Urgent message: This case underscores the importance of not “anchoring” to a previous provider’s diagnosis and always remembering that medical conditions are dynamic.
JOHN J. KOEHLER, MD, and DANIEL MURAUSKI, DO
Introduction
Acute pericarditis is defined as inflammation of the pericardium that surrounds the heart and the base of the great vessels. The classical presentation consists of chest pain, a pericardial friction rub, and serial changes on electrocardiogram (EKG). Although data on the incidence of pericarditis are lacking, estimates indicate that it is the cause of at least 1% of emergency room (ER) visits among patients with ST-segment elevation and up to 5% of ER visits for nonischemic chest pain.1,2
Case Presentation
A 57-year-old woman presented with persistent “chest congestion” starting 4 days prior. One day after onset of symptoms, she had seen her primary care physician, who diagnosed an upper respiratory tract infection (URI) and provided a “Z pack.” The patient reported no past medical or surgical history and takes no medications other than the recently prescribed antibiotic.
On further questioning, the woman reported experiencing sharp sub-sternal chest pain that radiated into her back. It was made worse with deep breathing and lying flat. She noted mild relief after taking acetaminophen, which she took 4 hours before presentation. On review of systems, the patient reported fever, chills, malaise, and a headache. She denied sore throat, nasal congestion, body aches, cough or ear pain.
Further evaluation of the patient revealed the following vital signs:
T 99.2°F
BP 90/60 mmHg
P 106 bpm
RR 16
O2 Sat 97%
She did not appear toxic and her exam was normal expect for trace amounts of clear nasal discharge with some mild cobble stoning in her oral pharynx. A rapid flu test was negative.
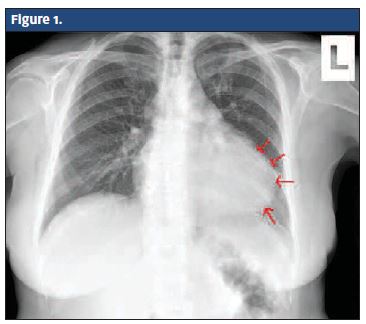
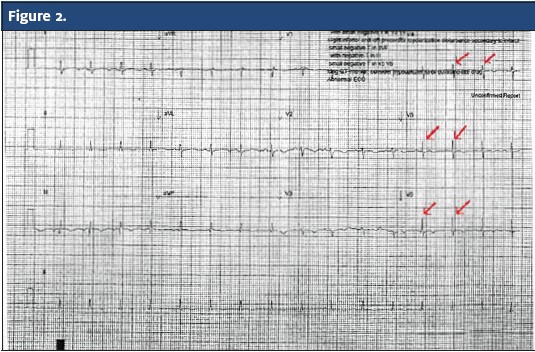
The patient’s chest x-ray (Figure 1) showed an abnormal “globular”-appearing heart with a left-sided pleural effusion. Her EKG (Figure 2) demonstrated poor R wave progression and T waves that had become diffusely flattened and inverted.
Disposition
Given the patient’s history and clinical findings, she was referred to the ER for suspected pericarditis with constrictive pericardial effusion. Surgical drainage of the effusion was successful without complication and she was discharged 5 days post admission.
Discussion
Although viral infection is the most common identifiable cause of acute pericarditis, there are multiple other etiologies, as listed in Table 1.3,4
| Table 1. Etiologies of Acute Pericarditis |
|
SLE – systemic lupus erythematosus
The classic history of acute pericarditis begins with prodromal symptoms of fever, myalgia, and malaise. It is followed by acute onset of pleuritic, substernal chest pain that may radiate to the scapular ridge, neck, arms or jaw. The pain is usually relieved by leaning forward and made worse with laying supine.3 Other associated symptoms include low-grade intermittent fever, dyspnea, tachypnea, cough and dysphagia.
