they added new services during 2011. Depending on the mix and volume of patients being seen in an urgent care business, the addition of physical therapy as a new line of service can make excellent business sense both clinically and financially. As the industry seeks to identify methodologies to demonstrate value under accountable care (beyond the obvious savings associated with emergency department diversion), early intervention and access to care, including physical therapy, should be a fundamental benefit we offer.
This article is Part 1 of 2 and addresses early considerations, rationale for implementation and legal considerations that must be addressed when adding this new line of service. Part 2, in a subsequent issue, will address more tactical considerations and the “how” of implementing physical therapy in your practice.
Establishing the Legal Entity
In most states, a physical therapy program can be included as an ancillary service provided by an urgent care entity, even one that is physician-owned. Among the states that prohibit or restrict physician ownership of a physical therapy practice are Missouri, Colorado, Delaware, and South Carolina, typically because of concerns associated with over utilization secondary to “self- referral.” Urgent care center owners should seek legal counsel related to specific state nuances before establishing their own therapy service. Our industry also must ensure that prescriptions and motivations are directed toward cost-effectively addressing soft tissue, pain, and movement disorders. Practice benchmarks for physical therapy care and utilization by diagnostic code are avail- able through resources such as the Official Disability Guidelines (ODG), The Medical Disability Advisor (MDA), and the American College of Occupational & Environmental Medicine Practice Guidelines.
Stark Regulations
Final Stark Regulations provide that the “in-office ancillary services” exception to the Stark prohibition on referrals apply to physician ownership of a physical therapy practice if the supervision, location, and billing requirements are satisfied. “Because the therapist in private practice rules do not require personal or direct physician supervision, physician groups billing therapy under these rules can satisfy the Stark supervision requirements with or without a physician on site.”1
In addition, if the in-office ancillary services exceptions are met, the physical therapy practice can be located either at the same address as the medical office or at another location. This may be beneficial if the organization has several urgent care locations that are in close enough proximity to establish one physical therapy location convenient to the majority of its patients.
Contracting/Credentialing
Each physical therapist should have his or her own Medicare provider number as well as a unique National Provider Identifier (NPI) number. This will allow each therapist to treat Medicare patients and eliminate the need for a physician to be onsite in order for a therapy visit to be billed.
The need to credential therapists for each commercial payor will vary, but it is often advantageous to bill incident to the physician when possible. This is because the reimbursement rate under physician contracts is likely to be higher than for physical therapists not associated with a physician practice or hospital. Whenever possible, it is recommended that physical therapy be included as part of the physician contracts for ease of submitting claims and to ensure the most favorable rates. It is imperative to know the cost of delivering a therapy visit in order to favorably position yourself for payors moving to visit rate payments. Establishing case rates for an episode of care that include physician services and imaging and therapy services is more complicated and requires a complete understanding of the costs of providing all services. Protocol-driven care by diagnosis is an effective way to control cost and ensure quality out- comes in a case-rate payment system.
Compliance With Legislation at the State Level
Just as in the practice of medicine, physical therapy is regulated by State Boards whose charter is public protection. Physical Therapists are licensed in every state and the District of Columbia. Therapy professionals should be familiar with the regulations and restrictions around the provision of care; however, it is best for each urgent care center offering this service line to be cognizant of the regulations. State Physical Therapy Practice Acts often limit the number of sup- port staff that can be supervised by each licensee and typically define their scope of services. Both the Practice Act and State physical therapy/occupational therapy rules should be reviewed at least annually to ensure compliance with any changes. In addition, individual licensees should understand that they have a responsibility to protect their own licenses and to practice ethically and lawfully.
Caseload to Support a Financially Solvent Practice
Key drivers for physical therapy are similar to those in an urgent care center, with the exception that recurring visits to complete a patient’s course of care should be factored in when assessing total cost of care to the payor or patient. Reimbursement for therapy services can be on a fee-for-service basis or a global rate. In the latter case, the intensity of care provided is irrelevant as it relates to ultimate compensation= for services rendered.
Other less frequent but emerging methodologies include case rates (one payment for all services, irrespective of intensity or number of visits with expectations for outcomes and quality) and capitation.
