Published on
Differential Diagnosis:
- Myocardial ischemia
- Myocardial infarction
- Nonspecific intraventricular conduction delay
- Atrial tachycardia
- Hyperkalemia
Diagnosis
The correct diagnosis is atrial tachycardia with abnormal P wave axis. The ECG illustrates an atrial tachycardia with a rate around 115 beats per minute, with three PVCs.
Learnings/What to Look for
Atrial tachycardia is an arrhythmia that occurs when the electrical signal in the heart originates from an atrial site other than the sinoatrial node. An ectopic atrial focus can be recognized by identifying the P wave axis.
The P wave represents atrial depolarization. Sinus rhythm is present when the sinoatrial node generates a signal that depolarizes the atria.
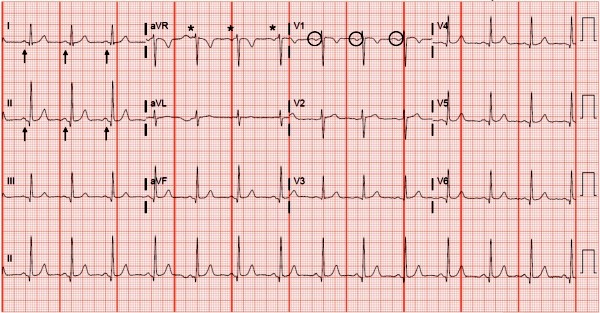
The sinoatrial node is a complex cluster of cells that exists at the junction of the superior vena cava and the right atrium and is the dominant pacemaker under normal circumstances. When the sinoatrial node generates the depolarizing impulse, the P wave will have an axis between 0° and +75°—upright in leads I and II, inverted in aVR, and frequently biphasic in V1. Depolarization of the right followed by left atria fuse together to form the typical monophasic P wave seen in leads I and II (Figure 2).
Derangements of the P wave axis are caused by an impulse originating from an ectopic atrial focus instead of the sinoatrial node. In our case, the P wave is inverted in the inferior leads and upright in aVR, indicating impulse generation from a low atrial site (Figure 3).
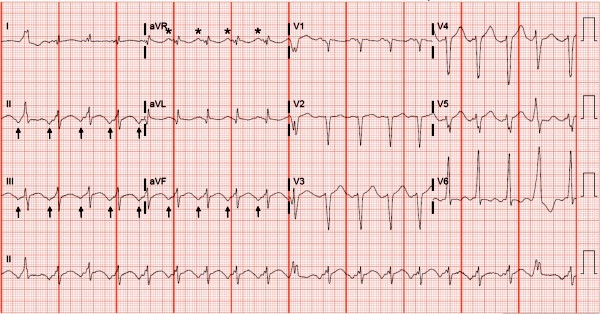
The inverted P waves on our patient’s ECG merge with the T waves to give the appearance of ischemic T wave inversions; however, a holistic approach to the ECG will help to reveal the presence of P waves consistent with atrial tachycardia. This rhythm is not inherently dangerous, as it is very similar to a sinus tachycardia. It is important to note, however, that as with most cases of tachycardia, atrial tachycardia may serve as a compensatory mechanism in patients with hypo/hypervolemia, sepsis, or many other conditions. Atrial tachycardia usually results from enhanced automaticity, the accelerated generation of an action potential by drugs, various forms of cardiac disease, electrolyte disturbances, or alterations of autonomic nervous system tone.1–3
Pearls for Urgent Care Management
- An abnormal P wave axis is the key to recognizing that a rhythm is not originating from the sinus node, but from an ectopic atrial focus
- Stable atrial tachycardia is not usually dangerous, but transfer may be considered in symptomatic patients or when the tachycardia is excessive
- Consider compensatory etiologies and treat the underlying condition if it exists; otherwise, outpatient referral to cardiology is sufficient
REFERENCES
- Mattu A, Tabas J, Brady W. Electrocardiography in Emergency, Acute, and Critical Care. 2nd ed. Dallas, TX: The American College of Emergency Physicians; 2019.
- Butta C, Tuttolomondo A, Giarrusso L, Pinto A. Electrocardiographic diagnosis of atrial tachycardia: classification, P-wave morphology, and differential diagnosis with other supraventricular tachycardias. Ann Noninvasive Electrocardiol. 2015;20(4):314-327.
- Poutiainen AM, Koistinen MJ, Airaksinen KE, et al. Prevalence and natural course of ectopic atrial tachycardia. Eur Heart J. 1999;20(9):694-700.
