Published on
Urgent message: Working knowledge of anatomy and familiarity with radiograph reading, injury classification, treatment options, and criteria for referral support positive long-term outcomes in patients with acute ankle injuries.
Janet D. Little, MD and William E. Saar, DO
Acute ankle injury is one of the most common musculoskeletal injuries in the athlete and sedentary person alike. The yearly incidence of ankle injuries varies between resources, but ranges from 1 million to 5 million per year in the United States alone.1-3
Injuries to the ankle affect soft tissue and bone, both of which must be addressed upon presentation to the urgent care setting to avoid long-term complications and to ultimately restore normal anatomy and functionality. Systemic illness (e.g., diabetes), high body mass index, smoking, and prior ankle injury4,5 are all associated risk factors for ankle injuries and must be taken into account, as these may affect overall outcomes.
This article will provide a brief overview of ankle sprains, but will focus primarily on acute ankle fractures that result from minor trauma, including a basic approach to evaluation, management, and orthopedic referral of stable versus unstable ankle fractures.
Anatomy
During ambulation, the ankle joint must withstand 1.25–5.5 times the normal body weight, depending on the activity. Its motion involves dorsi and plantarflexion and internal and external rotation, as well as inversion and eversion because of its proximity to the subtalar joint.3 A thorough knowledge of the anatomic structures making up the ankle joint helps in the evaluation and management of acute injuries.
The bony anatomy of the ankle consists of the articulation of the distal tibia—medial malleolus and fibula—and the lateral malleolus with the talus.
The posterior aspect of the distal tibia is referred to as the posterior malleolus. The bones are held together by the ligaments of the ankle to form a mortise (Figure 1A and Figure 1B).

The lateral collateral ligamentous (LCL) complex consists of the anterior talofibular ligament (ATFL), the calcane ofibular ligament (CFL), and the posterior talofibular ligament (PTFL), with the ATFL and CFL being the two most commonly injured ligaments with ankle sprains.6,7
The medial ankle complex consists of the deep and superficial deltoid ligaments.
The syndesmosis of the ankle refers to the articulation of the distal tibia and fibula, providing support of the mortise and prevents separation of the distal tibia from the fibula. It consists of the sup porting structures of the anterior inferior tibiofibular ligament (AITFL), PITFL, and the interosseous mem- brane. Other supporting structures of the ankle include the peroneal tendons, anterior and posterior tibialis tendons, Achilles ten- don, and the joint capsule. The posterior tibial artery and tibial nerve run together in the posteromedial ankle “behind” the medial malleolus. The anterior tibial artery and deep peroneal nerve run together and cross the ankle joint anteriorly lateral to the extensor hallucis longus.
A simple classification scheme describes the ankle as a “ring” of supporting structures surrounding the talus, which may be ligamentous or osseous. The lateral aspect of the ring is made up of the lateral ligaments or the distal fibula. The deltoid ligaments or the medial malleolus make up the medial part of the ring, while the posterior malleolus or PITFL compromise the posterior portion.
Anteriorly, the primary support is the AITFL, capsule, and anterior tibial region.8 If the ring is compromised at one site, the injury is stable and can be managed nonoperatively; if the ring is broken at two or more sites, the injury is considered unstable and immediate orthopedic referral should be made.
History and Physical Examination
Physicians should inquire about the mechanism and time of the injury, a history of recurrent sprains, site of most significant pain, neurovascular symptoms, ability to bear weight immediately after injury, and related comorbidities (e.g., diabetes).
The immediate development of ankle swelling and severe pain suggest fracture, ligamentous disruption, or tendon rupture. Urgent evaluation and orthopedic referral is recommended with presentation of any of these symptoms along with the following signs of compartment syndrome:9
- pain out of proportion to injury
- pain with passive extension of digits
- pallor
- pulselessness
- paralysis
- paresthesia
- poikilothermia (cold extremity)
As previously mentioned, an inversion injury is the most common mechanism for sprain of the lateral ligaments, but may also precipitate other conditions, such as fifth metatarsal fractures, anterior process calcaneal fractures, and fractures of the lateral process of the talus.
Although less common, an ankle injury resulting from an eversion (pronation- external rotation) mechanism can result in fracture of the proximal fibula. Hence, physical examination should not be limited to the injured ankle alone. A systematic approach should include assessment of the knee, the en- tire length of the tibia and fibula, the medial and lateral malleoli, tibial plafond, the talus, the calcaneus, and the base of the fifth metatarsal.
The skin, ligamentous structures—including the LCL and syndesmotic liga- ments, as well as the tendinous structures (Achilles, peroneal, and medial flexors [PTT, FDL, and FHL])—should be assessed for their integrity, as well. Injury to the syndesmotic ligament causes pain just above the ankle with compression of the tibia and fibula.
