Published on
Download the article PDF: Back Pain From Vertebral Metastases In Prostate Cancer A Case Report
Urgent Message: Persistent, non-mechanical back pain should raise suspicion for non-muscular causes, and in this case, such pain in an older man was related to a diagnosis of metastatic prostate cancer with bone involvement.
Rimsha Afzal, MA; Gregory M. Thompson, MD
Key Words: Vertebral Metastases; Metastatic Prostate Cancer; Urgent Care Diagnosis
Abstract
Introduction: Back pain is a common presentation in the urgent care center. While the majority of diagnoses are self-resolving and of a musculoskeletal nature, consideration of concerning etiologies is necessary based on patient history.
Presentation: A 72-year-old man presented to urgent care with 3 months of progressive, dull, achy thoracic back pain, sometimes waking him at night. Review of his past medical history revealed he had an elevated prostate-specific antigen 6 years ago without follow-up.
Physical Examination: On physical examination, the patient had significant thoracic spine tenderness to palpation, particularly over the midline. Range of motion of the thoracic spine was limited due to pain. Neurological assessment revealed intact motor strength and sensation in the lower extremities with normal reflexes. Gait was steady, and there was no evidence of saddle anesthesia or sphincter dysfunction.
Diagnosis: The patient was referred to the emergency department for further evaluation. Subsequent computed tomography and magnetic resonance imaging of the spine revealed sclerotic lesions in the thoracic spine, suggestive of osteoblastic bone metastases. He was ultimately diagnosed with prostate cancer with bone metastases.
Resolution: Following diagnosis, he was scheduled for outpatient follow-up with his primary care provider to coordinate comprehensive oncology care and ensure appropriate cancer management and support.
Conclusion: In patients with back pain, it is critical that urgent care clinicians recognize concerning elements of history and exam that may indicate the need for advanced imaging.
Introduction
A complaint of back pain is a common presentation in urgent care. While most presentations are caused by non-critical musculoskeletal etiologies, vertebral metastasis from prostate cancer can be a cause of persistent, non-mechanical back pain.
Prostate cancer bone lesions are primarily osteoblastic metastases, leading to abnormal bone formation and increased density. The formation of metastasis is initiated by prostate-specific antigen (PSA), which promotes osteoblastic proliferation. The release of growth factors and cytokines help drive additional bone formation.[1] In addition to pain, approximately 7% of patients with prostate cancer will present with neurological symptoms, such as spinal cord compression.[2] The most common site for spinal cord compression is the thoracic spine.[3] Patients with prostate cancer bone metastases have a 5-year survival of only 33%.[4] In cases of spinal metastases of prostate cancer, the median overall survival is estimated at 24 months.[5]
Case Presentation
A 72-year-old man presented to urgent care with 3 months of progressive, dull, achy thoracic back pain, sometimes waking him at night. The pain was not exacerbated by movement. Over the past year, he also experienced intermittent lower back discomfort, which he attributed to aging. He noted increased urinary frequency, nocturia, and a weaker urinary stream over the past several months. He denied recent trauma but mentioned that his pain had become more persistent and severe despite over-the-counter analgesics. Review of systems was positive for unintentional weight loss of 10 pounds over the past 6 months along with intermittent fatigue and a general sense of decreased stamina. Past medical history revealed an elevated PSA 6 years ago without follow-up since he moved to a new area and had not yet established care with a primary care provider.
Physical Exam
The patient had marked thoracic spine tenderness to palpation over the midline with minimal redness or inflammation. The patient’s vital signs were stable: blood pressure of 128/76 mm Hg; heart rate of 78 beats per minute; respiratory rate of 16 breaths per minute; temperature of 36.8°C; and oxygen saturation of 98% on room air. Plain thoracic and lumbar x-rays were obtained in urgent care, which demonstrated subtle sclerotic changes that were equivocal for metastatic disease.
Medical Decision Making
Due to the severity of the patient’s symptoms and consideration of a concerning diagnosis, the patient was sent to the emergency department (ED) for further evaluation and management.
Differential Diagnosis and Final Diagnosis
The differential diagnosis in this patient included primary malignancy, metastatic disease, fracture, osteomyelitis, or epidural compression syndrome such as cauda equina syndrome. In the ED, computed tomography (CT) and magnetic resonance imaging (MRI) of the spine revealed sclerotic lesions in the thoracic spine, suggestive of osteoblastic bone metastases. He was ultimately diagnosed with prostate cancer with bone metastases.
Discussion
Utilizing a structured approach for the patient with a complaint of back pain will help reduce the likelihood for missing concerning diagnoses.
