Published on
Differential Diagnosis
- Tumid lupus erythematosus
- Subcutaneous panniculitis-like T-cell lymphoma
- Morphea
Diagnosis
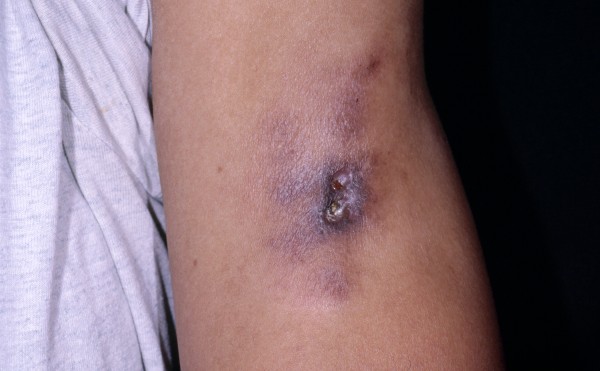
On examination, there are tender violaceous plaques and nodules with central crusted ulcers. A skin biopsy reveals a lobular panniculitis with a lymphoplasmacytic infiltrate, hyalinizing fat necrosis, and lymphoid follicles. Laboratory examination revealed a positive antinuclear antibody (ANA) and an elevated erythrocyte sedimentation rate (ESR).
Learnings/What to Look for
- Lupus panniculitis is sometimes termed lupus profundus and can be associated with overlying discoid lupus erythematosus (DLE) in approximately one-third of patients
- Lupus panniculitis is thought to be caused by an autoimmune reaction in the deep dermis and adipose tissue. The first stage is active inflammation with painful nodules, followed by the second stage of subcutaneous atrophy that can be cosmetically disfiguring
- Like SLE, lupus panniculitis occurs more commonly in women
- Lupus panniculitis develops in approximately 5% of patients with SLE but can occur as an isolated disease
- Cutaneous manifestations can develop years before or after the diagnosis of SLE
Pearls for Urgent Care Management
- In the absence of a definitive cause, treatment is aimed at reducing inflammation, such as through use of anti-inflammatory drugs
- Corticosteroids may speed recovery
- Compression stockings may help relieve symptoms in the legs
Acknowledgment: Image and case presented by VisualDx (www.VisualDx.com/jucm).
A 41-Year-Old Woman with a History of SLE and Sudden-Onset Sores on Her Limbs
1 2
