Urgent message: Evaluation of chest pain in the low-risk patient can be daunting. This case, in which the patient had no known history of cardiovascular disease, exemplifies the challenge.
MARREN J. WEBER, DO
The standard treadmill exercise tolerance test (ETT) and echocardiography are widely used as the initial tests of choice for prediction of cardiovascular disease. Historically stress echocardiography has been recognized to perform well in predicting mortality in conjunction with clinical data and other risk stratification measures.1 However, while it remains a useful diagnostic tool, it is limited by a moderate predictive accuracy of 70%-90% (varying by modality), irrespective of patient subset.2
Case Presentation
VG is a 59-year-old male who presented to urgent care with a complaint of chest pain. His past medical history was significant only for acid reflux, and he had no known familial history of cardiac disease. He is a one- pack-per-day smoker seen annually by a primary care provider, although he had never had a screening stress test. At his first visit, his chest pain had been intermit- tent for about two weeks, sternal, and not associated with nausea, shortness of breath, radiation, or palpitations. His work-up included blood work (troponin negative) and an ECG (Figure 1), which showed T wave inver- sion in leads V2-V4 only (no previous ECG was available for comparison). The patient refused hospital admission, requesting an outpatient work-up instead. His TIMI score was 0. He was discharged with instructions to follow up with caridology.

Ten days later, VG presented again to urgent care with sternal chest pain. He stated that he had been seen by cardiology for the appropriate follow-up stress testing and was told it was normal. As before, he was not experiencing dyspnea or any radiation of his pain. Severity was rated at 7-9/10. His pain was dull or squeezing in character, and he noted some indigestion. Eating made his pain worse; the pain was unrelieved by taking omeprazole (Prilosec) or calcium carbonate (TUMS).
Observations and Findings
Evaluation of the patient revealed the following vital signs:
- BP: 153/94
- P: 79
- R: 20
- T: 97.5° F
- O2 sat: 99%
- Wt: 100 kg
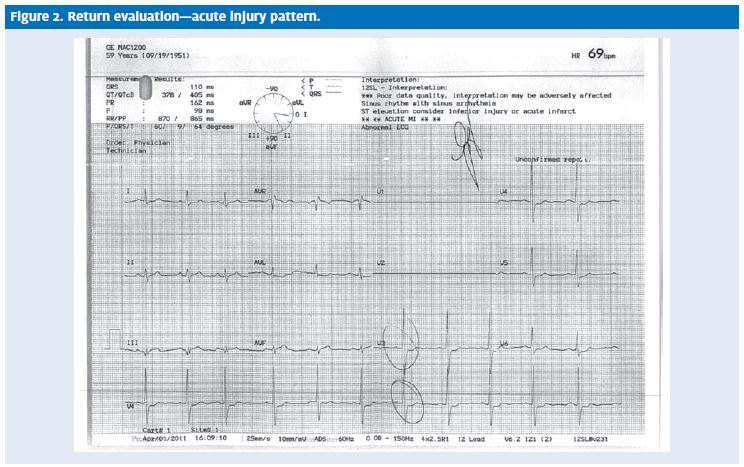
On examination, VG was in mild distress. His lungs were clear. He had no murmurs, no S3 or S4 rubs, and no jugular venous distention (JVD). His ECG (Figure 2 and Figure 3) showed ST depression >1 mm in leads V3 through V5, with flattening of the T wave.
The patient’s pain was relieved entirely after taking two 0.4mg SL nitroglycerin tablets and 4L O2 NC. How- ever, he then became clammy, diaphoretic, and significantly bradycardic at 38 bpm. He was transferred emergently to the nearest ED by EMS. His troponin results were subsequently found to be positive at 2.15.

Disposition
VG’s records were retrieved and his ETT was reviewed 6 days prior to his second urgent care visit. Following a standard Bruce protocol, the patient achieved 85% MPHR with normal wall motion, normal ejection fraction, and no ECG changes or chest pain. Resting EF was 65% and the stress test conclusion was normal.