Understanding The Anatomy
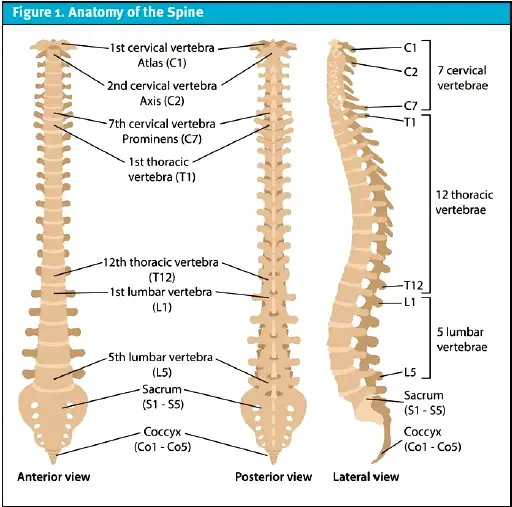
The spine consists of cervical, thoracic, lumbar, sacral, and coccygeal regions.[6] The lumbar vertebrae (L1-L5) are larger and able to withstand higher pressure and body weight (Figure 1). Vertebral bodies are the primary site of malignant metastasis.6 Metastatic lesions from prostate cancer tend to be osteoblastic rather than osteolytic, which leads to abnormal bone formation and increased bone density.6 Despite the sclerotic appearance of bone on imaging, these lesions do not strengthen the bone; rather, they further compromise the structural integrity of the vertebrae making patients susceptible to fractures.
History
In patients presenting with complaints of back pain, it is essential to inquire about relentless, progressive pain especially at night or with weight bearing.1 Patients should be questioned about new or worsening back pain.[7] Pertinent red flag signs/symptoms include age (>50 years), anticoagulation use, fever, genitourinary symptoms (saddle anesthesia, urinary/stool incontinence or retention), immunosuppressed state, and history of malignancy.7 Additionally, prior fractures should be noted, as well as any history of osteoporosis or osteopenia. For patients with a history of malignancy, additional questions should include prior oncologic history, previous hormonal treatments, chemotherapy, or radiotherapy. Asking about cancer screening including PSA values/trends, colonoscopy results, and mammogram results may also be indicated.
Physical Exam
On physical examination, the first steps are inspection, palpation, and range of motion examinations. Findings may include swelling or soft tissue masses, tenderness along the vertebral bodies or back musculature, decreased range of motion, or limping.1
Assessing for motor strength by testing the bilateral lower extremities for weakness helps exclude spinal cord or nerve root compression.7 In patients with low back pain that radiates to the lower extremities (radicular symptoms), about 60% to 80% demonstrate muscle weakness due to spinal cord or nerve root compression.[8] It is also essential to assess for gait disturbances in a patient with low back pain to rule out whether the altered gait is due to the back pain itself or an underlying significant pathology.[9]
Additional deficits may be noted on the neurological exam, such as vibratory and position functions, temperature, hyperreflexia, gait, cerebellar testing, and Babinski reflexes. Light touch and pinprick should be assessed to identify spinal compression that may be causing radicular pain or paresthesia.[10] Neurological pathologies, such as cauda equina syndrome can present with saddle anesthesia. Performing a digital rectal exam to test for decreased anal tone can help guide the diagnosis.[11] Palpable lymph nodes in the inguinal regions may indicate nodal metastasis.
Imaging
In urgent care centers, x-ray services are typically available. A study published in 2006 evaluated the accuracy of radiographs compared to MRI in diagnosing vertebral fractures in adults aged 50-96 years old and found that radiographs correctly identified vertebral fractures in only 51.5% of cases—with a 25.8% false positive rate and 6.5% false negative rate.[12]
In patients with prostate cancer, advanced molecular imaging to detect the degree of metastatic involvement includes a prostate-specific membrane antigen positron emission tomography scan (PSMA-PET), which has the highest specificity and sensitivity for early metastatic disease.[13]
Indications For Referral to the Emergency Department
Signs of spinal cord compression, cauda equina syndrome, infection, or spinal hematoma are indications for immediate referral to the ED as they require prompt treatment and neurosurgery consultation.7 For patients with the above diagnoses due to metastatic prostate cancer, additional consultation to radiation oncology is indicated. Consider the following risk factors, signs, and symptoms for possible ED referral:
- Age >50 years
- Genitourinary issues such as urinary retention
- Constitutional symptoms, such as a fever, malaise, and weight loss
- Hyporeflexia or areflexia
- Reduced anal sphincter tone
- Saddle anesthesia
- Lower extremity weakness
- Recent trauma to suggest a fracture
If spinal cord compression is suspected in the ED, dexamethasone would be initiated immediately until specialists evaluate the patient.[14] Pretreatment ambulatory status is the strongest predictor of function post-treatment in these patients, meaning that if a patient is ambulatory at diagnosis, they have the greatest likelihood of retaining mobility.14 In appropriate cases, the ED can facilitate direct admission to the hospital for medical treatment or to hospice for end-of-life care.[15]
Urgent Care Management
Managing back pain in urgent care primarily focuses on alleviating acute symptoms and identifying clinical features that warrant a prompt referral to the ED. Back pain is a common reason patients seek help from healthcare providers and is a leading cause of disability worldwide.[16] Urgent care providers should be familiar with the indications of referring patients presenting with back pain to the ED.
