Urgent message: Urgent care centers play a vital role as a gateway into the health system for many children with acute care needs. Some of these needs require identification by the urgent care team, who may then need to stabilize the patient and initiate transfer to optimize clinical outcomes.
Nikhil B. Shah, MD
INTRODUCTION
Pediatric office emergencies can be challenging for urgent care staff to manage. These high-stakes events do not occur frequently enough to give staff confidence or experience with the clinical care and team dynamics required for emergency management. Moreover, the consolidation of pediatric hospital care, shifts in utilization patterns, and the increasing prevalence of medically complex pediatric patients, has led to a growing influx of critically ill children in the outpatient setting, particularly urgent care. Therefore, it is essential for all members of the care team to be prepared for an office emergency and every urgent care should train its staff accordingly.
In 2007, the American Academy of Pediatrics (AAP) Section on Emergency Medicine published guidance on essential medications and equipment that outpatient pediatric offices should carry in the event of a pediatric emergency. They advised regular, simulation-based practice to train staff in managing critically ill children and having formal emergency preparedness policies and protocols in place.1
Almost 15 years later, a multicenter study examining the impact of these recommendations found that while many of the outpatient offices in their cohort carried the AAP-recommended supplies, the majority still had not implemented policies or procedures to manage critical events.2
There may be myriad reasons for this. Among them are denial (What is the likelihood this will happen in my office?). Liability may be another concern (If I carry this medication and equipment and my staff are not trained adequately to use it, I could legally be held accountable). Perceived cost might play a role. And, finally, personnel challenges (I just don’t have the staff to do it, it’s just me and a medical assistant). These concerns, though understandable, may not be entirely valid, and should not be barriers to implementation.
One challenge for the outpatient setting is that there is no gold standard certification, course, or simulation sequence to prepare staff for medical emergencies. Many practices have embraced the American Heart Association’s Basic Life Support (BLS), Pediatric Advanced Life Support (PALS), or Pediatric Emergency Assessment Recognition and Stabilization (PEARS) courses to teach emergency preparedness and simulation training.
BLS includes training in CPR, bag-valve-mask ventilation, and AED use, but has a limited scope for urgent care and a pre-hospital focus not specific to the problems of children.
PALS, on the other hand, is pediatric-specific and more comprehensive; however, this course features many advanced resuscitation algorithms that are not within the scope of a typical urgent care.
PEARS, which is also pediatric-specific, teaches the fundamentals of assessment and stabilization and is geared towards a broad target audience. However, it may not be comprehensive enough for urgent care clinicians as it does not cover advanced skills and interventions required to stabilize higher-acuity pediatric patients that may be encountered in the urgent care setting.
While PALS may be the most comprehensive course for pediatric emergency management, it has become increasingly apparent that PALS algorithms, equipment, medications, and personnel requirements do not adequately translate to urgent care. For example, most nonhospital-based urgent care practices will not have a manual defibrillator/monitor, wall oxygen, and suction; nor do they carry many of the medications and other equipment that are found in the hospital setting. Endotracheal tubes and other advanced airway devices may also be noticeably absent in an urgent care due to medicolegal concerns arising from staffing with newer, inexperienced providers who may lack training in their use.
Along these lines, as fewer emergency medicine-trained physicians are being relied upon to staff urgent care offices, the management priority is shifting towards stabilization for transfer rather than providing definitive care. The conundrum may lie in training staff to recognize and manage these “sick” but not critically ill patients who, for example, may simply be in respiratory distress but not failure.
