Published on
Our goal with the Bouncebacks series is to maximize patient safety and minimize the urgent care provider’s medico-legal exposure. As Greg Henry wrote in the forward of our Bouncebacks! book, “The
smart doctor is not the one who learns from his own mistakes. The smart doctor is the one who learns from the mistakes of others.”
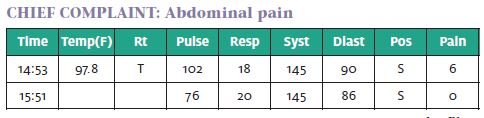
Our case this month involves a young man with vomiting and diarrhea and abdominal pain. This typical urgent care complaint usually is from a self-limiting illness, but if the history and physical exam are not able to rule out the “think worst first” diagnosis, then the patient may need to be referred to an emergency department, sent for further testing, or to return to the urgent care for a recheck.
In this case, our patient’s complaints at the first visit seem benign, except for several “red flags.” While it is unclear if the ultimate outcome would have been altered if the diagnosis was made sooner, an accurate diagnosis and recognition of serious illness must be the goal of every encounter.
A 24-Year-Old Man with Abdominal Pain
Initial Visit
(Note: The following is the actual documentation of the providers, including punctuation and spelling errors.)
HISTORY OF PRESENT ILLNESS:
24 y/o male c/o abdominal pain and n/v/d x 1 day. States he had a temperature yesterday and began to have stomach upset. States he began throwing up this am x 5 and admits to diarrhea today.
States pain is in the top part of his abdomen. Denies bloody urine or stool. States he has not been able to keep any liquids down today. Denies radiation of pain. Rates pain 6/10. Denies fever, chest pain, SOB, cough, rhinorrhea, dysuria or hematuria.
PAST MEDICAL HISTORY/TRIAGE:
Chief complaint/quote: (Per triage nurse): Pt. states he have severe lower abd. pressure pain vomiting also lower back pain. Complains of nausea, vomiting, diarrhea and flank pain. Pt c/o difficulty urinating. No private physician.
Allergies: No known allergies.
Medications: The patient is not taking medica- tions at this time.
Past medical history: No significant medical history. No significant surgical history.
EXAM:
General: Alert and oriented X3, obese, well appear- ing, in no apparent distress
Head: Normocephalic; atraumatic.
Eyes: PERRL
Nose: The nose is normal in appearance without rhinorrhea
Resp: Normal chest excursion with respiration; breath sounds clear and equal bilaterally; no wheezes, rhonchi, or rales
Card: Regular rhythm, without murmurs
Abd: Non-distended; tender over RUQ, Epigastrium and LUQ, soft, without rigidity, rebound or guarding
Skin: Normal for age and race; warm and dry; no apparent lesions
ORDERS:
Demerol 25mg IVP, Pheneran 12.5mg IVP, Levaquin 500mg PO, .9NS 1 L bolus
PROGRESS NOTES:
When the patient was ready to leave, he mentioned that the last time he had a stool, he saw some blood in it. I prescribed levaquin 500mg QD for 3 days in case this was bacterial in origin as there is good data to support a decrease in duration of symptoms with quinolone therapy. Patient is feeling better.
DIAGNOSIS:
- Gastroenteritis, 2. Vomiting – and nausea
DISPOSITION:
The patient was discharged to Home ambulatory at 17:03. Given name and number of PCP for follow up if not improved in 3-4 days. Prescriptions for Phenergan 25mg PO and suppositories. After care instructions for nausea, vomiting and diarrhea.
Discussion of Documentation and Risk Management
Issues at Initial Visit Error 1
Error: Nursing notes mention “trouble urinating,” but this was not addressed by the provider.
Discussion: Anything mentioned in the medical record is fair game; if the triage notation mentions a symptom, it needs to be evaluated. Trouble urinating could be from dehydration, renal failure, ureterolithi- asis, or urinary retention from over-the-counter med- ications or obstruction such as prostatitis.
