Click Here to download the PDF
Urgent message: By the time an adverse outcome occurs in the urgent care center, it’s too late to go back and ensure the documentation reflects the care the patient received.
Lyndsie Pfeifer, DO; Marta Fratczak, Kinkela Harkins, and Michael Weinstock, MD
Citation: Pfeifer L, Fratczak M, Harkins K, Weinstock M. Back pain, an urgent care visit—and a devastating outcome. J Urgent Care Med. 2023;17(8):13-17.
Key words: back pain, documentation
INTRODUCTION
It’s easy to let our guard down when it comes to common complaints, such as back pain. Conversely, sometimes we complete a thorough evaluation—but our excellent data-gathering is not reflected in the documentation.
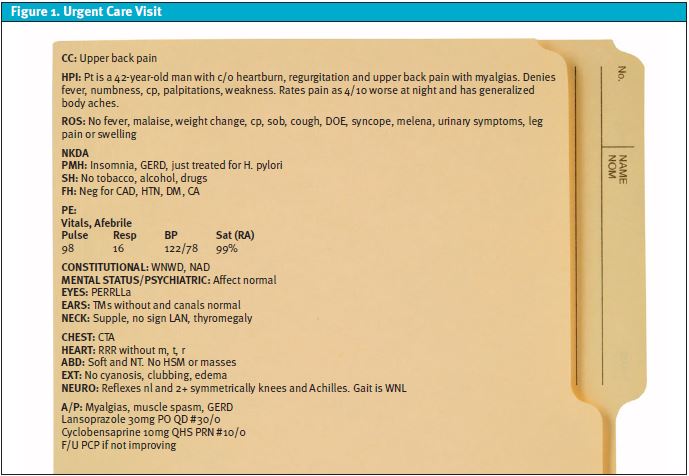
Discussion of the evaluation and documentation of patients with back pain is framed around the following case, with actual documentation reflected below.
THE PATIENT’S STORY
A 42-year-old man, sees his luck begin to turn when he is granted permission to immigrate to America. Having escaped the hardships of war and endured 8 months in a Somali refugee camp, Mohammed is ready to start his journey toward a new and improved life.
In America, he succeeds in finding a job at a distribution center, securing a yearly salary, health benefits, and a newfound sense of accomplishment. In spite of settling into a better life, however, old habits and hobbies begin to return, including playing soccer and, unfortunately, drug use. With increased exertion during soccer games, back pain begins to slow Mohammed down. Running on the field alongside teammates, Mohammed’s pain grows until he finally decides to make a visit to the urgent care clinic.1
THE URGENT CARE VISIT
(This is the actual documentation of the chart.)
DIFFERENTIAL DIAGNOSIS OF BACK PAIN
Back pain is a common presentation in the urgent care clinic; pain relief is often difficult to attain and finding the definitive cause proves to be even more elusive. In addition to common mechanical causes such as a strain, back pain can be the result of referred pain, originating from another area of the body.
A complaint-specific evaluation including a differential-based history and physical exam may shed light on serious underlying causes. The lifetime worldwide prevalence of low back pain is approximately 39%, with women 40 to 80 years of age being the highest-affected demographic group.2 Problems with ligaments, muscles, and joints are often responsible for chronic back pain. The differential diagnosis can be divided into two categories: mechanical and nonmechanical.
Mechanical causes of back pain
Low back pain is due to a mechanical cause 97% of the time, with lumbar strain accounting for 70% of cases.3 Originating from simple everyday overuse to traumatic injuries, lumbar strains and sprains often present with pain worse on movement, improvement with rest, and muscle tenderness. Other causes of mechanical back pain include degenerative disk and facet disease, followed by osteoporotic compression fractures, and spondylolisthesis; less than 1% of cases are due to traumatic fractures, congenital diseases, and spondylosis.3
Nonmechanical causes of low back pain
Nonmechanical conditions of the spine claim 1% of low back pain, with the most common condition being neoplasia.3 A broad categorization for low back pain includes hip problems, prostatitis and endometriosis, vascular disease such as an abdominal aortic aneurysm (AAA), or a systemic cause.4
Illnesses such as multiple myeloma, metastatic carcinoma, lymphoma and leukemia, spinal cord tumors, retroperitoneal tumors, and primary vertebral tumors account for 0.7% of nonmechanical low back pain cases. Inflammatory causes (specifically due to HLA-B27) make up 0.3% of low back pain presentations and include ankylosing spondylitis, psoriatic spondylitis, Reiter’s syndrome, inflammatory bowel disease, Scheuermann’s disease, and Paget’s disease of the bone.3
Red flags such as unexplained weight loss, immunocompromised state, intravenous drug use (IVDU), history of cancer or trauma, and long-term glucocorticoid use are associated with serious causes of back pain.4 At times, pain may be referred from other areas of the body—for example, the heart or aorta—and present as back pain.
