Urgent message: Sometimes, cellulitis can be confused with gout – especially when it involves the area around a joint. A detailed history and physical exam, along with diagnostic testing, will help you reach definite diagnosis.
Introduction
Gout is a metabolic disease characterized by recurrent episodes of acute arthritis. It is a type of monoarticular arthritis caused by deposition of monosodium urate crystals in and around the joint.
Hyperuricemia (serum uric acid level >6.5 mg/dL) seems to be associated with increased frequency of acute gouty attack.1,2 In 50% of the cases, gout affects the first metatarsophalyngeal joint; men are commonly affected than women.3
A typical gout attack is sudden in onset and associated with swelling, redness, warmth and severe pain in the effected joint. Symptoms usually peak in 12 to 24 hours. Patients may also develop fever, chills, malaise and diffuse erythema of the skin surrounding the joint, thus mimicking cellulitis. Cellulitis is an acute infection causing inflammation and involving the epidermis, dermis, and subcutaneous layers of the skin. The most common causes are S aureus and b-hemolytic streptococci (most commonly group A S pyogenes). In practice, the specific causative organism is usually not isolated. Blood cultures are usually negative.4 Skin swabs are rarely diagnostic.
Case
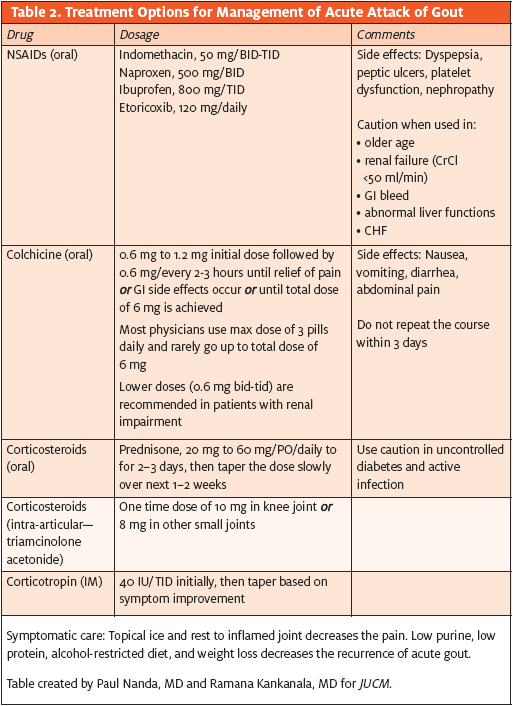
A 45-year-old obese, Caucasian male presented to urgent care with a chief complaint of right thumb swelling, redness, and excruciating pain for five days (Figure 1).

Three days prior, he presented to ED with similar complaints; he was diagnosed with gout and sent home on naproxen sodium and hydrocodone-acetaminophen tablets for pain control.
The patient was advised to follow up with his primary care physician for long-term medication for his gout. Today, in the urgent care he has worsening right thumb swelling, redness and pain.
His past medical history was significant for a long history of gout. He also has multiple tophi involving the elbow, ankle and finger joints (Figure 2).

Other significant past medical history includes chronic gout with tophi formation, hyperuricemia, cellulitis, and hypertension. He has no history of septic arthritis or rheumatoid arthritis; no history of travel or tick bites; and no history of trauma. His identical twin brother also has history of gout. Currently, the patient is not on any medication for gout.
The patient did admit that he drinks beer two to three times per week, has smoked cigarettes for the past 25 years, and “occasionally” uses marijuana. His diet, typically, includes salami, bologna, pinto beans, chicken, and pork.
Initial Evaluation and Management
Physical exam
The right thumb displayed a decreased range of motion and is painful, diffusely swollen, erythematous, has skin excoriation, and is tender to palpation. In addition, redness extended to the base of the right thumb.
Movement around the metacarpophalangeal joint and interphalangeal joint is painful. Physical exam also showed multiple tophi in his elbows, ankles, and heel. The rest of the physical exam was normal.
