Published on
Download the article PDF: Clinical Challenges June 2025
Differential Diagnosis
- Early repolarization
- Hyperkalemia
- Acute pericarditis
- ST-elevation myocardial infarction
- Brugada syndrome
Diagnosis
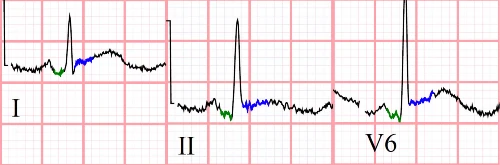
The diagnosis in this case is acute pericarditis. The ECG reveals sinus tachycardia with a rate of 108 beats per minute. There are diffuse, concave up ST-segment elevations without reciprocal changes and diffuse PR-segment depression (Figure 2).
Discussion
Acute pericarditis is an inflammatory condition of the pericardium, often causing symptoms like pleuritic chest pain that improve when leaning forward. Common causes include medications (eg, hydralazine, penicillin), infections (bacterial, viral, or fungal), malignancies, rheumatologic conditions (eg, lupus, rheumatoid arthritis), post-myocardial infarction syndromes (eg, Dressler syndrome), uremia, and idiopathic origins.1 Diagnosis requires meeting 2 out of 4 criteria:2,3
- Typical symptoms (pleuritic, sharp chest pain relieved when leaning forward)
- New pericardial effusion
- Presence of a friction rub
- Typical ECG findings
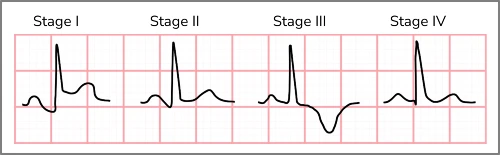
Differentiating pericarditis from ST-elevation myocardial infarction (STEMI) can be challenging, but careful attention to several electrocardiographic features can help. Features suggesting pericarditis over STEMI include diffuse concave up ST elevations without reciprocal changes, PR depression, PR elevation in aVR, ST-elevation in lead II greater than lead III, and Spodick’s sign (down-sloping of the TP segment).4 The test characteristics of any single electrocardiographic feature are insufficient to rule in/out pericarditis; the feature with the highest odds ratio for predicting STEMI (over pericarditis) is reciprocal ST-depressions. Acute pericarditis tends to follow a natural progression of electrocardiographic findings, starting with the aforementioned features in the first two weeks, followed by resolution of ST elevation, T wave flattening, T wave inversion, and finally returning to baseline over several weeks (Figure 3).5
Treatment includes non-steroidal anti-inflammatory medications tapered over 3-4 weeks and colchicine for 3 months. It’s also reasonable to prescribe a proton pump inhibitor to counteract gastrointestinal side effects. Corticosteroids are reserved for patients with contraindications to initial therapy but are not preferred due to increased recurrence.2
Although early repolarization can produce similar ECG patterns, the patient’s presenting symptoms favor acute pericarditis. Hyperkalemia can cause various ECG changes, but it does not typically result in the diffuse, concave-up ST elevation observed here. Furthermore, Brugada syndrome, characterized by ST elevation in leads V1 and V2 due to a sodium channelopathy, is inconsistent with the presented ECG.
What To Look For
- Electrocardiographic features that suggest acute pericarditis include diffuse concave up ST elevations without reciprocal changes, PR depression, ST-elevation in lead II greater than lead III, and Spodick’s sign (down-sloping of the TP segment).
- The presence of reciprocal ST-changes is very specific for an occlusive process.
Pearls For Management, Considerations For Transfer
- Patients with a clear diagnosis of acute pericarditis with a benign etiology and reliable follow up can be initiated on non-steroidal anti-inflammatory medications +/- colchicine.
- Pericardial effusion must be considered in all cases of pericarditis; however, clinically meaningful effusions occur in less than 3% of cases of acute pericarditis. It is worth noting that pericardial tamponade is more common in patients with identifiable causes compared to idiopathic cases.3 Tamponade and myocarditis should be considered in patients with tachycardia and/or hypotension; ED referral is indicated in such cases.
- If the diagnosis is in question, the etiology is unclear, vital signs are unstable, or the patient lacks reliable follow up, referral to an emergency department is appropriate.
References
- Mattu A, Tabas J, Brady W. Electrocardiography in Emergency, Acute, and Critical Care. 2nd ed. The American College of Emergency Physicians; 2019.
- LeWinter MM. Acute Pericarditis. NE J Emerg Med. 2017;371(25):349-359. doi:10.1016/j.pcad.2016.12.001
- Cremer PC, Klein AL, Imazio M. Diagnosis, Risk Stratification, and Treatment of Pericarditis: A Review. JAMA. 2024;332(13). doi:10.1001/JAMA.2024.12935
- Witting MD, Hu KM, Westreich AA, Tewelde S, Farzad A, Mattu A. Evaluation of Spodick’s Sign and Other Electrocardiographic Findings as Indicators of STEMI and Pericarditis. J Emerg Med. Published online March 2020. doi:10.1016/j.jemermed.2020.01.017
- Spodick DH. Diagnostic electrocardiographic sequences in acute pericarditis. Significance of PR segment and PR vector changes. Circulation. 1973;48(3):575-580. doi:10.1161/01.CIR.48.3.575
