Published on
Urgent message: Take vital signs and physical examination of the chest with the utmost importance when evaluating a patient with a cough. The common complaint of “cough” in the urgent care setting can be a symptom of a life-threatening pathology.
Frank Schaller, DNP, APRN, FNP-C and Lauren Dunn, MSN, APRN, FNP-C
INTRODUCTION
Cough is a common complaint across healthcare settings including the emergency department (ED), urgent care, and primary care arenas—especially during influenza season.1 Cough is also reported in 50% of patients who test positive for COVID-19 in the U.S.2 Often, a cough is a symptom of a benign pathology, but the clinician should be aware of potentially dangerous pathologies as well.
CASE PRESENTATION
LS is a 52-year-old woman who presents with a chief complaint of 2-3 weeks of cough and shortness of breath. She states her cough is nonproductive with intermittent wheezing. She admits mild chest pain with increased dyspnea on exertion, especially with climbing a flight of stairs. She states it takes several minutes to catch her breath after exerting herself. She states she has chest pain with coughing and deep breathing. She endorses mild orthopnea. She denies fevers, postnasal drip, frequent throat clearing/swallowing, acid reflux, hemoptysis. She is a never smoker, with no environmental exposures other than dust recently cleaning. No recent international travel.
There is no recent surgery or immobility for extended periods of time, no personal or family history of blood clotting disorders, denies calf pain/ swelling, denies hormone therapy.
PMH: Breast cancer in remission 1 year ago
PSHx: Lumpectomy 1.5 years ago
Observations and Findings
Evaluation of the patient showed the following:
| Temperature | 97.0⁰ F |
| Respiratory rate | 20 |
| Pulse | 97 |
| Blood pressure | 116/78 |
| Oxygen saturation | 93% room air |
General/Constitutional: Well appearing, well-nourished in no distress. Oriented x 3, normal mood and affect.
Skin: No rash, prominent lesions, ulcers, or masses. Good turgor.
Ears: Ear canals clear, tympanic membranes clear, ossicles normal appearance.
Pharynx: no erythema, exudates or lesions.
Neck: supple, without lesions, bruits, or adenopathy, thyroid non-enlarged and non- tender.
Cardiac: No cardiomegaly or thrills; regular rate and rhythm, no murmur or gallop
Lungs: Diminished to auscultation and percussion throughout L lung fields
Extremities: no amputations or deformities, cyanosis, edema or varicosities, peripheral pulses intact
Lymphatics: no lymphadenopathy in cervical, maxillary areas
DIFFERENTIAL DIAGNOSIS
- Acute bronchitis
- Pneumonia
- Pulmonary embolism
- Malignant pleural effusion
- Myocardial ischemia
- Congestive heart failure
- Other cardiopulmonary pathology
DIAGNOSTIC STUDIES
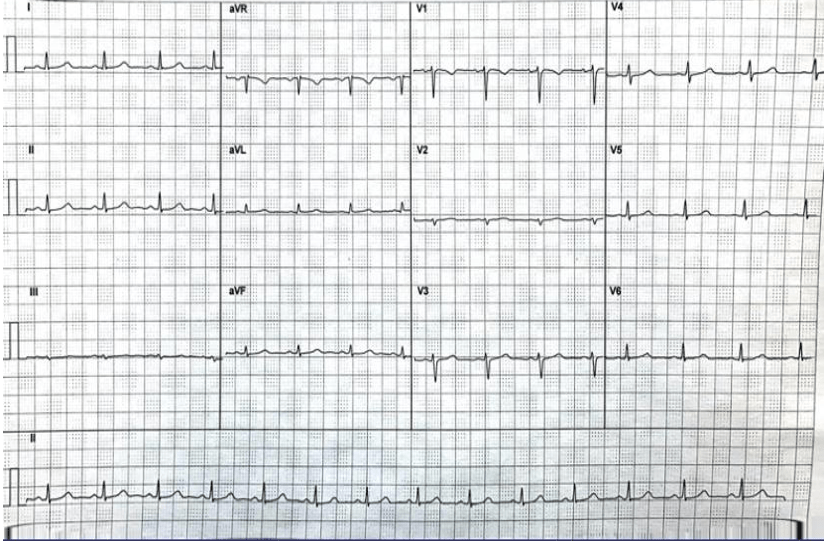
Initially, an ECG and 2-view chest x ray was ordered to rule out acute cardiopulmonary process (see Figure 1 and Figure 2)
Figure 1. Chest Radiograph (AP)
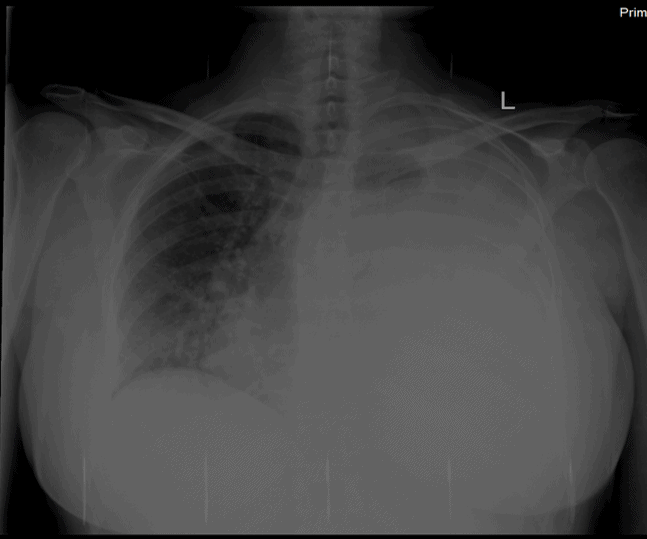
Figure 2. Electrocardiograph
Diagnosis
Tension pneumothorax with associated hemothorax of L lung