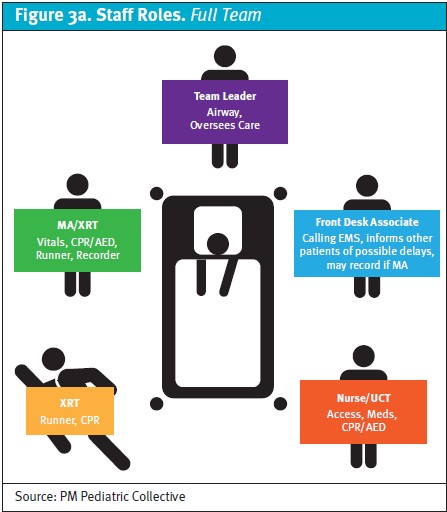
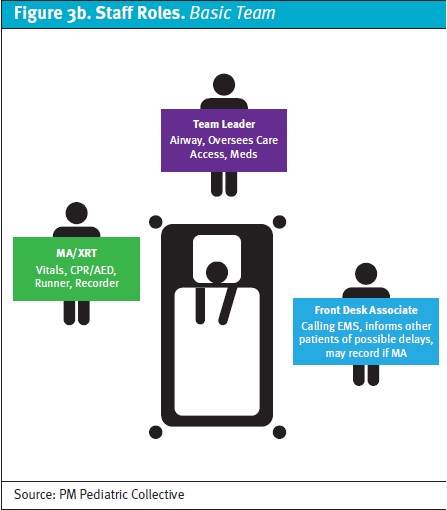
Finally, the staffing make-up of an urgent care office may place a physician or an advanced-practice provider (APP) alongside a medical assistant/receptionist, x-ray tech, or perhaps a nurse, as the care team that must manage a pediatric emergency. This is in stark contrast to the hospital setting in which resources are seemingly inexhaustible and where a critically ill child is more likely to be managed by a multitude of physicians, APPs, and nurses.
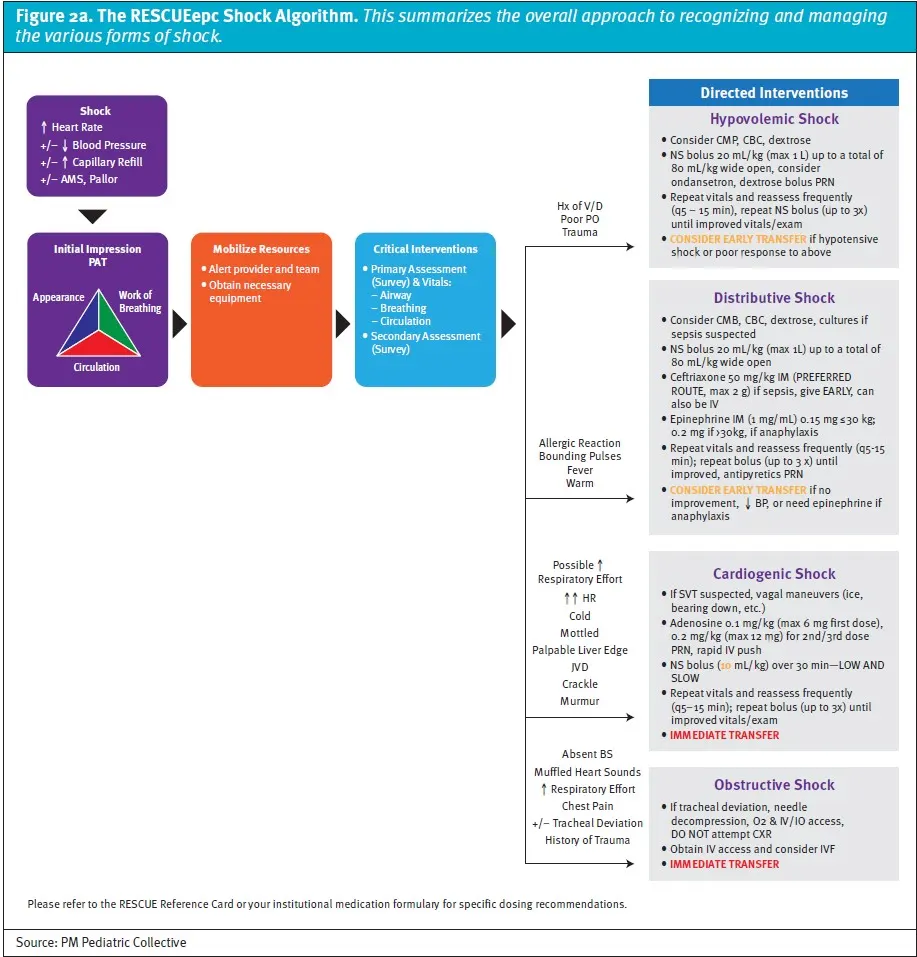
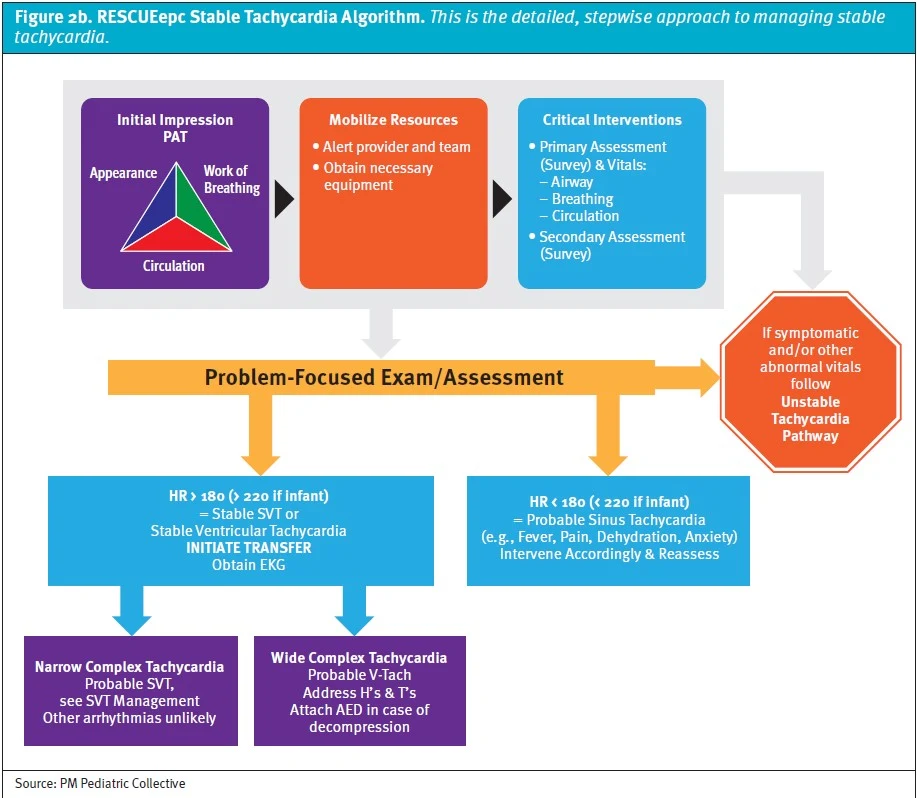
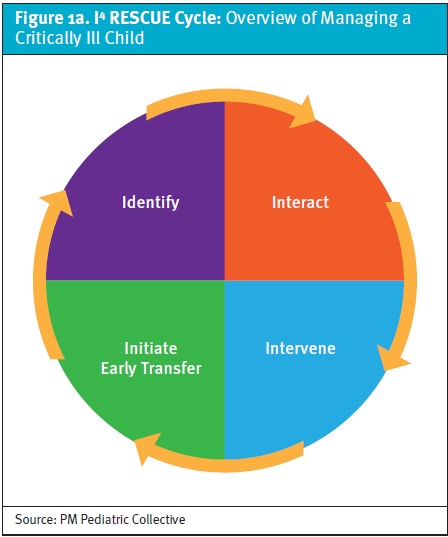
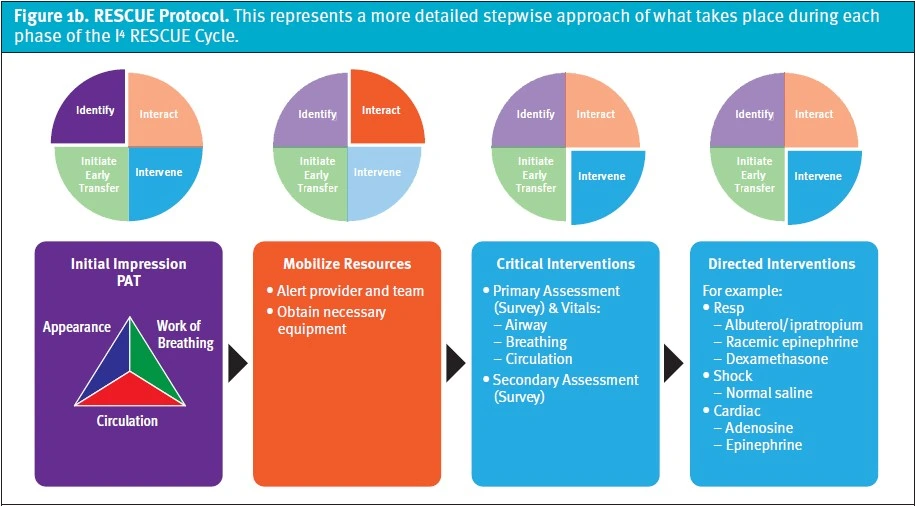
This void necessitates the creation of RESCUEepc (Resuscitation & Stabilization of Children in the Urgent Care Environment – emergency preparedness course)—a novel training curriculum for managing critically ill children that focuses on the unique personnel makeup, medications, and equipment found in a resource-limited ambulatory setting. RESCUEepc is a blended-learning activity in which participants must complete pre-coursework in the form of online learning modules (3 hours duration) prior to attending an instructor-led classroom training session (4 hours duration). The foundation for the course is a novel, team-based management approach collectively referred to as the “RESCUE Protocol” (Figures 1a and 1b), which utilizes original, evidence-based, urgent care-specific algorithms (Figures 2a and 2b).
