Differential Diagnosis:
- Sinus bradycardia
- Second-degree atrioventricular (AV) block
- Third-degree AV block
- Hyperkalemia
- Beta-blocker toxicity
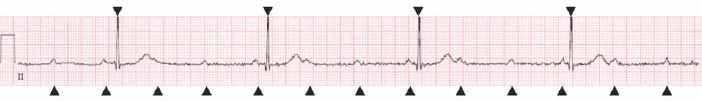
Figure 2. AV dissociation with completely independent ventricular (▼) and atrial (▲) rates.
Diagnosis
The ECG has an atrial rate of 80 bpm and a ventricular rate of 27 bpm. There are more P waves than QRS complexes, signifying the presence of an atrioventricular block. Both the P waves and the QRS complexes appear to be occurring regularly, but at different rates and with no relationship to each other.1
These findings support the ultimate diagnosis of a third-degree AV block, or complete heart block.
In complete heart block, the ECG will show complete atrioventricular dissociation. None of the atrial impulses are conducted to the ventricles, and perfusion is maintained only by a junctional or ventricular escape rhythm from an ectopic focus.
If the block is the result of a diseased atrioventricular node, a junctional focus emerges and produces a rate between 40 and 60 BPM. However, when infra-Hisian conduction disease exists (ie, below the bundle of His), the focus will be ventricular, and will be slower and less reliable.1,2
Because an escape rhythm may be transient, absent, or not generating enough cardiac output for perfusion, a third-degree AV block is life-threatening. It is typical for a patient with this condition to experience severe bradycardia and hypotension. If no escape rhythm is present the patient will arrest due to cardiac standstill.
(A note about isorhythmic complete heart block:On initial inspection of this ECG, you may suspect the patient has a second-degree AV block, Mobitz type II, as it appears there is a P wave before each QRS complex, and the other beats have been “dropped.” If this were the case, however, we’d expect the PR interval to stay consistent throughout. On closer examination of this patient’s ECG, you’ll notice that the PR interval varies, and in fact the apparent relationship between the P waves and QRS complexes is only by chance. This phenomenon is called isorhythmic complete heart block, and can be difficult to distinguish from a second-degree AV block, Mobitz type II. This patient was confirmed to have complete heart block via an electrophysiology study.)
Learnings/What to Look for
- When an ECG has more P waves than QRS complexes, consider the presence of an atrioventricular block
- A third-degree AV block will have no discernible relationship between P waves and QRS complexes
- An isorhythmic complete heart block can be difficult to differentiate from a second-degree AV block, Mobitz type II, but both represent conduction disease that needs emergent intervention
Pearls for Urgent Care Management
- Patients with third-degree AV block are at high risk of sudden cardiac death due to ventricular standstill, and should be immediately transferred for cardiac monitoring and insertion of a permanent pacemaker
- Patients with hemodynamically unstable bradycardia from an atrioventricular block should be transcutaneously paced and immediately transferred to an emergency department
References
- Knabben V, Chhabra L, Slane M. Third-Degree Atrioventricular Block. [Updated 2020 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; January 2020. Available at: https://www.ncbi.nlm.nih.gov/books/NBK545199/. Accessed January 10, 2021.
- Kusumoto FM, Schoenfeld MH, Barrett C, et al. 2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm. Circulation. 2019;140(8):e382-e482.
