Urgent message: Patient discomfort, inconvenience, and concerns—warranted or not—over possible vision loss make it essential for the urgent care clinician to quickly distinguish between benign conditions and those requiring referral, and to be able communicate clearly with the patient.
By Eric Langerman, medical student, Colleen Czerniak, pharmacy student, Mikayla Spangler PharmD, Shailendra Saxena, MD, PhD
Any ocular pathology can be distressing to the patient, as such conditions can often disrupt activity and even provoke concern about possible vision loss. Therefore, it is essential for an acute care physician—including the urgent care physician—to have a ready paradigm for evaluating these pathologies.
Specifically, it is important to differentiate a benign condition from one needing an ophthalmology referral and to reassure the patient accordingly.
Here, we use a case history to contrast two of the more common palpebral lesions: styes or hordeolums and chalazia.


History of Present Illness
A 50-year-old female presented with a chief complaint of a three- to four-day history of right eyelid swelling, pain, and redness. The patient denied any trauma, discharge, or change in vision, and reported no systemic symptoms or other complaints.
On examination, the superior portion of the right eyelid was erythematous and swollen, as well as warm and tender to palpation.
The sclera was clear and there was no sign of conjunctivitis.
Pen light examination showed the pupils to be equal in size and both the direct and consensual pupillary reaction to be intact.
With this history, a stye or chalazion is most likely, but blepharitis and sebaceous carcinoma must also be in the differential. It is particularly important to differentiate between styes and chalazia, as there are management implications.
Relevant Anatomy
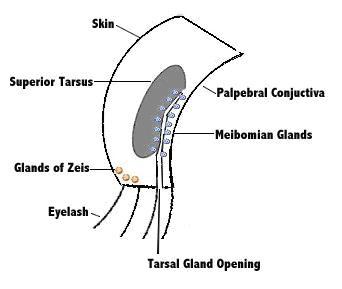
The superior palpebra house several glands, any of which may become inflamed. Just deep to the conjunctiva lays the superior tarsus, a dense connective tissue plate that contains the tarsal or meibomian glands, the site of pathology in a chalazion. In the inferior lid margin deep to the skin, there are sebaceous glands, also called the Zeis’ gland.
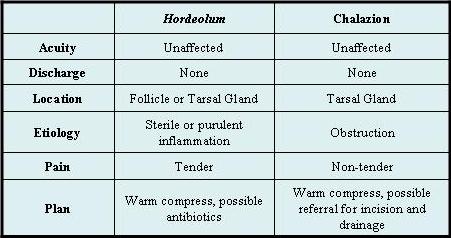
There are two types of styes—external and internal, with the former making up the vast majority. The more common external hordeola originate from an eyelash follicle or in the sebaceous glands of Zeis’ in the lid margin. The much rarer internal hordeola is an inflammation of the same tarsal glands affected by a chalazion.1,2
Table 1. Contrasting Features of Hordeola and Chalazia1
Relevant palpebral anatomy
Treatment
Despite contrasting locations and etiologies, both hordeola and chalazia may be initially treated by applying warm compresses to promote drainage.
In the uncomplicated case, resolution will likely follow, though on a longer time course in chalazia (weeks to months) compared with styes (days to weeks).
Referral to ophthalmology for incision and drainage or glucocorticoid (e.g., triamcinolone) injection is warranted for recurrent or refractory chalazia. To rule out malignancy, a tissue sample should also be evaluated by a pathologist.
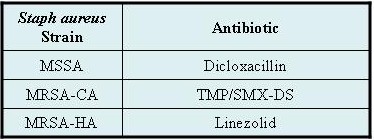
Internal hordeola may harden into chalazia, and would also need referral for incision and drainage. If a stye is associated with preseptal cellulitis, the first line antibiotic is a penicillin class medication with Staph aureus coverage.3 Cephalexin 500 mg bid for seven to 10 days, is a common regimen. In case of allergy, topical erythromycin applied TID or oral trimethoprim/sulfamethoxazole or clindamycin may be used.3,4
Table 2 Antibiotics for treatment of hordeola associated cellulitis.2
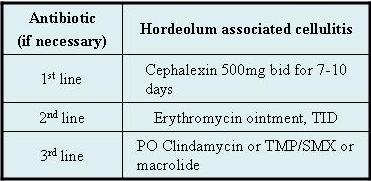
Table 3 Treatment for infected internal hordeola3
References
1. Ghosh C, Ghosh T. Eyelid lesions. Up to Date. Available at: http://www.uptodate.com/patients/content/topic.do?topicKey=~fOOfEP4PI9A6IM.
2. Cotran RS, Kumar V, Robbins SL, et al. Robbins Pathologic Basis of Disease. 7th ed. Philadelphia: Saunders, 2005.
3. Ehrenhaus MP, Sturridge KA. Hordeolum. E-medicine from WebMD. Available at: http://emedicine.medscape.com/article/1213080-overview.
4.Gilbert DN, Moellering RC, Eliopoulos GM, et al, eds. The Sanford Guide to Antimicrobial Therapy 2009. 39th ed. Westville, NJ: Antimicrobial Therapy, Inc., 2009.

