Urgent message: Utilization of validated scoring systems and clinical decision-making tools can enable the urgent care provider to manage many patients presenting with symptoms of deep-vein thrombosis in the urgent care center, reducing the need for costly referral to the emergency room.
Daniel Eisner, DMSc, PA-C
ABSTRACT
Management of venous thromboembolism accounts for $10 billion in medical spending annually, with much of the cost attributable to emergency room visits. Conversely, managing VTE patients in the urgent care center is safe, less costly, and helps prevent acuity degradation in the urgent care setting.
CASE PRESENTATION
A 35-year-old female presented on a Saturday morning with 5 days of left calf pain that started soon after she arrived on a flight from Mexico to Pennsylvania. She described the discomfort as cramping, persistent, and not responding to ibuprofen. The day before she presented to the clinic, she noticed her left calf was larger than the right and she had started limping. She could not recall any trauma to the area and she denied chest pain, shortness of breath or history of previous venous thromboembolism (VTE). She had no significant past medical or surgical history and her only medication was oral birth control pills. Her mother had type 2 diabetes but her family history was otherwise unremarkable, with no history of bleeding disorders or VTE. She smoked socially and rarely consumed alcohol.
Physical Exam
On exam, she was afebrile and able to speak in full sentences. Her pulse was 78, blood pressure 136/84, respirations 18, pulse oximetry 99%, and BMI 31. The lung and heart exam was normal. On left lower extremity inspection, a 4 cm difference in size was noted when compared with the right calf. It was painful with light palpation at the posterior aspect only and warm to the touch. Slight erythema was noted throughout the posterior calf, with no lesions. Nonpitting edema was noted at the ankle and dorsal foot. Pedal pulses were 3+ bilaterally
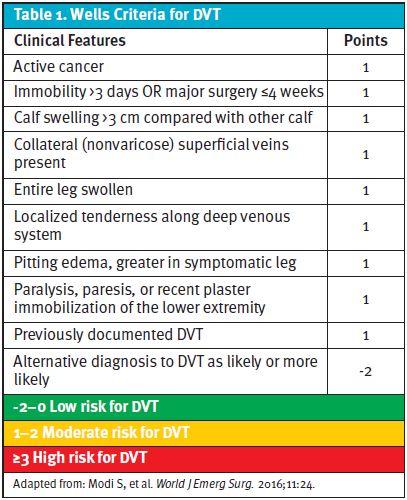
The Wells Criteria for DVT score (Table 1) was 2, placing her in the moderate risk group category.
Lab Testing
A qualitative point-of-care D-dimer test was positive. Urine pregnancy test was negative. Since she had just returned from international travel and would eventually be getting outpatient diagnostic testing, a COVID-19 PCR test was ordered and came back 2 days later as negative.
Management
ED referral was declined by the patient (her concern being the wait time during the COVID-19 pandemic) and she preferred anticoagulation over monitoring with serial imaging.
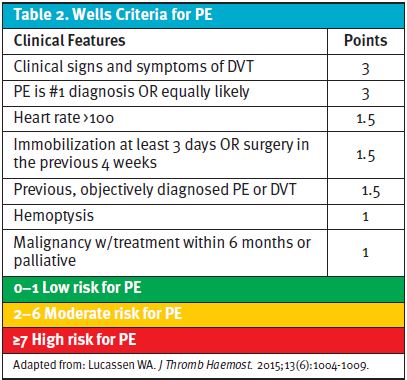
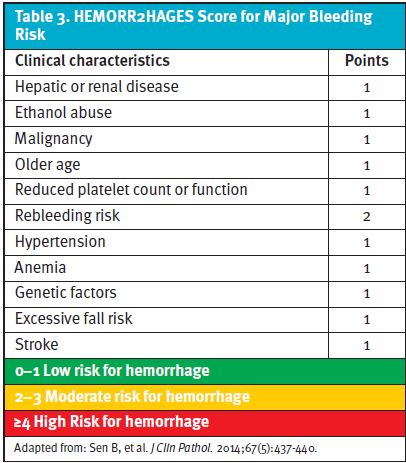
Using Well’s Criteria for Pulmonary Embolism (Table 2) and HEMORR2HAGES (Table 3) for bleeding risk, her scores totaled 3 (moderate risk group) and 0 (low risk group), respectively.
