Published on
Urgent message: Although chest pain in young adults is often benign, it is important to realize that emergency cases can sometimes be disguised as normal examination findings in adults.
ZANA ALATTAR and JOHN SHUFELDT, MD, JD, MBA, FACEP
This case demonstrates the importance of considering and ruling out rare cases of aortic dissection in patients with chest pain. We describe a case illustrating the approach to the management and work-up of chest pain in young patients to identify the underlying cause.
Case Presentation
A 44-year-old woman presented to an urgent care center reporting sudden-onset chest pain that had started the prior evening. On initial evaluation, the patient reported constant and worsening pain since onset, describing it as a “squeezing” pain associated with nausea and a single episode of vomiting.
Physical Examination
The initial physical examination revealed a patient in no acute distress and with stable vital signs as follows:
- Temperature: 36.7°C
- Heart rate: 78 beats/min
- Noninvasive systolic blood pressure: 135 mm Hg
- Noninvasive diastolic blood pressure: 70 mm Hg
- Respiratory rate: 16 breaths/min
- O2 saturation: 97% on room air
Her lungs were clear to auscultation bilaterally, respirations were not labored, and breath sounds were equal. The cardiovascular examination revealed normal peripheral perfusion and a regular heart rate and rhythm without murmur. The chest wall was tender to palpation, which was consistent with her report. The abdomen and back were nontender. The neurologic examination showed no focal neurologic deficit; that cranial nerves II through XII were intact; and normal sensory, motor, speech, and coordination findings.
The patient’s past medical history was significant for patent foramen ovale, transient ischemic attack, mitral valve prolapse, and atrial fibrillation with cardiac ablation 5 years earlier. Her social history was negative for alcohol, tobacco, or drugs of abuse. Her family history revealed that her mother had significant coronary artery disease.
Diagnostic Results
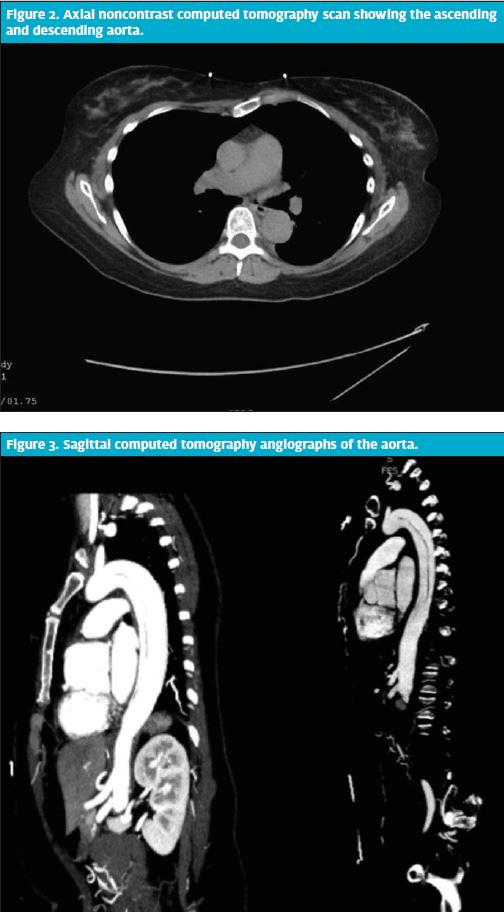
An electrocardiogram showed no acute changes. Findings on laboratory tests, including complete blood count, basic metabolic panel, and cardiac enzymes, were normal. However, a chest x-ray (Figure 1) showed an enlarged aortic knob, which concerned the urgent care provider and prompted transfer to an emergency department (ED) for further evaluation.
On ED presentation, the patient continued to report chest pain to the left anterior chest, radiating to the left upper back and left side of neck. She described a sharp, stabbing pain with associated diaphoresis, shortness of breath, and near syncope at time of onset. Upon further questioning, the patient described constant and worsening pain throughout the night that prevented her from sleeping, with associated nausea, diaphoresis, and a single episode of vomiting. She reported no pain relief with aspirin or Tylenol with Codeine, both of which she took prior to her visit.
