Published on
Differential Diagnosis
- Hyperkalemia
- Hypokalemia
- Digoxin toxicity
- Myocardial infarction
- Myocarditis
ECG Analysis
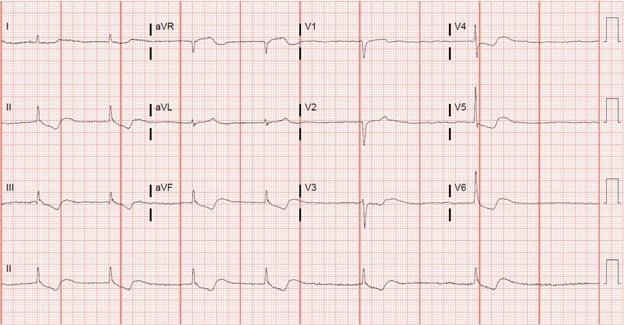
This ECG shows atrial fibrillation with a rate of 36 bpm. There is a narrow QRS interval followed by downsloping, “scooped” ST-segments predominantly seen in the anterolateral and inferior leads (resembling Salvadore Dalí’s mustache)—a finding that does not necessarily imply toxicity. These scooped ST-segments are followed by a biphasic t-wave, with an initial negative deflection and terminal positive deflection.
Overall, the findings of slow atrial fibrillation and the scooped ST-segments are consistent with digoxin toxicity.
Derangements in serum potassium can cause a variety of changes to the ECG. ECG changes due to hyperkalemia include peaked T-waves, P-wave flattening, prolonged PR interval, widened/abnormal QRS morphology, bradyarrhythmias, and a sine wave appearance. Changes due to hypokalemia include prolongation of the PR interval, ST depressions, T-wave flattening/inversion, U-waves, and an appearance of a long QT interval (due to fusion of the T- and U-waves).
The combination of features that favor digoxin toxicity include atrial fibrillation, narrow complex QRS interval, and a “scooped” morphology of the ST-segments. While ischemia and/or myocarditis can cause ST-segment changes, neither the history nor the ST-segment morphology supports these diagnoses.
Discussion
Digoxin is a cardiac glycoside most commonly used in the management of systolic heart failure and atrial arrhythmias. It is a reversible inhibitor of the Na-K ATPase pump, primarily in the myocardium, leading to increased intracellular calcium and enhanced contractility. In toxic doses, digoxin can cause a multitude of arrhythmias owing to increased automaticity, shortened refractory period, and decreased AV nodal conduction.
Digoxin toxicity can cause virtually any dysrhythmia, but common dysrhythmias associated with digoxin toxicity are: frequent PVCs, slow atrial fibrillation, sinus bradycardia, junctional rhythm, atrial tachycardia, AV blocks, and ventricular tachycardia (bidirectional or polymorphic).
Digoxin toxicity can be acute (accidental or nonaccidental overdose) or chronic, typically associated with renal failure, drug-drug interactions, or supratherapeutic dosing. Digoxin toxicity affects multiple organ systems and can manifest clinically as nausea/vomiting, anorexia, blurry vision, yellow/green color disturbances, seeing halos, palpitations, syncope, confusion, dizziness, hallucinations, and fatigue.
The mainstay of treatment is digoxin-specific antibody fragments (Fab) and is indicated with cardiac manifestations of toxicity. Additionally, concurrent derangements to serum potassium can be seen in digoxin toxicity and must be carefully monitored/managed.
Learnings/What to Look for
- Downsloping, scooped ST-segments resembling Salvadore Dalí’s mustache are a common ECG effect of digoxin and do not (in and of themselves) imply toxicity
- Digoxin toxicity can cause virtually any dysrhythmia, and toxicity is a life-threatening condition
- A careful medication history should be taken to help identify potential digoxin toxicity
- Digoxin toxicity can present with both cardiac and extracardiac manifestations
Pearls for Initial Management and Considerations for Transfer
- Urgent care patients in whom digoxin toxicity is a possibility should be emergently transferred to a facility capable of administering digoxin-specific antibody fragments
- Serum digoxin levels do not always correlate with degree of clinical toxicity
- Identify potential concomitant potassium derangements early in the resuscitation and correct them
- Intravenous atropine or transcutaneous cardiac pacing may be used in patients with high grade symptomatic AV blockade
Resources
- Ehle M, Patel C, Giugliano R. Digoxin: clinical highlights: a review of digoxin and its use in contemporary medicine. Crit Pathw Cardiol. 2011;10(2):93-98.
- Gheorghiade M, Adams KF Jr, Colucci WS. Digoxin in the management of cardiovascular disorders. Circulation. 2004;109(24):2959–2964.