A pericardial friction rub is the most specific physical exam finding in pericarditis (specificity approaching 100%), however, this exam finding is transient over time, has a low sensitivity, and may be present in only about 50% of cases.3,4 The rub is best heard over the left sterna border, during expiration with the patient leaning forward. It is characterized by a grating or rasping sound similar to leather rubbing together.3,5
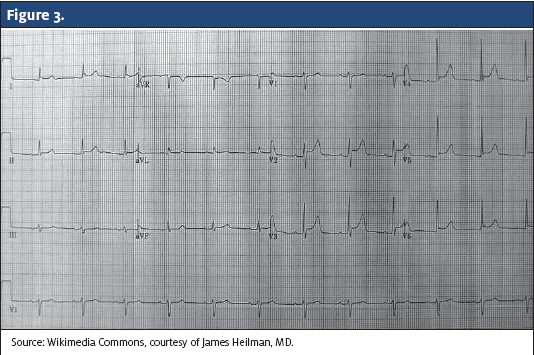
A major life-threatening complication of acute pericarditis is cardiac tamponade. Pericardial effusion results from accumulation of fluid between the visceral and parietal layer of the pericardium. Tamponade occurs when the fluid pressure in the intrapericardial space alters cardiac filling. The classic signs as described by Beck’s Triad are hypotension, jugular venous distension, and muffled heart sounds. Another important physical exam finding is pulsus paradoxus, a drop of at least 10 mmHg in arterial blood pressure on inspiration.3,5 ECG changes include low-voltage ORS complexes in the limb leads, poor R wave progression, and electrical alternans (Figure 3). Cardiac tamponade is a medical emergency and patients should be transferred to an emergency care setting for further evaluation.
During acute pericarditis, ECG changes evolve through four stages as described in Table 2.3,5,6 The hallmark ECG findings of diffusely concave upward ST elevation (not seen in V1 and aVR) with upright T waves, and a PR interval that deviates opposite of the P wave polarity are found during Stage I (Figure 3).3, 5 These acute findings were no longer apparent in our patient’s ECG. Instead, the ST segments had normalized and the T waves had become mostly inverted. The EKG presented here is most consistent with Stage III ECG changes of pericarditis with an underlying pericardial effusion.
| Table 2. Stages of ECG Changes During Acute Pericarditis |
Stage I: Stage III: Stage IV: Sources: Brady WJ et al1, Tingle TE, et al4, and Marinella MA7 |
Chest x-ray is usually normal in patients with pericarditis and minimal effusion. However, when a large amount of effusion is present (200-250 mL), a chest x-ray will reveal a flask-shaped, enlarged cardiac silhouette, and a possible left-sided pleural effusion.6 The chest x-ray taken of our patient demonstrated an enlarged cardiac silhouette with a “globular” appearance, which is consistent with a significant pericardial effusion. In this case, an echocardiogram would be warranted to further evaluate the significance of the effusion and assess cardiac function.
Treatment for pericarditis is directed toward the underlying cause. For idiopathic and viral pericarditis, therapy should be directed toward symptom control. Nonsteroidal anti-inflammatory drugs (NSAIDS) are the mainstay of therapy.2-5 Colchicine is a useful adjunct to NSAIDs and was once reserved for patient with recurrent or prolonged symptoms.5 Data from the Colchicine for Acute Pericarditis Trial has led to its routine use by many practioners.5 Corticosteroids are not recommended for first-line treatment unless indicated for the underlying disease or because of lack of response to NSAIDs or colchicine.2,5 NSAIDs and steroids should not be used in pericarditis associated with acute myocardial infarction (MI). Pericardiocentesis is indicated when significant pericardial effusion is present, for both diagnostic and therapeutic purposes.
Conclusion
This case highlights several important issues for urgent care providers. First is the danger of “anchoring” to the diagnosis of a prior provider. All patients presenting to urgent care deserve a full investigation of their chief complaint with an open mind as to the cause. The clinical presentation of the patient in this case warranted further investigation to rule out other significant disease processes, such as MI and pulmonary embolism.
The second important issue is that medical conditions are dynamic and evolve. While it may be tempting to criticize the first provider for having “missed” the diagnosis, we do not know if the key features of sharp positional chest pain, tachycardia, and subtle hypotension were present 4 days prior. A third key issue is to make sure the clinical presentation is consistent with the patient’s diagnosis. Several features make this case inconsistent with the original diagnosis of URI. The presence of positional pleuritic chest pain and subtle vital sign abnormalities and the absence of URI symptoms warranted the chest x-ray and EKG, which made the diagnosis obvious.
References
- Brady WJ, Perron AD, Martin ML, Beagle C, Aufderheide TP. Cause of ST segment abnormality in ED chest pain patients. AM J Emerg Med. 2001;19(1):25-28.
- Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet. 2004;363:717–727.
- Tingle TE, Molina D, Calvert CW. Acute Pericarditis. Am Fam Physician. 2007;76(10):1509-1514.
- Spodick DH. Acute Pericarditis: current concepts and practice. JAMA. 2003;289:1150–1153.
- Little WC, Freeman GL. Pericardial Disease. Circulation. 2006;113:1622-1632.
- Goyle KK, Walling AD. Diagnosing Pericarditis. Am Fam Physician. 2002:66(9):1695-1702.
- Marinella MA. Electrocardiographic manifestations and differential diagnosis of acute pericarditis. Am Fam Physician. 1998;57(4):699-704.