Documentation of Patients with Back Pain
In training, a common teaching is to inquire about different elements of the chief complaint. A common mnemonic is OLD CAAARS:
- O – Onset
- L – Location
- D – Duration
- C – Character
- A – Alleviating/aggravating factors
- A – Associated symptoms (eg, dyspnea, diaphoresis, nausea/vomiting)
- A – Activity at onset
- R – Radiation
- S – Severity
However, this doesn’t always translate to our history-taking or documentation; sometimes, a history this extensive is unnecessary (for example, when we walk into the room and see grouped vesicles on an erythematous base in a dermatomal distribution). In a busy urgent care, inquiring about all these elements after the pathognomonic rash is visualized may be unnecessary. On the other hand, sometimes simply documenting each of these elements will be inadequate; consider a patient with a headache from carbon monoxide toxicity: we are not able to consider this problem until we gather additional documentation in a “diagnosis-specific” fashion (ie, asking about others with headache—Yes, my children also have headaches), when the headache occurs (worse in the morning and on weekends), and even the social history (a trailer heated with a generator located near a window).
The Front-Door, Back-Door Approach
We propose data gathering first in a symptom-based fashion; consider the chief complaint and proceed down the OLD CAAARS pathway.
Next, consider the differential and ask questions in a “diagnosis-specific” fashion to specifically exclude “can’t-miss” diagnoses. In other words, before leaving the room consider serious diagnoses, and make sure adequate data have been gathered to exclude them.
In the case above, neither of these approaches were used. Almost all of documentation was either omitted or extremely vague. With cases of back pain, we should attempt to exclude life-threatening causes of back pain, while ruling in a likely diagnosis.
In our patient, the most likely diagnosis was a muscle strain; we are not paid to be “usually right,” however. After the evaluation was completed and the patient discharged, life-threatening causes of back pain still included thoracic aortic dissection, pulmonary embolism, spinal cord compression from both infectious (our patient had a history of IVDU) and cancer-causing etiologies, ureteral stone, and acute coronary syndrome (ACS).
Back to Our Case: How Would the Front Door, Back Door Approach Have Helped the Clinician to an Accurate Diagnosis?
Front door (a symptom-based history):
O – Onset: Arguably, onset (the first component of the OLD CAAARS mnemonic) would have helped to either increase or decrease the suspicion of a “muscle spasm” (one of the diagnoses). If the pain started suddenly while playing soccer or with lifting/pushing/pulling then a muscular etiology would be more likely. If it started during exertion, such as when climbing the stairs or walking/jogging, then a cardiac etiology could be considered.
L – Location: If the pain was midline, then a more concerning etiology such as a spinal epidural abscess (SEA)5 or thoracic aortic dissection (TAD)6 could be considered, but if lateral at the site of a muscle, such as the trapezoid, then a more benign muscular etiology would be more likely.
D – Duration: If present for just a few days and if started with a burning/hyperesthesia feeling, consider herpes zoster. If present for years, a TAD or ACS is much less likely. Correlating the duration with the onset might help to exclude entities such as SEA which would be more likely to manifest within several days and have a gradual onset.
C – Character: A sharp pain would make ACS less likely and increase the suspicion for musculoskeletal or pulmonary embolism (PE).
A – Alleviating/aggravating factors: Pain worse with range of motion suggests musculoskeletal, not simply from a muscle strain but could also be from discitis, osteomyelitis, fracture (with history of trauma) or SEA.
A – Associated symptoms: A very important part of our evaluation is the question; back pain and…
- Back pain and fever increase suspicion of osteomyelitis, SEA, and pyelonephritis
- Back pain and shortness of breath and/or sweating increase concern for ACS
- Back pain and weight loss would increase the risk of malignancy
- Back pain and history of IVDU (as was the case in our patient) increase the risk of osteomyelitis and SEA as well as pulmonary abscess and endocarditis
A – Activity at onset: Our patient played soccer, but did the pain start with a particularly rigorous kick of the soccer ball, or with the exertion of running up and down the field?