The in-person training comprises a brief review of key points from the online pre-coursework, practice-till-perfect approach to learning urgent care-specific skills (eg, operating an oxygen tank/attaching a regulator, using a portable suction device, AED, etc.), and simulation-based practice scenarios, with an emphasis on managing critically ill children with both full- and minimal staffing complements (Figures 3a and 3b). The course concludes with an online postassessment and megacode scenario.
Successful completion of the course requires a minimum score of 80% on the online exam and meeting all required competencies delineated in the structured debrief tool for the megacode scenario. The target audience is similar to that of PALS and includes physicians, APPs, and nurses. On the horizon is a high-yield version of the course with just the essentials (diminutively referred to as RESCUEepc-“lite”), intended for clinical support staff such as x-ray techs and medical assistants.
Thus far, RESCUEepc has been deployed in multiple regions, comprising over 90 provider and nurse participants. Key competencies highlighted in the course are tied to various quality metrics that will be tracked over time. Ultimately, the success of RESCUEepc will depend on whether it has an impact on patient outcomes, which will also be measured. The next steps for RESCUEepc are to complete internal implementation of the course by the end of this year and then launch RESCUEepc-lite for clinical support staff in 2024. One advantage of RESCUEepc is that it is scalable to other outpatient settings and can be tailored to their scope of practice. As