Medicare Beneficiaries have historically been limited to an annual “cap” of $1,880 for combined Physical & Speech Therapy Services. New in 2013, the “cap” now also applies to hospital-based and/or -owned outpatient programs.
One full-time physical therapist can typically remain productive and profitable for the practice when the urgent care clinic can produce 10 to 12 new physical therapy patients per week. Before implementing a full-time therapy service, an urgent care provider should analyze his or her clinic’s historical caseload and determine if a full or part-time service is appropriate. Many therapists seek part-time work and many therapy referrals call for services one to three times per week. Therefore, a 3-day-per- week on-site clinician may be the best way to test the viability of physical therapy and it also affords the practice same- or next-day appointments for early intervention.
A 2010 survey completed by Corvel found that 77% of Workers’ Compensation cases manifested in a physical therapy referral and the average number of therapy visits per claimant were 11 to 15. (That number includes postoperative rehabilitation, so an urgent care center’s visits per patient would likely be lower [per case]).2
Workers’ Compensation as a percentage of an urgent care center’s business is only a single consideration for potential new patient volume. Physical therapists are highly trained in analysis of movement and posture dis- orders. In addition, they are adept at caring for patients who present with balance disorders, benign paroxysmal positional vertigo, chronic headaches, overuse disorders including carpal tunnel syndrome, gait disorders, generalized weakness, neurological deficits and acute and chronic pain. Therapists may also have earned specialty certifications in orthopedics, sports, neurology, cardio- vascular & pulmonary, geriatrics, pediatrics, clinical electrophysiology and women’s health.
When analyzing an urgent care clinic’s diagnostic mix, it is important to consider all cases—not just musculoskeletal disorders—in which therapy intervention may improve function and quality of life. Therefore, when assessing a practice’s historical coding for services, it is important to not only consider ICD-9 codes that are
related to the musculoskeletal and connective tissues (710-739) but also neurologically based codes (320- 389), and injuries (800-959).
As an example, the baby boomer generation is aging and the risk associated with falls and muscle wasting will become increasingly prevalent. Urgent care clinics often have the opportunity to identify red flags for fall risk when patients seek care. An example is the “Five Times Sit to Stand” test and its associated benchmarks for fall risk and morbidities. Research strongly supports that a comprehensive therapy program that addresses strength, endurance, balance and flexibility can greatly reduce the risk of falls in older adults.3
The addition of a physical therapy component to an urgent care center also opens up opportunities to more aggressively pursue the 80% of people experiencing low back pain at some time in their lifetime or to increase community outreach by working with local schools to offer comprehensive “bump & bruise” clinics following sporting events. An urgent care center’s customers typically extend beyond the patient, often including the payor or the employer. No matter who the customer is, rapid return to prior level of function is the ultimate objective and ready access to medical care at the urgent care clinic coupled with ready access to professional therapy services is the formula for success.
Despite the many opportunities for therapy intervention, consideration must be given to consumer behaviors as patients experience increasing co-payments and co-insurance responsibilities. Therapists must also be sensitive to their financial obligations and strive to establish home exercise programs and encourage per- sonal responsibility towards goal achievement. While this is the ethically right thing to do, it manifests in fewer visits per patient. Because services provided to injured workers are 100% covered, they are more likely to complete the course of care toward established goals. Therapists also may run up against annual limits on therapy services based on their therapy benefit. Many physical therapists respond to this situation by establishing cash payment programs so patients can affordably continue care. One example in which that scenario might apply would be rehabilitation of a young athlete who anticipates a return to sports following surgery on an anterior cruciate ligament and for whom 12 to 15 visits per year are not likely to suffice.
Physical therapists should also communicate regularly with the providers and staff relative to their skill sets and opportunities to provide value. New providers to the practice should have time with the therapist to under
stand when an appropriate referral can be initiated. Specialty programs can be developed and cash pay services related to personal training programs or physical activities to support weight loss programs can also be offered to augment the practice and increase foot traffic to the urgent care center. Practice owners should consider whether external referrals are an option, based on organizational structure and relationships in the medical community. Free-standing clinics or separate entry- way access will support the impression that access to physical therapy services is not simply limited to urgent care- generated referrals. To accomplish this objective, the physical therapist must be involved in marketing the business to employers, primary care physicians, orthopedists, and neurologists.