R – Radiation
SUMMARY
Reading through the HPI again (the actual documentation from the chart) we see that almost none of these elements are explored. It is certainly hard to make a diagnosis when there are not adequate data to evaluate. With back pain, diagnosing a strain/spasm is usually right—but “usually right” is not even close to good enough for our urgent care patients!
Back door (a diagnosis-based history)
After we explore the chief complaint of back pain as above (OLD CAAARS or other memory aide), but before the patient leaves the urgent care, we need to consider which “can’t miss” diagnoses could still be occurring. Formulating this differential will help us to consider diagnoses which would not be considered simply by gathering more data on back pain. For example, we might get a lot of info on back pain, but never really consider ACS until we think about an expanded differential as the pain from coronary ischemia can certainly be referred to the back, neck, arm, jaw. Following is a list of possible diagnoses for our patient:
- Thoracic aortic dissection
- Pulmonary embolism
- Spinal epidural abscess
- Malignancy (renal cancer or lung cancer)
- Osteolytic lesion
- Ureteral stone
- Pyelonephritis
- Pneumonia
- Acute coronary syndrome
It does not seem as though the treating clinician considered many (or any) of these diagnoses. Not only does their history and exam lack evaluation for serious causes of back pain, but these are not detailed in a medical decision making (MDM) note.
The Physical Exam
The physical exam documentation should include skin findings, palpation, percussion, and range-of-motion if applicable. Because so many internal organ systems coalesce in the thorax and nervous innervation can be radiated to the back, the differential is extensive (as noted previously). Looking at the chart, we do not see that these were done—in fact, despite a chief complaint of back pain, there was not even documentation of a cursory back exam.
MEDICAL DECISION-MAKING
In the primary care setting, ruling out life-threatening diagnoses buys you one thing: time. Time to utilize treatment of the likely diagnosis (back strain) and to have the patient return or follow up with a primary care clinician if the symptoms do not resolve or if they change or worsen. However, when in the urgent care setting, follow-up may be less defined, and most patients are not known to the clinician, as would be the case with a primary care patient who has been receiving care for years or decades.
This is why knowledge of the life-threatening causes of back pain (differential) and how to rule them out (bedside evaluation and possibly testing) is the best way to keep patients safe; and this should be reflected in the MDM. Using the MDM as a “hard stop” can allow for consideration of serious causes before the patient leaves the urgent care; after completion of the MDM, note whether “can’t miss” causes have been considered and evaluated for and excluded to a high degree of likelihood. If not, return to the bedside for further data gathering.
For example, if a patient’s history denies any loss of ability to control bowel or bladder, and there are no gluteal or lower extremity paresthesias, it is unlikely that cauda equina syndrome is present. In a patient with back pain who does not have a fever or a history of IVDU, there is even more support that this diagnosis is unlikely and an MRI is not necessary to be done emergently.
In our patient, we lack the data or cauda equina symptoms—and he did have increased risk with history of IVDU. Unfortunately, the clinician did not explain why they thought this was not occurring. Additionally, considering the diagnosis of ACS, there is no mention of exertional pain, diaphoresis, radiation, and there was no ECG, imaging, or other evaluation of a serious cause of pain. Whether a mental or physical list is made, the top differentials and how to rule them out are paramount to making a diagnosis and treating the patient.
OUTCOME OF THE CASE
Two hours after his urgent care visit, Mohammed arrives at the emergency department by EMS following witnessed cardiac arrest. EMS reports police were performing CPR at the scene and the patient has been going in and out of ventricular tachycardia and pulseless electrical activity. The patient has undergone multiple defibrillations alongside multiple administrations of epinephrine, amiodarone, and atropine.
Once in the ED, CPR continues and he is intubated. After two more rounds of epinephrine and defibrillation for ventricular fibrillation, a sinus rhythm is seen and a femoral pulse is able to be palpated. Respiratory metabolic acidosis is found and treated with mechanical hyperventilation and sodium bicarbonate. Cardiology is consulted and the patient undergoes cardiac catheterization.
