Urgent message: Many performance-enhancing medications not currently approved by the FDA remain undetectable in basic urine specimens collected in the urgent care setting. If there is suspicion of any form of illicit substance use, the inquiry of specific supplements/agents is key, as side effect profiles are often vast and wide.
Rachael M. Poff, PA-C and Christina E. Gardner, DHSc, MBA, PA-C
INTRODUCTION
Selective androgen receptor modulators (SARMs) constitute a class of medication that has become increasingly popular over the past decade. Their popularity likely stems from the nonsteroidal component the medications possess; SARMs have benefits on both muscle and bone tissues without the negative side effects of a traditional anabolic steroid. SARM molecules are selective in that they target androgen receptors on muscle and bones, but do not influence receptors on androgen-dependent tissues such as prostate, testis, and skin.1
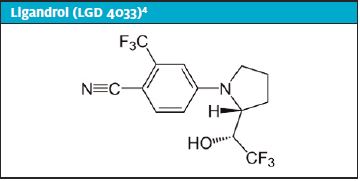
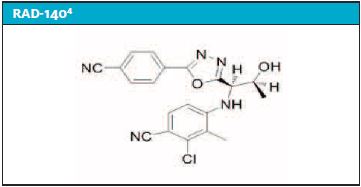
However, these medications have yet to be approved by the Food and Drug Administration (FDA) and are currently labeled “not for human consumption.” In addition, the World Anti-Doping Agency (WADA) further prohibits the usage of SARM agents as they are often labeled “body image-enhancing drugs.”2 Both Ligandrol (LGD 4033) and RAD-140 are examples of two specific SARMs that are listed as prohibited substances on the 2020 edition of the United States Anti-Doping Agency (USADA) as well as the WADA list of banned agents. A 2019 Norwegian study estimated that “6%–9% of all anti-doping rule violations (ADVR) internationally are caused by the use of contaminated dietary supplements.”3 Unbeknownst to the layperson, they may be ingesting products that are not 100% chemically pure.
CASE PRESENTATION
Mr. L is a 27-year-old male who presents to urgent care with dizziness, lightheadedness, and pain over his left antecubital fossa for the past 2 hours. He describes the pain as “pinpoint and sharp.” There is no change when he moves the arm. The patient states he does not feel like his normal self and “it is as if I was high, as if I have done drugs or drank, but I have not taken anything today.” He admits drinking an energy drink prior to symptom onset. He denies any personal medical history of hypertension, diabetes mellitus, hyperlipidemia, hepatitis, hypertrophic obstructive cardiomyopathy, or other cardiovascular events.
He reports current usage of Blue Dragon, a selective androgen receptor modulator (SARM) containing LGD 4033 and RAD 140. He has been using 1 dropper full (equivalent of 1 mL per patient) of both LGD 4033 and RAD 140 approximately 45 minutes prior to gym workouts once per day for the past month. The patient also reports concomitant usage of cocaine and alcohol. The patient’s alcohol usage varies depending on the day, but he states that he drinks “at least two beers a night” with intermittent liquor consumption. His most recent alcohol consumption was the previous night. Illicit drug use entails intermittent cocaine ingestion with last intake 3 weeks ago and episodic ingestion of marijuana. He denies marijuana usage in the past 2 days and denies a history or current use of intravenous drugs.