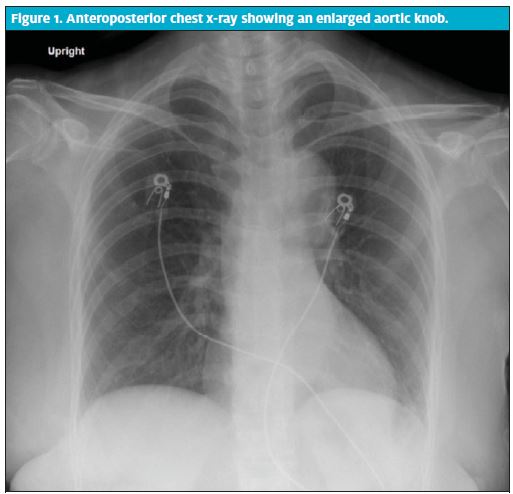
A noncontrast computed tomography (CT) scan of the chest, abdomen, and pelvis revealed an aortic dissection arising just distal to the left subclavian artery and extending through the descending aorta. Bilateral blood pressures were measured and found to be equal at 97 mm Hg/54 mm Hg on the right and 99 mm Hg/54 mm Hg on the left.
CT angiography of the aorta revealed a type B aortic dissection and a 4.3-cm aneurysmal dilation of the aortic root (Figures 2 and 3).
Diagnosis
Aortic dissection, Stanford type B.
Course and Treatment
Further questioning revealed that the patient’s brother had a history of Marfan syndrome and that her father died of cardiac arrest at the age of 52. The patient remained in the intensive care unit under close observation and medical management for 2 days until the hemodynamic goal was achieved and she was in stable enough condition to be transferred to the medical floor. With continued use of blockers and with consults from cardiology and cardiothoracic surgery, the patient’s condition remained stable and the dissection did not extend. After a 5-day admission, the patient was prescribed aggressive blockers and lisinopril, advised to follow up with cardiology and cardiothoracic surgery, and discharged home.
Overview
An aortic dissection is a tear in the lining of the aorta, which causes a change in blood flow from the normal arterial pathway. Relatively uncommon, this condition is frequently misdiagnosed and has a high mortality rate. Aortic dissections are three times more common in men than women and about 75% of the time, they are found in patients between the ages of 40 and 70 years.3 Risk factors for the condition include hypertension, atherosclerosis, hypercholesterolemia, smoking, and certain inherited disorders, such as Marfan syndrome and Ehlers-Danlos syndrome.1
Aortic dissection should be considered whenever there are risk factors and telltale clinical signs from the medical history and physical examination. The patient typically presents with severe, sharp, or “tearing” chest pain from a location that depends on the type of dissection. Ascending aortic dissections typically present as anterior chest pain, whereas dissections distal to the left subclavian present as posterior chest or back pain. With either type, if the dissection has progressed to the point of impairing or preventing blood flow to peripheral vessels, the physical examination may reveal weakened or absent carotid, brachial, or femoral pulses unilaterally or bilaterally.2
Take-Home Points
This case of aortic dissection was easy to miss. The patient was thin, nonsmoking, and athletic and had normal findings on electrocardiography. Moreover, she had somewhat reproducible chest wall pain. The key to this case was the correct and timely identification of the enlarged aortic knob on the chest x-ray and then linking this finding to the possibility of a dissection. Although the family history in this case provided a critically important clue, it took obtaining histories via 3 separate providers before it was revealed that her brother had Marfan syndrome and that her father experienced sudden cardiac death.
References
- Creager M, Loscalzo J. Diseases of the aorta. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, eds. Harrison’s Principles of Internal Medicine. 17th edition. New York, New York: McGraw-Hill Medical; 2008: 1563–1567.
- Hansen MS, Nogareda GJ, Hutachison SJ. Frequency of and inappropriate treatment of misdiagnosis of acute aortic dissection. Am J Cardiol. 2007;99:852–856.
- Younus F. Aortic dissection. A diagnosis not to be missed: case report and review. Federal Practitioner. 2001;15:36–42.