Once emergent conditions have been excluded, one needs to assess if the ankle fracture is stable and can be managed nonoperatively, or if it is unstable and must be referred.
Criteria for a stable ankle fracture include:
Deciding when to use radiography for patients with ankle injuries. In an era of practicing “defensive medicine,” the rules have been shown to have sensitivities between 97% and 100%, with variable specificity, which has led to a decrease in use of ankle radiography, waiting times, and costs without patient dissatisfaction or missed fractures.11,12
Ankle radiograph series is required only if there is any pain in the malleolar zone and:
- isolated fractures of the lateral, medial or posterior malleolus
- non-displaced fractures
- not associated with a ligamentous
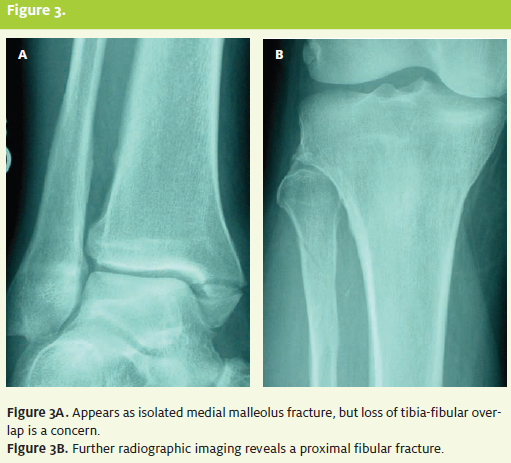
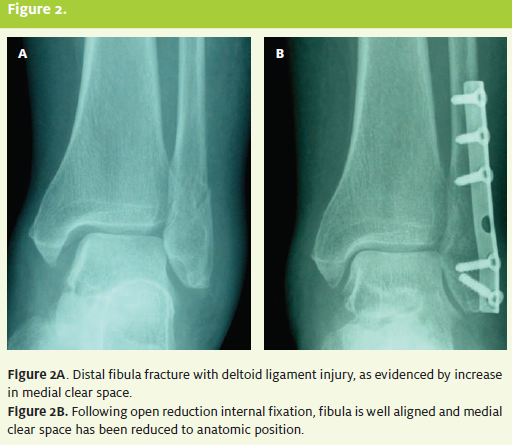
Isolated lateral and medial malleolar fractures are best seen on AP view. Posterior malleolar fractures are best seen on the lateral view. On the mortise view, the distances between the talus and the lateral malleolus, the talus and the medial malleolus, and the talus and the tibial plafond is known as the clear space, and should normally be equidistant through out. Deltoid ligament disruption is suggested if a distance greater than 5 mm of medial clear space exists. A lateral clear space of more than 2 mm or loss of overlap between the tibia and fibula suggests a syndesmotic injury. (See Figure 2A and Figure 2B.) The Maisonneuve fracture is a fracture of the proximal fibula with associated syndesmosis disruption and deltoid ligament tear or medial malleolus fracture. The mechanism is an eversion stress in which the force vector travels upward, damaging the syndesmosis complex and fracturing the proximal fibula. Al- though less common than other ankle fractures, this is an unstable fracture that is commonly misdiagnosed or missed altogether.13 Special consideration should be made for additional radiographic images and emergent orthopedic referral. (See Figure 3 and Figure 3B.)
Radiographic Findings
Routine radiographic imaging of the ankle includes AP, lateral, and oblique (mortise) views.
The Ottawa ankle rules were developed to aid in deciding when to use radiography for patients with ankle injuries. In an era of practicing “defensive medicine,” the rules have been shown to have sensitivities between 97% and 100%, with variable specificity, which has led to a decrease in use of ankle radiography, waiting times, and costs without patient dissatisfaction or missed fractures.11,12
Ankle radiograph series is required only if there is any pain in the malleolar zone and:
- bone tenderness at the posterior edge of the distal 6 cm or tip of the fibula
- bone tenderness at the posterior edge of the distal 6 cm or tip of the tibia
- inability to take four steps either immediately or during evaluation.
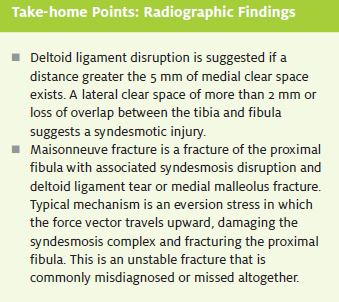
Isolated lateral and medial malleolar fractures are best seen on AP view. Posteriormalleolar fractures are best seen on the lateral view. On the mortise view, the distances between the talus and the lateral malleolus, the talus and the medial malleolus, and the talus and the tibial plafond is known as the clear space, and should normally be equidistant throughout.
