Differential Diagnosis
- Ventricular tachycardia
- Supraventricular tachycardia with aberrancy
- Atrioventricular reentrant tachycardia
- Sodium channel toxicity
- Hyperkalemia
Diagnosis
This patient was diagnosed with supraventricular tachycardia with aberrancy. The ECG reveals wide complex tachycardia (WCT) with ventricular rate 150 beats/minute. The QRS duration is prolonged, measuring >120 ms. The QRS complex has a right bundle branch block (RBBB) pattern with an “M”-shaped QRS complex in the anterior precordial leads (V1-V3) and a slow, slurred S-wave in the lateral leads (I, aVL, V6). Additionally, there is an extreme left axis deviation (>45⁰ of leftward deviation), suggesting left anterior fascicular block (ie, bifascicular block).
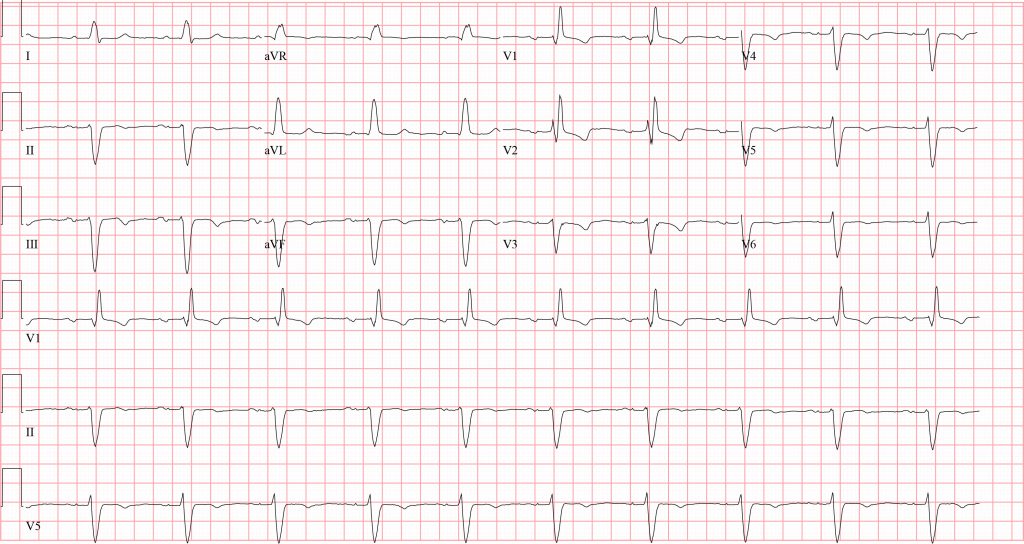
This rhythm is either arising from a supraventricular focus (ie, atrioventricular node or higher) with aberrancy (ie, bundle branch block) or is ventricular in origin (ie, ventricular tachycardia).
Ventricular tachycardia (VT) is the most life-threatening WCT and should be the presumed diagnosis unless there is a very compelling reason to suggest otherwise. Up to 80% of all WCT is VT,1 and the diagnosis is even more likely in an elderly patient with known coronary artery disease (as with this case).
There are established algorithms to help differentiate supraventricular tachycardia (SVT) with aberrancy versus VT. SVT includes atrial flutter (2:1 conduction is a strong consideration in a patient with a heart rate of 150 beats/min like this one), atrial tachycardia, and atrioventricular nodal reentrant tachycardia.
When a patient has underlying conduction disease (ie, bundle branch block) at baseline, supraventricular tachycardia will have the appearance of WCT. The most cited algorithm to help differentiate SVT with aberrancy from VT is the Brugada algorithm.2 It involves a series of four criteria; VT is diagnosed when any single criterion is met. The criteria include:
- Absence of an rS complex across the precordium
- Beginning of the R to the nadir of the S wave greater than 100 msec
- Signs of atrioventricular dissociation (ie, fusion complexes or capture beats)
- Absence of typical bundle branch morphology
It should be noted than none of the established criteria perform well in the acute setting.1,3,4 Therefore, it is safest to treat WCT as VT because the consequences of treating WCT as SVT could be devastating if the diagnosis is incorrect. Atrioventricular nodal blocking agents like beta blockers or non-dihydropyridine calcium channel blockers could result in cardiac decompensation in patients with ventricular tachycardia.