Records from the admitting hospital show the patient was evaluated in the ED, where he had no chest pain. Cardiology was consulted and VG was admitted for cardiac catheterization. Cath results were:
- EF: 40%
- Akinetic inferobasal wall with moderate impairment to overall LV function
- Right coronary artery: 100% occlusion, stented
- Left anterior descending mid-portion: 99% occluded with a ruptured plaque, stented
Discussion
This case pointedly demonstrates the limitations in ETT as a prognostic test. ETT results are generally considered positive if the ECG shows 1 mm ST segment depression, horizontal or downsloping.3 The test is non-diagnostic if ischemic ST depression is absent but HR does not reach 85% of predicted maximum for age/gender, or if the ST changes were non-diagnostic (ST depression 0.5-0.9 mm, ST depression with slight upslope, or non-specific T wave abnormalities). The ETT’s predicted accuracy of approximately 70% is seen in multiple studies. There is, however, some controversy about its overall predictive value when combined with demographic and clinical data. In addition, there are subtle ECG measures relating to rate, conduction, left ventricular mass, and repolarization, which only moderately improve risk stratification, but which are predictive of long- term mortality.4 The four most significant are higher ventricular rate, more leftward QRS axis, more downward ST segment deviation, and longer QT interval, all of which can be present in a negative or nondiagnostic ETT.5
It is particularly difficult to stratify the low-risk patient with a clinically normal resting ECG. Of patients seen in the ED for acute chest pain, approximately 4%-5% with acute coronary syndrome (ACS) are inadvertently sent home.6 The push for accelerated diagnostic protocols (stress testing and echo within 48 hours of discharge) is to get physicians to stratify higher-risk patients promptly. However, inconclusive ETT results are relatively common,6 often requiring further diagnostic testing. In patients under age 40, with a prevalence of ACS of <2%, the use of ETT is of limited diagnostic utility.2 Finally, the accuracy of ETT is lower in women than in men, with a lower specificity, sensitivity, and positive predictive value.3
Conclusion
In evaluating chest pain in the urgent care patient with no known history of cardiovascular disease, the physician has many factors to consider. As this case demonstrates, even an echo stress test, while helpful for risk stratification, can be falsely negative. Clear commu- nication with the patient of all test results and their limitations is crit- ical when evaluating chest pain. Shared decision-making and good documentation are important as well. The emergence of multidetec- tor CT angiography, coronary artery calcium scores, serum markers of inflammation, and novel biomarkers of ischemia all hold prom- ise in the evaluation of the low-risk patient. Until their role is clarified, however, evaluating chest pain in low risk patients remains a daunting challenge. n
REFERENCES
- Rubinshtein R, Hallon DA, Gaspar T, et Usefulness of 64-slice multidetector computed tomography in diagnostic triage of patients with chest pain and negative or non-diagnostic exercise treadmill result. Am J Cardiol. 2007;99(7):925-929.
- Hermann L, Weingart S, Duvall WL, Henzlova The limited utility of routine cardiac stress testing in emer- gency department chest pain patients younger than 40 years. Ann Emerg Med. 2009;54(1):12-16.
- Morise AP, Diamond Comparison of the sensitivity and specificity of exercise electrocardiography in biased and unbiased populations of men and women. Am Heart J. 1995;130(4):741-747.
- Gorodeski E, Ishwaran H et Quantitative electrocardiographic measures and long-term mortality in exercise test patients with clinically normal resting electrocardiograms. Am Heart J. 2009;158(1):61-70.e1.
- Greenland P, Xie X, Liu K, et Impact of minor electrocardiographic ST-segment and/or T-wave abnormalities on cardiovascular mortality during long-term follow-up. Am J Cardiol. 2003;91(9):1068-1074.
- Nucifora G, Badano LP, Sarraf-Zadegan N, et Comparison of early dobutamine stress echocardiography and exercise electrocardiographic testing for management of patients presenting to the emergency departments with chest pain. Am J Cardiol. 2007;100(7):1068-1073.