Following catheterization, he is found to have a complete occlusion of the proximal left anterior descending coronary artery. Despite rescue percutaneous intervention and drug-eluting stent placement, neurology and the intensive care unit are consulted for anoxic injury. Mohammed is later pronounced brain dead and life support is withdrawn with no palpable pulses, cardiac activity, or spontaneous respirations.1
DISCUSSION OF ACUTE CORONARY SYNDROME AND UNUSUAL PRESENTATIONS
While as few as 10% out of more than 8 million patients per year will be diagnosed with ACS after presenting to the ED with acute chest pain, it is important to include ACS in the differential.7
Classic cardiac chest pain is considered to be a retrosternal, left anterior chest crushing, squeezing, tightness, or pressure accompanied by radiation to the arms, neck or jaw; diaphoresis; dyspnea; and nausea or vomiting with the pain being worsened by exertion and relieved by rest with a duration of 2 to 10 minutes for anginal pain, 10 to 30 minutes for unstable anginal pain, and greater than 30 minutes for acute myocardial infarction pain.8 However, this presentation is widely affected by sex, race, age, and concurrent medical conditions.8-10
Nonclassic presentations are surprisingly common with up to 33% of ACS patients presenting without chest pain; these nonclassical complaints include chest pain lasting for seconds instead of minutes to hours or constant pains that are not relieved by rest and aggravated by exertion, burning pain described as similar to heartburn, epigastric pain, and back pain.11
Additional unusual complaints are chest pain worsened by specific body movements or positions, such as twisting and turning of the thorax. In stark contrast to the typical description of pressure or tightness of the chest, 22% of patients with acute myocardial infarction described their chest pain as sharp or stabbing.5 It is important to be aware that unusual presentations of ACS occur more frequently in patients who are genetically female, racial minorities, the elderly, diabetics, or present with altered mental status.10,12
With so many factors altering the likelihood of classical symptoms, it is clear that ACS cannot be ruled out with confidence on the basis of their absence.13 In maintaining a high clinical suspicion for ACS with uncommon presentations, we can work toward missing fewer cases that lead to devastating consequences for patient’s, and their family’s, lives such as in Mohammed’s story.
In summary, back pain is a very common ailment we see frequently and that can seem rather simple to diagnose and treat. As providers, we need to keep a broad differential, know the red flag warning signs, and how to identify those in patients efficiently and accurately. Patient’s lives like Mohammed depend on it.
(This article has been adapted from a case published in Bouncebacks! Critical Care. Columbus, OH: Anadem Publishing; 2021.)
REFERENCES
- Horan C. A 42-year-old man with history of IVDU and upper back pain. In: Weinstock MB, ed. Bouncebacks! Critical Care. Columbus, OH: Anadem Publishing; 2021.
- Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028-2037.
- Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344(5):363-370.
- Chiarotto A, Koes BW. Nonspecific low back pain. N Engl J Med. 2022;386(18):1732-1740.
- Weinstock M, Pilcher C. A legal quandary: poor care…or malpractice? J Urgent Care Med. 2022;16(4):13-15.
- Grock A, Weinstock MB, Jhun P, Herbert M. Aortic dissection! Or is it? Sigh. Ann Emerg Med. 2016;68(5):640-642.
- Fanaroff AC, Rymer JA, Goldstein SA, et al. Does this patient with chest pain have acute coronary syndrome? The rational clinical examination systematic review. JAMA. 2015;314(18):1955-1965.
- Swap CJ, Nagurney JT. Value and limitations of chest pain history in the evaluation of patients with suspected acute coronary syndromes. JAMA. 2005; 294:2623-2629.
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137:e67.
- Canto JG, Goldberg RJ, Hand MM, et al. Symptom presentation of women with acute coronary syndromes: myth vs reality. Arch Intern Med. 2007;167:2405-2413.
- DeVon HA, Mirzaei S, Zègre-Hemsey J. Typical and atypical symptoms of acute coronary syndrome: time to retire the terms? JAMA. 2020;9(7):e015539.
- Canto JG, Shlipak MG, Rogers WJ et al. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000;283(24): 3223-3229.
- Oliver G, Reynard C, Morris N, Body R. Can emergency physician gestalt ‘rule in’ or ‘rule out’ acute coronary syndrome: validation in a multicenter prospective diagnostic cohort study. Acad Emerg Med. 2020;27(1):24-30.