It seems like the physician thought this was a volume problem and gave a liter of IV fluids in the department, but it is not documented whether this resulted in ability to urinate. Additionally, the exam does not include a genitourinary evaluation.
Teaching point: Once a piece of data is included in the medical record, it needs to be addressed with either diagnostics or an explanation of the provider’s thought process on its relevance—or irrelevance to the case.
Error 2
Error: Severe abdominal pain should be taken seri- ously.
Discussion: The patient apparently felt better with IV fluids, promethazine HCl (Phenergan), and meperidine hydrochloride (Demerol), which would be expected narcotics are good for pain! But the need for IV narcotics is a sign that the pain is bad enough that there might be something more serious occurring.
Teaching point: Patients with pain severe enough to require IV narcotics generally require further evaluation.
Error 3
Error: Progression of symptoms was not adequately addressed.
Discussion: During the course of his evaluation, the patient developed a potentially ominous symptom (blood in the stool). Whereas the differential for hematochezia is often from a benign cause such as anal irritation from frequent wiping or painless internal hemorrhoids, more serious causes need to be considered.
Though typically the urgent care visit is short and does not include an option for prolonged observation, sometimes symptoms can change or progress during the evaluation.
It seems the physician took the easiest course and prescribed a course of antibiotics and sent the patient home. A more prudent approach may have been to revisit the evaluation with a more in-depth history and repeat abdominal exam. A complaint of undifferentiated abdominal pain and bloody stool may warrant more than two hours of observation, IV fluids, and narcotic pain medicine.
Teaching point: The combination of abdominal pain, bloody stool, and trouble urinating may suggest serious pathology and likely warrants a more emergent work-up.
Error 4
Error: Inappropriate follow-up parameters.
Discussion: The patient had undifferentiated abdominal pain and bloody stool, a potentially ominous combination. He also had no primary care physician. He was told to follow up with a PCP “if not improved in 3-4 days,” a time period too long to detect progression of serious illness. Close follow-up within 12 hours, arranged with a primary care physician prior to discharge (or back at your own center), may have been more appropriate.
Teaching point: While immediate diagnostic work-up is often not necessary, when a potentially life-threatening diagnosis has not been ruled out, urgent, timely outpatient follow-up must be arranged and its importance stressed to the patient.
Bounceback Visit—ED
Return EightHours Later 12:42 a.m.
Presents per EMS with chief complaint of vomiting. Nurse documents severe, stabbing pain 10/10 which worsened 3 hours ago. Initial vital signs:
Temp (F) Pulse Resp BP
95.2 80 28 100/60
ED physician sees pt. immediately on arrival and documents complaints of vomiting and midepigastric abdominal pain. Exam shows pt. to be uncomfortable with tenderness mid-epigastrium but soft without r/r/g. Orders for dilaudid 1mg, phenergan 12.5mg and IV fluids
01:00 IV fluids started and medications administered
01:05 (RN notes) Patients brother comes out to ask nurse what med the pt. was given, stating, “I don’t think he’s breathing”. Pt was cyanotic in face, took an agonal breath, no pulse palpated carotid. Code blue called and patient moved to trauma room for resuscitation.
01:09 The patient was immediately intubated and chest compressions were begun while being attached to the monitor. Patient was found to be initially in v- fib and was shocked at 200J. Patient then went into PEA. A Right femoral triple lumen CVP was placed by a second ED physician who had come in to assist. The patient continued to alternate betweenv-fib and PEA. The patient was given narcan, glucose, bicarb x2, calcium chloride, magnesium, and several rounds of ep- inephrine and atropine. Chest compressions and bagged respirations were continued throughout the code. The patient’s wife was initially in the room when the patient became apneic and pulseless and was escorted immediately into a family consultation room by staff. The patient was coded for an hour without return of a pulse despite multiple medications and shocks.
02:09 The code was ended with agreement by staff.