Observation and Findings
- Vital signs: BP 178/96, HR 73, RR 18, temp 97.9⁰ F, SpO2 100%
- General: On exam, he appears to be anxious
- Eyes: Pupils are approximately 4 mm in size and equal with room lighting. Minimal pupil constriction appreciated with direct light
- RRR without obvious murmur
- Lungs are CTAB with normal pulmonary effort
- Musculoskeletal: FROM without TTP over left antecubital fossa
- Neuro: Normal sensation and 5/5 strength of bilateral upper extremities
- Extremities: 2+ radial pulses noted bilaterally
- Skin: Two small, red pinpoint areas over the left AC fossa without any obvious associated track marks, surrounding erythema, or warmth
- Neuro: No focal neurologic deficits. CN 3-12 are grossly intact. GCS of 15. No facial asymmetry or dysarthria. No motor or sensory deficits noted. Coordination is intact. No pronator drift. Romberg sign is negative
Differential Diagnoses/Decisional-Making
- Atypical chest pain (given concomitant usage of substances)
- Cocaine-induced MI (recent cocaine ingestion)
- Adverse drug reaction from SARMs (ingestion of daily SARMs for one month)
- Anxiety attack (patient appeared anxious)
- Adverse drug reaction from energy drink consumption (ingested energy drink prior to onset of symptoms)
- Acute coronary syndrome (given new onset of dizziness)
Of these, atypical chest pain, adverse drug reaction from SARMs, and cocaine-induced MI were of higher concern when compared with the other diagnoses. These diagnoses were considered to be more likely due to patient’s age, substance ingestion, rapid onset of symptoms, no prior history of said symptoms, and physical exam findings.
Course
Poison control was contacted for guidance of known associated adverse side effects of SARMs. The representative noted limited information on the exact SARM brand or individual agents, but reported that similar SARM products, in an event of overusage or occasional usage, have been associated with hepatic, testicular, and cardiac side effects. Given his symptoms, substance ingestion, and poison control’s recommendations, the patient was sent to the emergency department for further evaluation and management.
Diagnostic Studies/Tests/Labs
An electrocardiogram performed in the urgent care clinic demonstrated a sinus rhythm at a rate of 71 with normal intervals and normal axis in the absence of any acute ST segment changes or T wave inversions. The patient was transferred to the ED where a CBC, CMP, and serial troponins were all essentially normal (Table 1).
Table 1. Laboratory Results Obtained in the Emergency Department
| Laboratory Results | Patient’s Value | Reference Range |
| Troponin | <0.30 ng/mL | <0.30 ng/mL |
| Sodium | 141 mmol/L | 135-145 mmol/L |
| Potassium | 3.9 mmol/L | 3.5-5.3 mmol/L |
| Chloride | 102 mmol/L | 95-107 mmol/L |
| CO2 | 23 mmol/L | 21-31 mmol/L |
| Urea nitrogen | 15 mg/dL | 6-20 mg/dL |
| Creatinine | 1.28 mg/dL | 0.5-1.4 mg/dL |
| Glucose | 93 mg/dL | 70-99 mg/dL |
| Total protein | 7.1 g/dL | 6.0-8.3 g/dL |
| Albumin | 4.4 g/dL | 3.2-5.5 g/dL |
| Total bilirubin | 0.4 mg/dL | < 1.3mg/dL |
| Calcium | 8.9 mg/dL | 8.5-10.7 mg/dL |
| Alkaline phosphatase | 63 IU/L | 42-121 IU/L |
| AST | 49 IU/L | 10-42 IU/L |
| ALT | 36 IU/L | 10-60 IU/L |
| Globulin | 2.7 g/dL | 1.7-3.9 g/dL |
| Albumin/globulin | 1.6 ratio | 0.7-2.3 ratio |
| Anion gap | 16 mmol/L | 8-18 mmol/L |
| Osmolality calc | 293 mos/kg | 278-305 mos/kg |
| Bun/creatinine | 11.7 | 7-20 |
| GFR, Estimated | 77 mL/min | >60 mL/min |
| WBC | 9.3 K/ul | 4.0-10.5 K/ul |
| RBC | 5.13 M/ul | 4.5-5.3 M/ul |
| Hemoglobin | 15.9 g/dL | 13.0-16.0 g/dL |
| Hematocrit | 47.3 % | 37-49 % |
| Platelet count | 301 K/ul | 130-400 K/ul |
DISCUSSION
Given this patient’s ingestion of several different products, it is difficult to decipher which agent or agents were the culprit or if his symptoms were the result of concomitant usage. In addition, SARM agents are often marketed as a single, isolated, and pure substance. However, recent studies have emerged suggesting that this may not necessarily be the case.