Deltoid ligament disruption is suggested if a distance greater than 5 mm of medial clear space exists. A lateral clear space of more than 2 mm or loss of overlap between the tibia and fibula suggests a syndesmotic injury. (See Figure 2A and Figure 2B.) The Maisonneuve fracture is a fracture of the proximal fibula with associated syndesmosis disruption and deltoid ligament tear ormedialmalleolus fracture.
The mechanism is an eversion stress in which the force vector travels upward, damaging the syndesmosis complex and fracturing the proximal fibula. Although less common than other ankle fractures, this is an unstable fracture that is commonly misdiagnosed or missed altogether.13 Special consideration should be made for additional radiographic images and emergent orthopedic referral. (See Figure 3A and Figure 3B.)
Fracture Classification
Ankle fractures can be classified as single malleolar, bimalleolar, and trimalleolar if the posterior part of the tibial plafond is involved.
Careful attention must be paid to all single malleolar fractures because ligament in- stability is frequently associated with the contralateral side. Distal fibula fractures are the most common fracture type to the ankle. The Danis-Weber classification for ankle fractures is simple and is the most useful for primary care management (Table 1).14
An ankle fracture is considered unstable if two or more sites of significant injury are present, such as a malleolar fracture and a ligamentous disruption or a bimalleolar fracture.10
Treatment
The immediate goals of treating acute ankle injuries are to decrease pain and swelling and to protect sur- rounding ligaments from further damage. For acute ankle sprains, the RICE (rest, ice, compression, elevation) treatment protocol is commonly used. This includes protection using a compressive device such as a lace up or semirigid support. This has been shown to significantly decrease short-term swelling.15
Avulsion fractures and stable, nondisplaced distal fibula fractures can be treated with a hard-sole shoe, walking cast, or compression wrap.13 Fracture dislocations must be reduced immediately to prevent complications, such as neurovascular compromise and avacular necrosis. The ankle should be splinted in neutral position, usually with a short-leg posterior splint. A sugar-tong splint adds additional mediolateral support. All patients with unstable ankle fractures should be made non-weight bearing, fitted with crutches, and instructed to maintain RICE protocol.
Subtle fractures of the ankle or foot can often present as acute ankle sprains. Always remember to palpate the proximal fibula, base of the fifth metatarsal, anterior process of the calcaneus, and the lateral talar process. Repeat x-rays in 10 to 14 days may show callous formation. CT or MRI may be indicated for further evaluation if an ankle sprain is not progressing as expected.
References
- Daly PJ, Fitzgerald RH Jr, Melton LJ, et Epidemiology of ankle fractures in Rochester, Minnesota. Acta Orthop Scand. 1987;58:539-544.
- Ivins Acute Ankle Sprain: An Update. Am Fam Physician. 2006;74:1714-1720.
- Mandi DM, Nickles WA, Mandracchia VJ, et Ankle Fractures. Clin Podiatr Med Surg. 2006;23:375-422.
- Valtola A, Honkanen R, Kroger H, et Lifestyle and other factors predict ankle fractures in perimenopausal women: A population-based prospective co- hort study. Bone. 2002; 30:238-242.
- Ganesh SP, Pietrobon R, Cecilio The impact of diabetes on patient out- comes after ankle fracture. J Bone Joint Surg. 2005;87:1712-1718.
- Wexler The injured ankle. Am Fam Physician. 1998;57:474-480.
- Frey C, Foot and ankle. In: Essentials of Musculoskeletal Care. Rosemont, Ill.: American Academy of Orthopaedic Surgeons, 2005:593.
- Simon RR, Koenigsknecht Fractures of the Ankle. In: Emergency Orthope- dics: The Extremities. McGraw Hill, New York 2001:497.
- Pimentel Orthopedic trauma: Office management of major joint injury. Med Clin N Am. 2006;90:355-382.
- Koehler SM, Eiff Overview of ankle fractures. Available at: www.uptodate.com/patients/content/topic.do?topicKey=ad_orth/22905&title=Exerci se. Accessed June 19, 2008.
- Stiell I, Wells G, Laupacis A, et Multicentre trial to introduce the Ottawa ankle rules for use of radiography in acute ankle injuries. Multicentre Ankle Rule Study Group. BMJ. 1995;311:594-597.
- Markert RJ, Walley ME, Guttman TG, et A pooled analysis of the Ottawa ankle rules used on adults in the ED. Am J Emerg Med. 1998;16(6):564-567.
- Rooks YL, Corwell Common urgent musculoskeletal injuries in primary care. Prim Care Clin Office Pract. 2006; 33:767-769.
- Steele PM, Kelly JD. Ankle Available at: www.emedicine.com/ sports/TOPIC4.htm. 2006. Accessed June 19, 2008.
- Kerkhoff GM, Strujis PA, et Different functional treatment strategies for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002; (3):CD002938.