Published on
Urgent message: Runners who train too much too soon risk serious injury. Prompt and thorough evaluation is necessary to spot CECS masquerading as “shin splints.”
MATTHEW SPEER and JOHN SHUFELDT, MD, JD, MBA, FACEP
Overview
Running is one of the world’s most popular exercises, with millions across the globe participating and training for events from 5K races to ultramarathons of over 100 miles. Despite the fact that more than 10 million people run over 100 days per year, more than half of regular runners find themselves injured each year. Moreover, many such injuries result from overexertion or overuse.
Chronic exertional compartment syndrome (CECS), which often masquerades as shin splints, is one example of a running-related injury that results from repetitive microtrauma. Because endurance athletes typically avoid any sort of treatment that involves rest, immediate recognition of CECS is of utmost importance to avoid further complications. As illustrated by the case presented here, conducting a proper examination with attention to both history and symptoms will ensure an accurate diagnosis and proper treatment.
Case Presentation
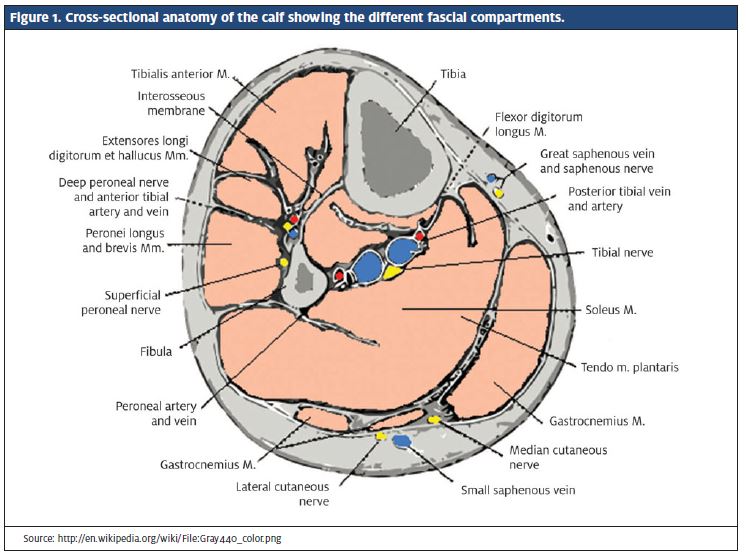
A 19-year-old male long-distance runner presents with sharp, cramping pain in the anterior compartment of his lower right leg that gradually intensifies during physical exertion, similar to that associated with medial tibial stress syndrome (shin splints). He reports that the pain generally subsides within approximately 25 to 30 minutes after he ceases physical activity. The discomfort is associated with some paresthesia and numbness bilaterally down the anterior compartment of each leg (Figure 1)
The patient has been seen twice in the urgent care setting with the same symptoms, which were diagnosed both times as shin splits. The treatment recommended was scaling down the patient’s weekly mileage, icing the affected area, and taking ibuprofen or acetaminophen daily until the swelling and pain subsided. The patient reports that the pain and other symptoms have persisted and now linger longer after each run.
Labs/Imaging
Measurement of compartment pressure with the Stryker Intracompartmental Pressure Monitor is actually quite easy despite the fact that it is considered beyond the scope of many urgent care centers. In this case, measurement of compartment pressure in the patient’s lower leg was necessary to make a definitive diagnosis because his history and physical examination suggested CECS. Such measurements can be done at an urgent care center or an emergency department or be performed by an orthopedist.
Measurements taken with and without exercise are considered to be the gold standard for diagnosis of CECS. Proposed by Pedowitz etal, the criteria for confirmation of CECS in the leg are as follows:
- A pre-exercise/rest pressure 15 mm Hg or higher
- A 1-minute post-exercise pressure 30 mm Hg or higher
- A 5-minute post-exercise pressure 20 mm Hg or higher
Although Pedowitz suggests that only one of the above criteria are necessary to confirm a CECS diagnosis, it should be noted that the confidence level increases with the number of criteria met. The following equipment is necessary to accurately measure the pressure in a given compartment:
- Stryker Intra-Compartmental Pressure Monitor System
- Syringe, prefilled with saline
- Side-port needle
- Diaphragm chamber
- Arterial line transducer system
- Intracompartment needle
- High-pressure tubing
- Pressure transducer with cable
- Pressure monitor/module
- Sterile saline
- Variable-height transducer stand
- Two 3-way stopcocks
- Syringe, 20 mL
Measurement Technique
The technique used for measuring compartment pres- sure varies greatly depending on the compartment being tested. For purposes of this case study, we will describe the technique for measuring pressures in the anterior compartment of the lower leg. In all cases, however, the following should be observed:
- The compartment to be measured (the anterior compartment of the lower leg, in this case) should be at the same level as the heart;
- The patient and the corresponding compartment should be positioned such that the needle is introduced perpendicularly into the compartment; and
- The skin at the site of insertion should be properly prepared as for any sterile procedure and local anesthesia should be
Anterior Compartment Technique
With the patient supine, palpate the anterior border of the tibia at the level of the junction of the proximal and middle thirds of the lower leg. Identify the needle entry point 1-cm lateral to the anterior border of the tibia. Orient the needle so that it is perpendicular to the skin and insert it to a depth of 1 to 3 cm. The most common error with both the Stryker monitor set and the arterial line transducer system is depressing the syringe plunger too quickly. This may give a transient falsely elevated reading. Another source of error with either system is obstruction of the needle with a plug of tissue if the syringe plunger is pulled back.