Van Wagoner R, et al explored the purity of these agents in their marketed form in a 2017 article, reporting that out of “44 products, only 23 (52%) contained one or more SARM, 17 products (39%) contained another unapproved drug (including growth hormone secretagogue), no active SARM compound was detected in 4 (9%), substances not listed on the label were contained in 11 (25%), and only 18 of the 44 products (41%) had the amount of active compound in the product that matched that listed on the label.” Further, 59% of the products that were marketed for sale differed substantially from that found by laboratory analysis.4
If the two SARM agents that the patient ingested were not chemically pure, this serves as another avenue of investigation into what caused his symptoms. The fact that these agents are for sale (through the black market) does not mean they are safe for ingestion. Perhaps conversations regarding the above article’s findings should be warranted for patients in whom illicit substance use is suspected. Thus, even if SARMs themselves are eventually approved by the FDA, providers still need to consider what additional agents are mixed in with the SARMs.
As medicine continues to evolve, pharmaceutical agents of all kinds continue to diversify, and the black market remains a viable avenue for obtaining substances, providers would be well advised to develop a baseline level of clinical suspicion.
This heightened level of suspicion should entail expanding differential diagnoses as a whole, but particularly for patients who exhibit a wide range of nonspecific symptoms. SARMs are the “new kid on the block” when it comes to “doping agents.” As such, identifying these products using currently available detection methods is difficult if not near impossible. Rather than relying on urinalysis and other laboratory measures, the attention should be focused on finetuning clinical judgement and physical exam skill sets, as these may be the only way to detect the use of a doping agent in the urgent care setting.
Another key aspect to detection of these agents revolves around targeted, non–open-ended specific questions during the history-taking portion of the office visit. The patient in the case described in this article did not consider LGD 4033 nor RAD-140 to be “illicit” substances because they did not contain any anabolic steroids. Broadly inquiring about the usage of “illegal substances” leaves the door open for patients to misunderstand the question. Patients may decline to divulge use of SARMS not in an effort to deceive the provider, but because they may not view them as unlawful substances. Fortunately, in this case scenario, the patient was forthcoming with his SARM usage; however, that may not always be the case.
Given the relatively recent emergence of these agents, there is no one specific antidote or pharmaceutical treatment, per se. Instead, the mainstay of treatment remains symptomatic management, with the cornerstone being fluid administration. As previously mentioned, these molecules are thought to negatively affect hepatic and cardiac functioning; therefore, baseline and routine laboratory measures should be obtained for monitoring purposes. Establishment with a primary care provider to maintain close follow-up is a key aspect in the well-being of these patients.
CASE RESOLUTION
The patient was diagnosed in the ED with atypical chest pain. He was given PO fluids with resolution of his initial symptoms, and was discharged home in stable condition. Follow-up with his PCP was recommended, but not obtained.
CONCLUSION
While the investigation into SARMs is ongoing and the degree to which they affect the human body is being researched further, one common principle is that these molecules are not safe for human consumption. As such, patients need to be educated on the potential for harm these agents possess and the need for observation of subsequent signs and symptoms.
References
- Miklos A, Tero-Vescan A, Vari CE, et al. Selective androgen receptor modulators (SARMs) in the context of doping. Farmacia. 2018;66(5):758-762.
- World Anti-Doping Agency. What is Prohibited. Available at: https://www.wada-ama.org/en/content/what-is-prohibited/prohibited-at-all-times/anabolic-agents. Accessed September 13, 2020.
- Helle C, Sommer A, Syversen P, Lauritzen F. Doping substances in dietary supplements. Tidsskr Nor Laegeforen. 2019;139(4).
- Van Wagoner R, Elchner A, Bhasin S, et al. Chemical composition and labeling of substances marketed as selective androgen receptor modulators and sold via the internet. JAMA;2017;318(20):2004-2010.
Author affiliations: Rachael M. Poff, PA-C, Department of Family and Community Medicine, Carilion Clinic. Christina E. Gardner, DHSc, MBA, PA-C, Carilion Clinic Advanced ACP Fellowship in Urgent Care and Rural Health; Radford University PA Program. The authors have no relevant financial relationships with any commercial interests.