A 2019 study examined over 2 million ED discharges with nonspecific diagnoses to assess for primary outcomes, and researchers found the most commonly missed condition that presented with back pain was an intraspinal abscess. Additionally, patients with an underlying malignancy were found to have a higher likelihood of experiencing adverse outcomes.[17] Although this study did not evaluate cases in urgent care settings, it underscores the critical importance of a thorough history and physical exam in all clinical environments to avoid missing serious pathologies.
Assessing the risk of fracture is also an essential component to managing these patients in urgent care, especially in weight bearing bones. If a fracture is suspected or confirmed on imaging, an ED referral for surgical evaluation and treatment options is needed.[18]

Next Level Urgent Care Pearls
- Persistent back, hip, or rib pain in a patient with prostate cancer should raise a high suspicion for fracture. Order x-rays and arrange for urgent ED evaluation for a CT/MRI (Figure 2).
- Evaluate indications for immediate referral to the ED, including age, genitourinary symptoms, constitutional symptoms, neurological symptoms, saddle anesthesia, and recent trauma.
Management of Metastatic Prostate Cancer
In order to conduct a proper risk assessment, the Mirel scoring system is used to predict pathological fracture risk and whether a patient is likely to benefit from prophylactic fixation. The scoring system is based on 4 factors: site of the lesion; size; type of lesion (lytic, blastic, mixed); and pain, each scored from 1-3 points. A score of ≥8 indicates the need for surgical intervention.[19]
Surgical techniques may include decompression and stabilization for spinal metastases causing cord compression.[20] Fixation methods could include applying prostheses for lesions destroying the articular surfaces.[21] Prostate cancer metastasizes to the spine occur through the venous drainage system known as Batson’s plexus.[22] Respectively, the thoracic spine is most commonly affected, followed by lumbar, sacral, and cervical areas.[23]
Case Disposition
In the ED, the patient was further evaluated by orthopedic surgery, oncology, and urology. He was immediately started on an intravenous pain regimen. After ruling out spinal cord compression, he was admitted for oncology staging and initiation of therapy. After a complete evaluation, the patient was discharged with an outpatient oncology follow-up recommendation to receive palliative radiation for pain management. He continued to follow up with his primary care physician for additional supportive care.
Ethics Statement
The patient provided consent for the publication of this case.
Red Flags and Legal Pitfalls
- Sending a patient with red flag signs/symptoms including back pain, weakness, and urinary incontinence home instead of an immediate ED transfer can result in a delayed diagnosis and management.
- A delayed diagnosis of a pathological fracture can occur when localized bone pain is dismissed or appropriate imaging is not obtained.
- When considering analgesia, weigh risks and benefits as well as degree of pain. A combination of acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) is appropriate for most with consideration of potential side effects of NSAIDs. A short acting opioid would be appropriate in those with a higher degree of pain caused by metastatic disease.
- A lack of a follow-up plan, including the need for ED transfer and referrals to orthopedics, neurosurgery, and oncology, can compromise timely patient care.
Takeaway Points
- The physical exam is important, and providers should pay close attention to red flag findings such as motor and sensory deficits, including hyporeflexia, muscle weakness, saddle anesthesia, and gait abnormalities.
- Persistent, non-mechanical back pain in an older male with up-trending PSA in the medical history is highly suspicious for metastatic prostate cancer.
- Prevention of pathological fracture, adequate pain management, and immediate transfer to the ED is essential for further evaluation.
- Avoid relying solely on radiographs to rule out underlying pathology, as they have significant lower diagnostic accuracy compared to MRI.
Manuscript submitted April 29, 2025; accepted July 23, 2025.
References
- [1]. Weber KL. Evaluation of the adult patient (aged> 40 years) with a destructive bone lesion. JAAOS-J Am Acad Orthop Surg. 2010;18(3):169-179.