Results
Compartment measurements of the patient’s left leg produced the following results:
- A pre-exercise/rest pressure of 18 mm Hg
- A 1-minute post-exercise pressure of 35 mm Hg
- A 5-minute post-exercise pressure of 24 mm Hg
Alternatively, the pressures in the patient’s right leg were as follows:
- A pre-exercise/rest pressure of 21 mm Hg
- A 1-minute post-exercise pressure of 41 mm Hg
- A 5-minute post-exercise pressure of 32 mm Hg
Diagnosis and Treatment
Because this patient met all three pressure criteria, his was a classic presentation of bilateral CECS. Referral was made to an orthopedic surgeon for scheduling of an elective fasciotomy. A few key factors underscored the differential diagnosis. A tibial stress fracture or shin splints initially could be ruled out because the patient’s pain ceased approximately 25 to 30 minutes after physical exertion. Focal tenderness is typical of tendinopathy, which can be seen by testing various muscle groups at rest. A bone scan and magnetic resonance imaging would help to rule out a stress fracture, stress reaction, and any possible nerve entrapment.
Discussion
Once CECS is diagnosed, the treatment most likely to return a patient to his or her former level of physical fitness is surgery. Fasciotomy (Figure 2) typically is necessary to allow the muscle to expand more within the compartment, which facilitates regulated flow of oxygen-rich blood throughout the lower leg. The procedure can be per- formed in one of a four ways: (1) open fasciotomy with 1 or The alternative is cessation of the inciting activity.
Abrupt changes in a training regimen often lead to injuries such as CECS. When increasing training volume or training intensity, patients should be counseled to gradually increase the volume or intensity (typically a 10% increase per week is advised). Limiting weekly volume to 2 incisions; (2), minimally invasive subcutaneous fasciotomy through 1 or 2 incisions; (3), partial fasciectomy; or (3) subcutaneous endoscopic fasciotomy, which can be done with and or without use of balloon dissectors.
An open fasciotomy involves 1 to 2 large incisions through which fascial tissue is cut. Minimally invasive subcutaneous fasciotomy involves incision of fascia blindly via small skin incision(s). A portion of the fascia is removed in fasciotomy with partial faciectomy. In subcutaneous endoscopic fasciotomy, use of a balloon dissector creates an optical cavity through which the fascia can be visualized and space in which to perform dis- section with endoscopic equipment.
Although surgery is the most effective treatment for CECS, cessation of the inciting physical activity would also lead to lessening or disappearance of a patient’s symptoms. Because this condition typically occurs in endurance athletes, however, patients are unlikely to be willing to completely forgo their former level of activity. That, coupled with the fact that any nonsurgical treatment or rehabilitation would fail to truly alleviate any muscle ischemia as a result of reduced blood flow, gives weight to surgical intervention as treatment of choice.
Summary
Chronic exertional compartment syndrome is an exercise-induced neuromuscular condition characterized by pain due to repetitive microtrauma, typically in the lower legs (although it can also been found in the fore- arms). Stereotypically seen in young endurance athletes, CECS often masquerades as shin splints and is chronically misdiagnosed in urgent care centers and emergency departments.
In patients who present with symptoms of CECS, proper diagnosis requires measurement of compartment pressures both before and during exercise. If these measurements confirm the diagnosis, a patient should be referred to an orthopedic surgeon for a fasciotomy approximately 40 miles will reduce the number of injuries. Moreover, it is advisable to run no more than 4 or 5 days per week, with one long run (13+ miles) taking place only once every 14 days.
If the patient described here had continued his training regimen on the assumption that he was suffering shin splints, a vicious cycle of worsening tissue perfusion could have resulted in the loss of one or both lower legs, thus forcing an abrupt end to his running career.
References
- Detmer, Diagnosis and management of chronic compartment syndrome of the leg. Sem Orthop. 1988;3:223.
- Qvarfordt P, Christenson JT, Eklöf B, et Intramuscular pressure, muscle blood flow, and skeletal muscle metabolism in chronic anterior tibial compartment syndrome. Clin Orthop Relat Res. 1983;179:284-290.
- Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni Modified criteria for the objec- tive diagnosis of chronic compartment syndrome of the leg. Am J Sports Med. Jan-Feb 1990;18(1):35-40.
- Rowdon GA, Agnew S, Goodman SB, Keenan MAE, Rabin SI, Smith DG, Visotsky JL, Wal- lace Chronic exertional compartment syndrome. Medscape Reference. Aug 2011. http://emedicine.medscape.com/article/88014-overview.
- Styf JR, Körner Diagnosis of chronic anterior compartment syndrome in the lower leg. Acta Orthop Scand. 1987;58:139.
- Turnipseed Diagnosis and management of chronic compartment syndrome. Sur- gery. 2002;132:613.
- Wittstein J, Moorman CT, III, Levin Endoscopic compartment release for chronic exer- tional compartment syndrome. Am Jour Sports Med. 2010;20:1–6.


