Published on
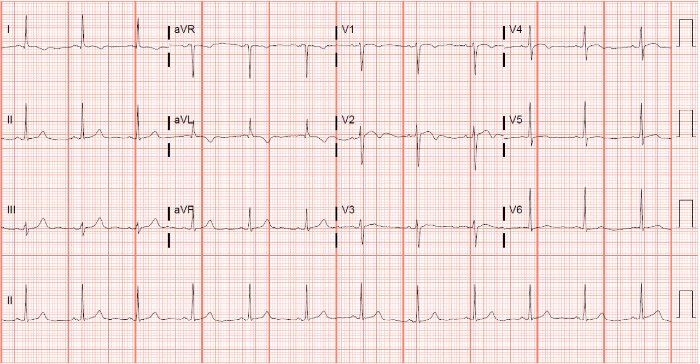
A 61-year-old female presents to urgent care with chest pain for 2 days. She describes it as “mild right now” but that it varies in intensity; it was so severe the previous night that it kept her from sleeping. Today the pain has been stuttering, lasting a couple of minutes at a time. Pain is substernal, nonradiating, and is associated with vomiting and diaphoresis. Vital signs are normal.
View the ECG and consider what your diagnosis and next steps would be. Resolution of the case is described on the next page.
(Case presented by Jon Giordano, DO, MEd, McGovern Medical School, Department of Emergency Medicine, The University of Texas Health Sciences Center at Houston.)
A 61-Year-Old Woman with a 2-Day History of Chest Pain
1 2