such, this customizable version of the course will be known by the apropos acronym, SCOPE (Stabilization of Children with Office Pediatric Emergencies), which is currently under development. The goal is to obtain certification for RESCUEepc and its offshoots by offering them in partnership with an accrediting body and making them available externally to both urgent care centers and other outpatient practices that take care of children.
Urgent care has differentiated itself as a highly specialized environment that has carved its own niche within the modern healthcare landscape. As such, the field deserves to have training that is specific to its needs and not an amalgamation or adaptation of what already exists. While BLS, PALS, and PEARS are valuable tools, there is a compelling need for a resuscitation course specifically designed for urgent care that addresses the unique considerations of this setting and provides the necessary training to effectively manage a sick child.
REFERENCES
- Frush K. American Academy of Pediatrics Committee on Pediatric Emergency Medicine. Preparation for emergencies in the offices of pediatricians and pediatric primary care providers. Pediatrics. 2007;120(1):200–212.
- Abulebda K, Yuknis ML, Whitfill T, et al. Improving Pediatric Acute Care Through Simulation (ImPACTS). Preparedness for pediatric office emergencies: a multicenter, simulation-based study. Pediatrics. 2021;148(3):e2020038463.
Author affiliations: Nikhil Shah, MD is Senior Director of Provider Training, PM Pediatric Care.
Click Here to download the article PDF
