Published on
Urgent message: Acute aortic obstruction should be suspected in all patients with back pain and a history of peripheral vascular disease and atrial fibrillation, as over 50% of these cases are misdiagnosed, resulting in high mortality rates in affected patients.
Kristopher Palmer, DO and JM Alderson, DO
Introduction
Aortic occlusion is a rare but potentially fatal vascular phenomenon that must be considered in all patients with peripheral vascular disease (PVD) complaining of severe pain. Here, we present a case of acute infrarenal aortic occlusion in a 76-year-old female with severe PVD and chronic, untreated atrial fibrillation.
Case Presentation
A 76-year-old female presented with acute onset of chest, back, and bilateral lower extremity pain and right lower extremity weakness. Her physical examination was significant for severe, diffuse low back pain to palpation, mottling and coldness of the lower extremities bilaterally below the level of the knee, and absent dorsalis pedis and posterior tibial pulses. In addition, she demonstrated a very limited range of motion in her back and right lower extremity. She had an extensive past medical history that suggested severe PVD and risk factors for embolic disease that included type II diabetes, quadruple cardiac bypass surgery, DVT, CVA, severe pulmonary HTN, and atrial fibrillation. She had stopped taking her warfarin (Coumadin) several years ago secondary to finding blood in her urine at home. She denied any history of smoking.
Urgent Care Evaluation
Her serious clinical picture, combined with a blood pressure of 250/110, prompted rapid transfer by EMS. Given these objective findings and clinical presentation, differential diagnoses included aortic dissection, abdominal aortic aneurysm, stroke, hypertensive emergency, and aortic occlusion.
Her troponin was 0.84 in the ED. Chest x-ray findings were consistent with cardiomegaly and alveolar edema. Her ECG and echocardiogram revealed evidence of right heart strain with a right ventricular systolic pressure (RSVP) of 81. Brain CT was negative.
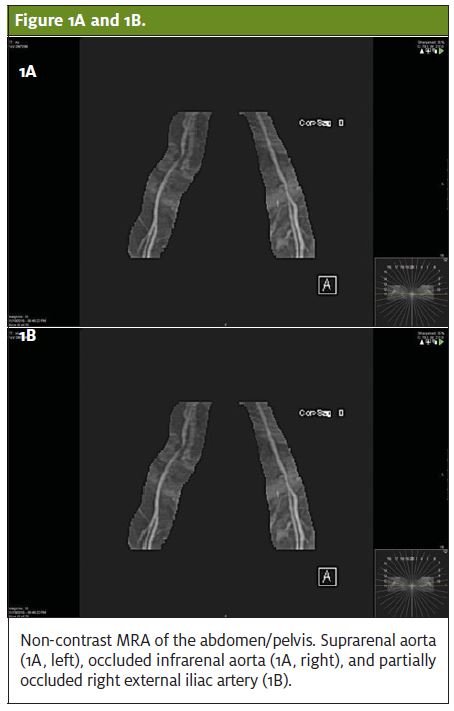
She was started on a heparin drip with consideration of pulmonary embolism, given her history of atrial fibrillation. The providers were reluctant to perform a CT angiogram as the creatinine was elevated, indicating acute renal failure. Venous Doppler could not locate pulses in the lower extremities, and the pain continued to worsen. Ankle-brachial index was 0.20, indicating severe vascular compromise. Magnetic resonance angiography of the abdomen and pelvis without contrast followed, showing nearly complete occlusion of the infrarenal aorta 1.6 cm proximal to the bifurcation without evidence of emboli and severe focal stenosis of the right external iliac artery (Figures 1A and 1B). There were multiple large lumbar collaterals present.
She underwent emergent aortogram with balloon angioplasty and stenting of the infrarenal aorta. Final imaging showed rapid blood flow through the stented segment. The postprocedure physical examination revealed palpable dorsalis pedis pulses, and both lower extremities felt warm to the touch. Unfortunately, the patient had minimal improvement in her lower extremity pain following the procedure. She was started on aspirin and Plavix daily.
Discussion
Acute abdominal aortic occlusion is a vascular emergency affecting 9% of people >65 years of age in the United States.1 The two most common causes of abdominal aortic occlusion are cardiac embolism (65%) and local thrombosis (35%).2
Atrial fibrillation and atherosclerotic cardiac disease are the greatest risk factors for embolism, while hypertension, diabetes, and smoking are the greatest risk factors for thrombosis.2,3
This patient most likely had severe stenosis of the abdominal aorta and external iliac arteries for many years, which went undetected due to sufficient collateral circulation from the lumbar arteries.
Over half of cases of aortic occlusion are misdiagnosed due to the nonspecific nature of the presenting symptoms, which include severe pain and/or sensory deficits in the lower extremities, acute paraplegia, abdominal pain, back pain, chest pain, acute hypertension, and acute renal failure.3 The mortality rate is 31%-52% within the first 24 hours if left untreated. Even if treated promptly, limb amputation may still result.4
Duplex scanning of the of the abdominal aorta, iliac, and femoral arteries is a simple, quick, and inexpensive test with a 91% sensitivity and 93% specificity for detecting abdominal aortic occlusion in severe occlusive disease and should be considered in patients with PVD presenting with concerning symptoms.4
Take home points for the urgent care clinician include:
- Atrial fibrillation, hypertension, and smoking increase the risk of acute aortic occlusion.
- Etiologies may be embolic or thrombotic.
- Acute occlusion is a surgical emergency requiring rapid identification in the urgent care center and rapid transfer to the hospital.
Citation: Palmer K, Alderson JM. Acute occlusion of the abdominal aorta in a patient with severe peripheral vascular disease and untreated atrial fibrillation. J Urgent Care Med. October 2017. Available at: https://www.jucm.com/acute-occlusion-abdominal-aorta-patient-severe-peripheral-vascular-disease-untreated-atrial-fibrillation/.
References
- Steckmeier B. Epidemiology of aortic disease: aneurysm, dissection, occlusion. 2001;41(8):624-632.
- Kilany A, Al-Hashel JY, Rady A. Acute aortic occlusion presenting as flaccid paraplegia. Case Rep Neurol Med. [Epub March 11, 2015]
- Matolo NM, Cheung L, Albo D Jr, Lazarus HM. Acute occlusion of the infrarenal aorta. Am J Surg. 1973;126(6):788-793.
- Efstratiadis G, Kirmizis D, Papazoglou K, et al. Nephrol Dial Transplant. 2004;19(1):227-229.