Labs and imaging
Reading of an x-ray of the right hand was consistent with a synovial inflammatory process. Lucencies in the osseous structures appeared to represent cysts, likely related to calcium pyrophosphate deposition (CPPD) arthropathy. Rheumatoid arthritis and gout were possibilities, as well. WBC count was 16000 cell/cc. Renal and liver function were within normal limits. Uric acid was -7.4. Other serum chemistry was normal. A general culture swab collected form the wound site was sent in for culture. This later grew Staphylococcus aureus. Two sets of blood cultures were both negative.
Aspiration was not initially performed as the right thumb appeared to show classic signs of cellulitis.
Differential Diagnosis
Gout, cellulitis, pseudogout, septic arthritis, or some combinations of these diagnoses were suspected.
Diagnosis
Initially, the patient was diagnosed with gout in the ED and was sent home on an NSAID.
Subsequently, he presented to urgent care complaining of worsening right thumb pain, increased redness (involving the entire thumb) and swelling. Labs show an elevated white blood cell count.
Ultimately, the diagnosis of cellulitis with or without gout was made in urgent care.
Discussion
Gout
The clinical picture and elevated serum uric level suggest a diagnosis of possible acute gouty arthritis.
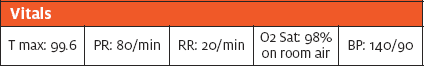
The presence of six or more minor criteria or one major criteria (Table 1) appears to be required to make a diagnosis of acute gout (sensitivity: 74%; specificity: 99%.2,5). For typical presentations of gout, a clinical diagnosis alone is reasonably accurate (mean score of 95%), but not definitive without crystal confirmation.1
Definitive diagnosis is polarized light microscopy into clinical practice, providing urate crystal identification (negatively birefringent needle-shaped crystals) in synovial fluid.3 Overall, normal to low serum urate values have been noted in 12% to 43% of patients with acute episodes of gout. Although uric acid levels is the most important risk factor for gout,3 serum uric acid levels do not confirm or exclude gout.1 Presence of tophi also has high diagnostic value.1
Risk factors for gout include male sex, presence of diabetes, hypertension, obesity, chronic renal failure, a high purine diet, alcohol consumption (not wine), and medication (aspirin, hydrochlorothiazide).1,6-8
Cellulitis
Cellulitis is a soft tissue infection involving the epidermis, dermis, and subcutaneous tissue.
In this case, the patient complained of worsening redness, swelling, and pain. On physical exam, there was diffuse erythema involving the areas proximal and distal to the first interphalangeal joint. In addition, the patient had signs of inflammation extending beyond the confines of the joint that is primarily involved. There is also excoriation of skin (Figure 1). This feature even gives the impression of cellulitis. The white blood cell count may be elevated in acute gout; fever is also a common finding. These two findings, while consistent with infection, cannot be used to confirm cellulitis, however. Gradual worsening of signs and symptoms in spite of treatment for gout also point towards cellulitis.
Pseudogout
Pseudogout is a monoarticular arthritis caused by deposition of calcium pyrophosphate dehydrates crystal in the perisynovial joint area. It is less common than gout. Clinical presentation is very similar to gout: sudden onset of pain, redness and swelling in the joint. Hypothyroidism, chronic renal insufficiency, diabetes, and hyperparathyroidism are some of the risk factors associated with pseudogout. Definitive diagnosis is made by synovial fluid analysis; crystals from this aspirate show weakly positive birefringent, linear, or rhomboid crystals. Treatment of pseudogout is similar to the treatment of gout.
Septic arthritis
The term “septic arthritis” usually refers to bacterial infection – the most common cause of septic arthritis – of the joint. Signs and symptoms include joint swelling, warmth, pain, restricted joint movement9; these are commonly associated with fever. fluid analysis (Gram stain, culture, leukocyte count) is the definitive diagnostic test. In our patient, the infection involved soft tissue infection of the entire thumb. Moreover, he had been afebrile and the joint did not seem to be as tender, compared to rest of the thumb. Since the patient had underlying cellulitis, we chose initially not to obtain synovial fluid analysis.