Coding and Appropriate Utilization of Services
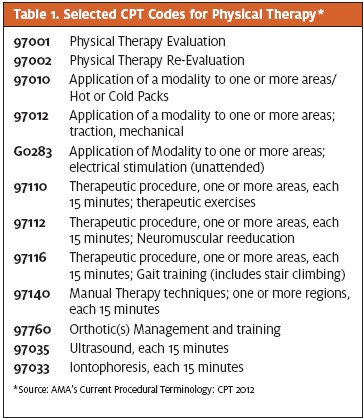
In most states physical therapy services are billed using the Physical Medicine & Rehabilitation CPT Codes. They are distinguished as either “time-based” where more than one may be billed per session or non-time- based, allowing for only one billed code per session. Most rehabilitation codes for services can be found in the CPT range of 90000 to 99600. Table 1 lists some, but not all, of the typical codes that are used in the urgent care setting.
Appropriate utilization of therapy services is essential for payment and must require the skills and intervention of the therapist. Documentation must support not only the services billed, but that the skills of the therapist are necessary. Take, for example, a patient who is issued crutches as the result of an injury and for whom the urgent care provider orders gait training. The physical therapist’s intervention should involve not only assessment of the patient for safety and selection of crutches over alternative assistive device options (e.g, a walker), evaluation of triceps strength, and review of fit- ting considerations for the crutch pad space in the axilla and appropriate elbow flexion, but also cueing during training and safety instructions and training for navigating ramps, stairs, and curbs.
Metrics for Success
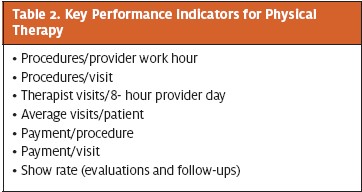
Just as in traditional medicine, the quality of a physical therapy visit and, by extension, the level of success in achieving a prompt return to function for a patient relates to access and face time with the therapist. There- fore, productivity expectations must be reasonable and aligned with an organization’s quality objectives. Therapy productivity is impacted by the acuity of the patient population and the intensity of services provided. Most therapists, when supported by an aide or Physical Therapist Assistant (PTA), are comfortable seeing 10 to 15 patients in an 8-hour day. Reimbursement per visit, like other aspects of medicine, continues to experience reimbursement pressures. The 2010 Corvel Study indicated that reimbursement for Workers’ Compensation- related therapy visits ranged from $80 to $175.2
Despite these ongoing pressures, urgent care clinics must remain committed to providing the highest quality of care with the best clinical outcomes and the highest level of patient satisfaction while at the same time remaining prof- itable. Reliable data are essential to effectively manage an outpatient physical therapy ancillary service.
Recommended key performance indicators (KPIs) are listed in Table 2.
Conclusion
The urgent care industry undeniably plays a role in reducing the cost of health care. Just as early intervention in management of disease typically manifests in more favorable outcomes and fewer complications, the same holds true for implementation of a quality physical therapy program. In many urgent care settings, the addition of a physical therapy service is a low-risk expansion opportunity.
In the next issue of The Journal of Urgent Care Medicine, Part 2 of this article will provide more tactical considerations for implementation of physical therapy, including the revenue cycle from referral to payment, patient scheduling, equipment purchases, space needs, creating a 3-year pro forma, recruitment of the physical therapist, and staffing models.
References
- Edgar White Paper: The Stark Exception for Physical Therapy Ancillary Services & Other Ancillaries. http://ancillarycaresolutions.com
- Corvel CompInSights Physical Therapy Report 2010. http://www.corvel.com/ compInsights/media/Report_Physical_Therapy_April_2010.pdf. Accessed March 6, 2013.
- Means KM, Rodell DE, O’Sullivan Balance, mobility, and falls among community- dwelling elderly persons: effects of a rehabilitation exercise program. Am J Phys Med Reha- bil. 2005;84(4):238-250.