After discussing the risks and benefits of outpatient management of DVT, rivaroxaban was initiated, starting with a starter kit. This would be continued for 3 months, pending both the results of the ultrasound and a vascular specialist consult. Rubicon eConsult, an online platform that allows same-day access to specialists, was also consulted and the treatment plan proposed was deemed acceptable.
Two days later, compression ultrasound confirmed a thrombus in the gastrocnemius vein. The remainder of the leg was clear of any thrombi, both distal and proximal. The next day she had an appointment with a vascular specialist who took over the case for the remainder of the time she was on rivaroxaban. A chest CT was thought to be unnecessary, as she continued to score low on the Well’s Criteria for PE. She discontinued her birth control and no longer smokes.
DISCUSSION
VTE can present as a DVT, PE, or both. Approximately 80% of patients with a PE will have a DVT and 50% of those with a proximal DVT will have a PE.1 The Centers for Disease Control and Prevention estimates there are up to 900,000 cases of DVT annually in the United States, with 10% to 30% of patients dying within the first month.2 The costs of VTE management is estimated at up to $10 billion a year.3
When considering the management of DVT in an outpatient setting, an extrinsic factor to cause a provoked VTE must be isolated.4 There should be no previous history of VTE and risk factors for bleeding and/or severe PE should be low to nonexistent (low-risk PE can also be safely treated as outpatient in certain candidates5). A pretest probability scoring system, such as the Wells Criteria for DVT,6 along with a review of recent labs, past medical history, and family history should be utilized to determine if D-dimer POCT is appropriate.6
Since management will be outpatient and diagnostic testing may be delayed, it is acceptable to initiate parenteral or direct oral anticoagulants (DOAC) until diagnostic testing can be completed.7 DOACs with a reversal agent are preferred (for rivaroxaban, it is Andexxa8). To assess bleeding risk, HEMORR2HAGES is validated for use in elderly patients with atrial fibrillation but should be sufficient for patients when we are considering anticoagulation. For the low-to-moderate risk patient, anticoagulation treatment should be continued for a minimum of 3 months.7 If a provoking factor cannot be isolated or the patient is considered high risk, outpatient management may not be appropriate.
Despite multiple studies and expert recommendations encouraging outpatient treatment of low-risk candidates with VTE, a high rate of hospital admission persists.9,10 Over Inpatient costs can be more than double that of outpatient,11 with differences in socioeconomic, gender, race, and age adding more.10,12 Besides increased costs and unnecessary testing, overcrowding in the hospital, especially during the pandemic, can lead to errors and suboptimal care.13
It is important to avoid overtreatment or undertreatment while balancing the cost of therapy.1 Considering home-treated DVT can be 56% lower than the classic inpatient, heparin-warfarin bridge route, 9 VTE management with DOACs is recommended.14 Utilizing outpatient diagnostic centers can help alleviate the strain on overburdened health systems. Multiple POCT kits are available for outpatient settings and have proven to be cost effective and timesaving,15 with the quality of the results comparable to lab-based D-dimer tests.16 While a laboratory quantitative test is superior, qualitative testing and scoring systems in combination have shown to be just as useful,17 with qualitative methods yielding quicker results.18
CONCLUSION
By distinguishing low-risk from high-risk patients with DVT, the clinician has the opportunity to help alleviate overcrowding in the hospitals while lowering the risk of medical errors and suboptimal care. Utilizing pretest probability scores, point-of-care testing, DOACs and outpatient diagnostic studies leads to significant cost-containment.
Manuscript submitted February 24, 2022; accepted March 8, 2022.
REFERENCES
- Rugvedita S Parakh, Daniel E Sabath. Venous thromboembolism: role of the clinical laboratory in diagnosis and management. J Applied Lab Med. 2019;3(5):870–882.