Treatment Plan
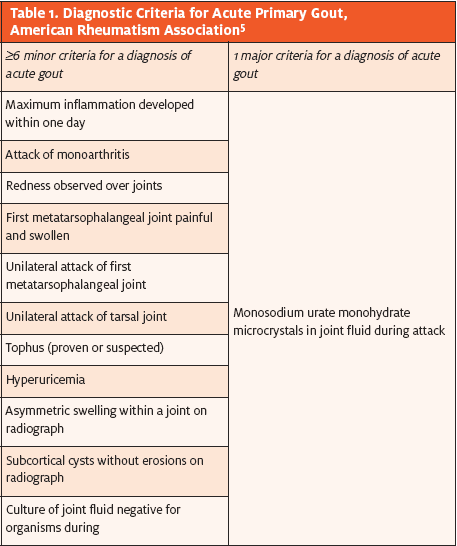
Acute gout
Nonspecific measures such as resting and elevating and cooling the affected limb provide symptomatic relief. NSAIDs, all of which seem to be equally effective when started early in the course of the disease, are the initial treatment of choice. Complete resolution of symptoms occurs in five to 10 days. Colchicine is a safe option in patients who are allergic to NSAIDs or with a history of chronic kidney disease or gastrointestinal bleed is. Such patients should be informed about the side effects of colchicine, which include flushing, abdominal bloating, and diarrhea.
Oral steroids (e.g., prednisone, triamcinolone) are appropriate for patients who cannot take NSAIDs or colchicine.
Abstaining from alcohol, decreasing meat and seafood intake, and stopping specific medications (e.g., hydrochlorothiazide, aspirin) will help speed recovery.
Urate-lowering therapies, started six to eight after the attack has resolved, are indicated in patients who have two are more attacks per year.10 If patients are already on urate-lowering drugs, discontinuation of the drug during the acute attack is not recommended, as this will exacerbate the symptoms.
Pseudogout
Medical treatment for pseudogout is similar to treatment for gout. Acute cases are treated with NSAIDs, plus or minus colchicine.
Cellulitis
Cellulitis is primarily a clinical diagnosis. However, early cellulitis involving the digits is sometimes mistaken for gout.
Cellulitis should be considered in patients who have not responded to NSAIDs, colchicine, or corticosteroids. Culture and sensitivities are obtained depending on the case presentation. Treatment with antibiotics depends on the local microbial susceptibilities.
Conclusion
Cellulitis is sometimes misdiagnosed as gout. When in doubt, treat it as cellulitis. Use antibiotics based on local susceptibilities. This patient had cellulitis with both underlying gout and pseudogout with tophi formation. He was started on sulfasuxamide-trimethoprim double strength, naproxen sodium, oxycodone for pain, and promethazine for nausea. Follow-up general culture grew methicillin resistant Staphylococcus aureus sensitive to sulfasuxamide-trimethoprim.
Over the next seven days, our patient improved significantly.
References
1. Zhang W, Doherty M, Pascual E, et al. EULAR evidence based recommendations for gout. Part I: Diagnosis. Report of a task force of the Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann Rheum Dis 2006;65:1301-1311.
2. Ma L, Cranney A, Holroyd-Leduc JM. Acute monoarthritis: What is the cause of my patient’s painful swollen joint? CMAJ. 2009;180(1):59-65.
3. Schlesinger N. Management of acute and chronic gouty arthritis: Present state-of-the-art. Drugs. 2004;64(21):2399-2416.
4. Bisno AL, Stevens DL. Streptococcal infections of skin and soft tissues. N Engl J Med. 1996; 334:240-245.
5. Wallace SL, Robinson H, Masi AT, et al. Preliminary criteria for the classification of the acute arthritis of primary gout. Arthritis Rheum. 1977;20:895-900.
6. Skipper A. Nutrition Care Manual. American Dietetic Association. Chicago IL; 2008.
7. Choi HK, Gao X, Curhan G. Vitamin C intake and the risk of gout in men: A prospective study. Arch Intern Med. 2009;169:502 – 507.
8. Pillinger MH, Keenan RT. Update on the management of hyperuricemia and gout. Bull NYU Hosp Joint Dis. 2008;66:231-239.
9. Margaretten ME, Kohlwes J, Moore D, et al. Does this adult patient have septic arthritis? JAMA. 2007;297:1478-1488.
10. Emmerson BT. The management of gout. N Engl J Med. 1996;334:455-5

