Differential Diagnoses
Anterior nongranulomatous uveitis
Herpes simplex virus keratitis
Viral conjunctivitis
Corneal abrasion
Diagnosis
Acute angle-closure glaucoma
Learnings
Angle-closure glaucoma is a major cause of blindness worldwide. White individuals have a 0.1% incidence of acute angle-closure glaucoma, whereas those of Inuit descent have an incidence that is up to 40 times higher. Angle-closure glaucoma is also more common in persons aged 55 to 70 years, women, Asians, and individuals with smaller eyes. Many drugs, including anticholinergic agents, tricyclic antidepressants, selective serotonin reuptake inhibitors, and adrenergic agonists, can precipitate angle-closure glaucoma by shifting the lens iris diaphragm anteriorly.
An attack of angle-closure glaucoma occurs when there is a sudden obstruction of aqueous humor outflow through the drainage angle of the eye, causing a rapid increase in intraocular pressure. Primary angle closure may be caused by pupillary block or angle crowding, or both. Pupillary block occurs when the increased iris convexity brings the iris into apposition with the trabecular meshwork, thereby blocking drainage of the aqueous fluid. With an angle-crowding mechanism, anteriorly positioned ciliary processes push the iris anteriorly so that the peripheral iris lies against the trabecular meshwork. Secondary angle closures are associated with other ocular diseases such as iris neovascularization, uveitis, trauma, and lens protein leakage.
Patients often present with an acutely painful red eye and blurred vision. Headache, seeing rainbow-colored halos around lights, nausea, and vomiting may also be present. There may be a recent history of physiologic or pharmacologic pupillary dilation.
What to Look For
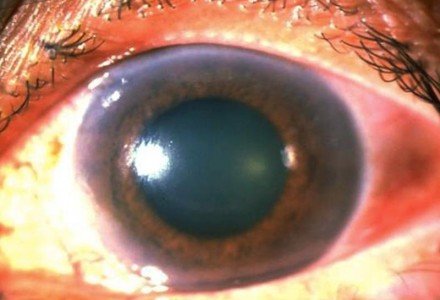
High intraocular pressure associated with a red eye, often with corneal edema (grossly, the cornea may appear cloudy, and the corneal light reflex may appear dull), is typical of acute angle-closure glaucoma. Intraocular pressures of >21 mm Hg are considered high, but with an acute attack of glaucoma, pressures are often >35 mm Hg. Other findings commonly associated with acute angle closure include a mid-dilated, sluggish, and often irregular pupil; a shallowed anterior chamber (especially in the periphery); and a mild amount of anterior uveitis.
The optic nerve may be hyperemic and edematous early in the attack. With prolonged elevated intraocular pressure, the nerve may appear pale, and there may be some disc cupping. There may also be associated retinal ischemia.
Acknowledgment: Image courtesy of Logical Images, Inc. (www.VisualDx.com/JUCM)