- Centers for Disease Control and Prevention. Data and statistics on venous thromboembolism. Available at: https://www.cdc.gov/ncbddd/dvt/data.html. Accessed January 22, 2021.
- Grosse SD, Nelson RE, Nyarko KA, et al. The economic burden of incident venous thromboembolism in the United States: a review of estimated attributable healthcare costs. Thromb Res. 2016;137:3-10.
- Kearon C, Ageno W, Cannegieter SC, et al. Subcommittees on Control of Anticoagulation, and Predictive and Diagnostic Variables in Thrombotic Disease. Categorization of patients as having provoked or unprovoked venous thromboembolism: Guidance from the SSC of ISTH. J Thromb Haemost. 2016;14(7):1480-1483.
- Roy PM, Moumneh T, Penaloza A, Sanchez O. Outpatient management of pulmonary embolism. Thromb Res. 2017;155:92-100.
- Schulman S, Ageno W, Konstantinides SV. Venous thromboembolism: past, present and future. Thrombosis and Haemost. 2017;117(7):1219-1229.
- Streiff MB, Agnelli G, Connors JM, et al. Guidance for the treatment of deep vein thrombosis and pulmonary embolism. J Thromb Thrombolysis. 2016;41(1):32-67.
- Andexxa—an antidote for apixaban and rivaroxaban. JAMA. 2018;320(4):399-400.
- Singer AJ, Thode HC Jr, Peacock WF 4th. Admission rates for emergency department patients with venous thromboembolism and estimation of the proportion of low risk pulmonary embolism patients: a US perspective. Clinic Exp Emerg Med. 2016;3(3):126-131.
- Vinson DR, Ballard DW, Huang J, et al. Outpatient management of emergency department patients with acute pulmonary embolism: variation, patient characteristics, and outcomes. Ann Emerg Med. 2018;72(1):62-72.e3.
- LaMori JC, Shoheiber O, Mody SH, Bookhart BK. Inpatient resource use and cost burden of deep vein thrombosis and pulmonary embolism in the United States. Clin Ther. 2015;37(1):62-70.
- Douce D, McClure LA, Lutsey P, et al. Outpatient treatment of deep vein thrombosis in the United States: the reasons for geographic and racial differences in stroke study. J Hosp Med. 2017;12(10):826-830.
- Morley C, Unwin M, Peterson GM, et al. Emergency department crowding: a systematic review of causes, consequences and solutions. PLOS ONE. 2018; 13(8): e0203316.
- Deitelzweig S, Laliberté F, Crivera C, et al. Hospitalizations and other health care resource utilization among patients with deep vein thrombosis treated with rivaroxaban versus low-molecular-weight heparin and warfarin in the outpatient setting. Clin Ther. 2016;38(8):1803-1816.e3.
- Price CP, Fay M, Hopstaken RM. Point-of-care testing for d-dimer in the diagnosis of venous thromboembolism in primary care: a narrative review. Cardiol Ther. 2021;10(1):27-40.
- Hendriksen JMT, Geersing G-J, van Voorthuizen SC, et al. The cost-effectiveness of point-of-care d-dimer tests compared with a laboratory test to rule out deep venous thrombosis in primary care. Expert Rev Mol Diagn. 2015;15(1):125-136.
- Lucassen WA, Erkens PM, Geersing GJ, et al. Qualitative point-of-care d-dimer testing compared with quantitative d-dimer testing in excluding pulmonary embolism in primary care. J Thromb Haemost. 2015;13(6):1004-1009.
- Sen B, Kesteven P, Avery P. Comparison of D-dimer point of care test (POCT) against current laboratory test in patients with suspected venous thromboembolism (VTE) presenting to the emergency department (ED). J Clin Pathol. 2014;67(5):437-440.
Author affiliations: Daniel Eisner DMSc, PA-C practices in primary and urgent care at Johns Hopkins Community Physicians in Baltimore, MD.