- [2]. Osborn JL, Getzenberg RH, Trump DL. Spinal cord compression in prostate cancer. J Neurooncol. 1995;23(2):135-147. doi:10.1007/BF01053418.
- [3]. Wang J. Characterization of metastatic spinal cord compression from prostate cancer. J Clin Oncol. 2020;38(6_suppl):248. doi:10.1200/JCO.2020.38.6_suppl.248.
- [4]. Kingsley, L.A.; Fournier, P.G.J.; Chirgwin, J.M.; Guise, T.A. Molecular Biology of Bone Metastasis. Mol. Cancer Ther. 2007, 6, 2609–2617.
- [5]. Drzymalski DM, Oh W, Werner L, Regan MM, Kantoff P, Tuli, S. Predictors of survival in patients with prostate cancer and spinal metastasis: Presented at the 2009 Joint Spine Section Meeting. J. Neurosurg. Spine 2010, 13, 789–794.
- [6]. Maccauro G, Spinelli MS, Mauro S, Perisano C, Graci C, Rosa MA. Physiopathology of spine metastasis. Int J Surg Oncol. 2011;2011(1):107969.
- [7]. DePalma MG. Red flags of low back pain. Jaapa. 2020;33(8):8-11.
- [8]. Yáñez ML, Miller JJ, Batchelor TT. Diagnosis and treatment of epidural metastases. Cancer. 2017;123(7):1106-1114.
- [9]. Tsuzuki S, Park SH, Eber MR, Peters CM, Shiozawa Y. Skeletal complications in cancer patients with bone metastases. Int J Urol. 2016;23(10):825-832.
- [10]. Bhattacharyya S. Spinal cord disorders: myelopathy. Am J Med. 2018;131(11):1293-1297.
- [11]. Todd NV. Quantifying the clinical aspects of the cauda equina syndrome–The Cauda Scale (TCS). Br J Neurosurg. 2018;32(3):260-263.
- [12]. Ito Z, Harada A, Matsui Y, et al. Can you diagnose for vertebral fracture correctly by plain X-ray?. Osteoporos Int. 2006;17(11):1584-1591. doi:10.1007/s00198-006-0123-0.
- [13]. Thoma C. PSMA PET–CT outperforms conventional imaging in high-risk prostate cancer. Nat Rev Urol. 2020;17(6):319-319.
- [14]. Loblaw DA, Laperriere NJ. Emergency treatment of malignant extradural spinal cord compression: an evidence-based guideline. J Clin Oncol. 1998;16(4):1613-1624.
- [15]. Gould Rothberg BE, Quest TE, Yeung SJ, et al. Oncologic emergencies and urgencies: A comprehensive review. CA Cancer J Clin. 2022;72(6):570-593.
- [16]. Vos T, Allen C, Arora M, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545-1602.
- [17]. Dubosh NM, Edlow JA, Goto T, Camargo Jr CA, Hasegawa K. Missed serious neurologic conditions in emergency department patients discharged with nonspecific diagnoses of headache or back pain. Ann Emerg Med. 2019;74(4):549-561.
- [18]. Malviya A, Gerrand C. Evidence for orthopaedic surgery in the treatment of metastatic bone disease of the extremities: a review article. Palliat Med. 2012;26(6):788-796.
- [19]. Agarwal MG, Nayak P. Management of skeletal metastases: an orthopaedic surgeon’s guide. Indian J Orthop. 2015;49(1):83-100.
- [20]. Archer Goode E, Wang N, Munkley J. Prostate cancer bone metastases biology and clinical management. Oncol Lett. 2023;25(4):1-18.
- [21]. Sevimli R, Korkmaz MF. Analysis of orthopedic surgery of patients with metastatic bone tumors and pathological fractures. J Int Med Res. 2018;46(8):3262-3267.
- [22]. Benjamin R. Neurologic complications of prostate cancer. Am Fam Physician. 2002;65(9):1834-1841.
- [23]. Lee CC, Tey J, Cheo T, et al. Outcomes of patients with spinal metastases from prostate cancer treated with conventionally-fractionated external beam radiation therapy. Glob Spine J. 2023;13(2):284-294.
Author Affiliations: Rimsha Afzal, MA, Kentucky College of Osteopathic Medicine, Pikeville, Kentucky. Gregory M. Thompson, MD, Adena Cancer Center, Chillicothe, Ohio. Authors have no relevant financial relationships with any ineligible companies.
Read More
- Escalating Back Pain Leading to a Diagnosis of ST-Elevation Myocardial Infarction (STEMI) in Urgent Care: A Case Report
- Back Pain, an Urgent Care Visit—and a Devastating Outcome
