Differential Diagnosis
- First-degree heart block
- Second-degree type 1 heart block
- Second-degree type 2 heart block
- Third-degree (complete) heart block
- Hyperkalemia
- Sinus bradycardia
Diagnosis
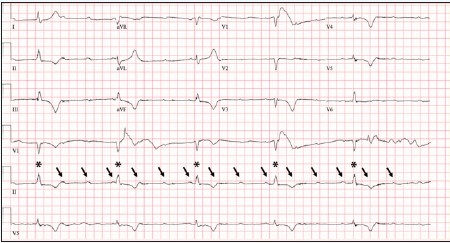
The patient was diagnosed with a third-degree (complete) heart block. The ECG reveals a complete heart block with atrioventricular dissociation. There is an atrial rate of approximately 100 beats per minute and a ventricular rate of 30 beats per minute. There are no ST-elevations or depressions. T-wave inversions are noted in the precordium as well as in the inferior leads.
Complete heart block (CHB) is characterized by atrioventricular dissociation as atrial impulses fail to conduct to the ventricles. Due to this failure, the atria and ventricles act independently of each other. Systemic perfusion is maintained by an escape rhythm originating from either the junction or the ventricles.
Causes of CHB include myocardial infarction, AV nodal blocking drugs, or idiopathic degeneration of the conduction system. CHB caused by inferior myocardial infarctions tends to lead to junctional escape rhythms, while CHB caused by anterior myocardial infarctions causes slower ventricular escape rhythms.
If the block is the result of a diseased AV node, a junctional focus (escape rhythm) emerges and produces a rate typically between 40 to 60 beats per minute. This is characterized by a narrow QRS complex on ECG. However, when infra-Hisian (below the bundle of His) conduction disease exists as the cause, the escape focus is ventricular in origin, producing a slower, less reliable rhythm—characterized by a wide QRS complex on ECG. If no escape rhythm is present, the patient will not be able to perfuse, and will subsequently arrest due to cardiac standstill.
CHB is life-threatening, and it is typical for patients with this condition to experience severe bradycardia and hypotension. A pacemaker is the necessary treatment for CHB.
Additional examples may be found in the ECG Stampede glossary (www.ecgstampede.com/glossary).
Learnings/What to Look for
- CHB is a life-threatening event and prompt recognition, investigation into the underlying cause, and treatment is imperative
- A careful medication review should be completed for AV nodal blocking agents
- Consider thyroid studies if no other clear cause is identified
- Insults to the conduction system at the AV node are more likely to respond to atropine than infra-Hisian etiologies
- Hyperkalemia could be a mimic for CHB, and should be considered in patients with bradycardia, particularly if there is a wide-QRS complex
Pearls for Urgent Care Management and Considerations for Transfer
- Transcutaneous pacing pads should be placed, with emergent transfer to a higher level of care facility
- If unstable, transcutaneous pacing should be initiated

Click Here to download the article PDF