Labs return with serum bicarb of 5 and creatinine of 2.5. Autopsy shows:
Infarction of small bowel Mesentaric vein thrombosis
Multiple other sites of thrombi, including several small PEs
Discussion of Mesenteric Ischemia
Our patient initially presented with abdominal pain, vomiting, and diarrhea and was diagnosed with gas- troenteritis. He returned less than eight hours later in multi-organ system failure and expired shortly after from infarcted bowel and multiple small PEs.
The classic presentation of mesenteric ischemia is abdominal pain “out of proportion” to exam findings. The symptoms may also be vague, especially in otherwise healthy individuals with no apparent risk factors for the disease. This often leads to missed or delayed diagnosis and increased mortality.
Mesenteric ischemia is caused by decreased blood flow to the GI tract, typically as a result of either thrombosis within the mesenteric arteries or as a result of embolism from a more proximal source. It has been reported as the cause of 0.1% of all hospital admissions, with mortality rates ranging from 60% to 100%.
Common presenting symptoms include abdominal pain, vomiting, and diarrhea. Melena or hematochezia is reported in 15% of cases, with occult blood detected in nearly half of all cases. Physical examination often is initially unremarkable until the ischemia has continued, causing distention, ileus, peritonitis and shock. As mentioned, rectal exam may reveal blood, although a negative fecal occult blood test (Hemoccult) does not rule out the diagnosis.
Diagnostic Testing
As with most true surgical emergencies, labs are often nonspecific and of little help. Various reports in the literature cite that 25% or more of patients will have a normal WBC count. Traditional teaching recommends a serum lactate level; unfortunately, an elevation of the lactate is a late finding.
In the age of CT scans, plain films for the evaluation of abdominal pain have little utility. The big question is whether this patient should have had a CT scan. While his complaints and exam on presentation seemed relatively benign, we do not know if this changed during the course of his evaluation. A repeat exam may have revealed rigidity or guarding, indicating a surgical abdomen.
Additionally, the description of the rectal bleeding was minimal. A patient with significant ongoing blood loss without another explanation would best be evaluated with a CT.
There are no good evidence-based guidelines with recommendations for who should be scanned. A particularly ominous finding in mesenteric ischemia is pneumatosis intestinalis. For evaluation of mesenteric ischemia, CT has sensitivities over 90%.
Risk-Management Principles
While the initial visit appeared benign at first glance, a closer look suggests otherwise.
The patient initially complained of vomiting, diarrhea, and abdominal pain—symptoms occurring frequently in urgent care practice. However, there were some unrecognized red flags, including difficulty urinating, bloody stool, and pain severe enough to require IV narcotic medication. He bounced back eight hours later and expired shortly after from mesenteric ischemia.
Although the patient looked well initially, there was some subtle suggestion of serious underlying pathology. Unfortunately, it was too late when the diagnosis became clear.
The chance that a healthy 24-year-old man would have a severe undiscovered coagulation disorder is extremely small, and even a vigilant physician could miss this serious diagnosis. Nonetheless, one must have a high index of suspicion; though the initial complaints are often vague and nonspecific, it is during this part of the clinical course that we can make the greatest impact.
Suggested Readings
- Nagurney JT, Brown DF, Chang Y, et al. Use of dia nostic testing in the emergency department for patients with non-traumatic abdominal J Emerg Med. 2003; 25:363-371.
- Ahn SH, Mayo-Smith WW, Murphy BL, et Acute nontraumatic abdominal pain in adult patients: abdominal radiography versus CT evaluation. Radi- ology. 2002; 225:159-164.
- Rosen MP, Siewert B, Sands DZ, et al. Value of ab- dominal CT in the emergency department for pa- tients with abdominal pain. Eur Radiol. 2003; 13:418-424.
- Nishijima DK, Su M. Mesenteric ischemia. eMedicine from WebMD. Available at www.emedicine.com/emerg/ TOPIC311.HTM. Accessed June 16, 2008