ECG; Normal sinus rhythm
This patient was transferred to a local hospital for further workup and management.
TREATMENT AND HOSPITAL COURSE
ED course included chest tube placement requiring subsequent intubation and mechanical ventilation with admission to the ICU. Fluid cytology was sent positive for adenocarcinoma cells concerning recurrent malignancy and stage IV breast CA, Patient was eventually extubated and transitioned to room air. She was evaluated by thoracic surgery, and was able to have her chest tube removed and was discharged in stable condition. She was instructed to follow up with her oncologist outpatient.
DISCUSSION
Cough with pleuritic chest pain and subjective dyspnea are common complaints in urgent care.
Pneumothorax
Clinical features include patient complaints of dyspnea, pleuritic chest pain.3 On physical examination, the clinician may find absent tactile fremitus, hyperresonance to percussion, decreased breath sounds on the affected side. Hypotension may also occur.4 Most common etiologies of pneumothorax include underlying pulmonary disease, mechanical ventilation, chest trauma.
Diagnosis is confirmed by chest radiograph, on which trachea may be visibly shifted to the opposite side of pneumothorax if pneumothorax is large, along with hyperresonance on the affected side.5
Important factors in making this diagnosis included having a low threshold for thoracic radiology when evaluating complaints such as dyspnea on exertion and orthopnea, and considering patient history (breast CA) when evaluating the seemingly routine complaint of cough.
Although a subtle change, the pulse ox of 93% should prompt the clinician for a possible emergent process. It would have been very easy to dismiss this complaint as a viral cough without considering subtle details. Chest radiographs and ECG are fairly inexpensive, minimally invasive procedures that can help establish diagnosis and include or exclude acute cardiopulmonary processes in the urgent care setting. In this case, the provider was able to improve the outcome for the patient by arranging immediate transfer via EMS before clinical deterioration. Additionally, although it was not applicable in this case, a history of pneumothorax is clinically significant in that recurrence occurs in 37% of patients.6
CONCLUSION
Always be meticulous when evaluating the chief complaint of cough—especially in the urgent care setting.
REFERENCES
- Morice AH. Epidemiology of cough. Pulm Pharmacol Ther. 2002;15(3):253-259.
- Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(24):759-765.
- Kelly AM. (2019). 6.6 Pneumothorax. Textbook of Adult Emergency Medicine E-Book, 290.
- Dains JE, Baumann LC, Scheibel P. Advanced Health Assessment & Clinical Diagnosis in Primary Care E-Book. Elsevier Health Sciences. 2018.
- Jarvis’s Physical Examination and Health Assessment E-Book. Elsevier Health Sciences. 2019.
- Tyczynska N, Prasad N, Yealy DM. A 50-year-old man with COPD and dizziness and dyspnea. In: Weinstock MB, Klauer KM, eds. Bouncebacks! Critical Care. Columbus, OH: Anadem Publishing. 2020; 213-241.