Cardioversion is the preferred management. Synchronized electrical cardioversion is safest, although pharmacologic cardioversion can be attempted. Procainamide 10 mg/kg over 20 minute is likely to be the most effective for VT,5 but other pharmacologic options exist. Adenosine is a short-acting atrioventricular nodal-blocking agent that can be attempted and may be both diagnostic and therapeutic. If the patient converts with adenosine (6 mg intravenously followed by 12 mg if ineffective), the diagnosis is likely to be SVT with aberrancy, although adenosine-sensitive VT does exist.6
While this patient was ultimately diagnosed with SVT with aberrancy, the presumed diagnosis should be VT in the acute setting for the aforementioned reasons. This patient spontaneously converted out of the rhythm and into sinus rhythm with underlying bifascicular block (Figure 2). When the QRS morphology in the WCT exactly matches that of their baseline ECG (assuming one is available), SVT with aberrancy can be more reliably diagnosed (as with this case).
Sodium channel toxicity can cause WCT, although there was no history of ingestion with this case. Sodium channel-blocking toxicity was initially described in tricyclic overdoses,7 but other sodium channel-blocking agents include antiarrhythmics (lidocaine, phenytoin, propafenone, flecainide, amiodarone, sotalol), antiepileptic medications (carbamazepine, lamotrigine), selective serotonin reuptake inhibitors (citalopram, fluoxetine), antihistamines (diphenhydramine), propranolol, cyclobenzaprine, and others.8 Hyperkalemia can also cause WCT, but this was not the case here. Atrioventricular reentrant tachycardia, when conducted in an antidromic fashion, is a cause of WCT. It is a phenomenon that can happen in patients with ventricular pre-excitation (ie, the Wolf-Parkinson-White syndrome)9 and was not the case here.
Learnings/What to Look for
- WCT is VT up to 80% of the time
- Algorithms for differentiating VT from SVT with aberrancy exist, but none are reliable in the acute setting
- Consider all WCT to be VT unless a compelling alternative exists
Pearls for Urgent Care Management and Considerations for Transfer
- The safest approach to management of WCT is electrical synchronized cardioversion
- If the patient is unstable, cardioversion should be perused immediately
- If stable, patients with WCT should be immediately transferred to the nearest emergency department with defibrillation pads in place
References
- Vereckei A. Current algorithms for the diagnosis of wide QRS complex tachycardias. Curr Cardiol Rev. 2014;10(3):262-276.
- Brugada P, Brugada J, Mont L, et al. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation. 1991;83(5):1649-1659.
- Szelényi Z, Duray G, Katona G, et al. Comparison of the “real-life” diagnostic value of two recently published electrocardiogram methods for the differential diagnosis of wide QRS complex tachycardias. Acad Emerg Med. 2013;20(11):1121-1130.
- Baxi RP, Hart KW, Vereckei A, et al. Vereckei criteria as a diagnostic tool amongst emergency medicine residents to distinguish between ventricular tachycardia and supra-ventricular tachycardia with aberrancy. J Cardiol. 2012;59(3):307-312.
- Ortiz M, Martin A, Arribas F, et al. Randomized comparison of intravenous procainamide vs. intravenous amiodarone for the acute treatment of tolerated wide QRS tachycardia: The PROCAMIO study. Eur Heart J. 2017;38(17):1329-1335.
- Michowitz Y, Belhassen B. New Insights on Verapamil-Sensitive Idiopathic Left Fascicular Tachycardia. J Electrocardiol. 2018;51(5):874-878.
- Boehnert MT, Lovejoy FH. Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after an acute overdose of tricyclic antidepressants. N Engl J Med. 1985;313(8):474-479.
- Gray A, Talari G, Mirrakhimov AE, Barbaryan A, Ayach T, Chadha R. The Role of Sodium Bicarbonate in the Management of Some Toxic Ingestions. Int J Nephrol. 2017;2017:1-8.
- Moore EN, Spear JF, Boineau JP. Recent electrophysiologic studies on the Wolff-Parkinson-White syndrome. N Engl J Med. 1973;289(18):956-963.
View Similar Clinical Challenges
- A 55-Year-Old Man with a 2-Day History of Respiratory Symptoms, Palpitations, and Dizziness
- A 73-Year-Old Woman with a 12-Day History of Palpitations
- An 82-Year-Old Man with Palpitations
