Urgent message: Not all GI complaints can be attributed to gastrointestinal pathology; symptoms of dyspepsia, vomiting, early satiety, weight loss, and abdominal pain may also be from a pelvic etiology.
Fabrizia Faustinella, MD, PhD and L. Alexandre Frigini, MD
INTRODUCTION
Gastrointestinal complaints are common in ambulatory centers, urgent care, and in emergency departments. The symptoms of abdominal pain, nausea, and vomiting account for 12% to 15% of ED visits.1
Several non-GI intra-abdominal, endocrine, and pelvic disease processes can manifest with GI symptoms, notably ovarian masses, abdominal aortic aneurisms, diabetic ketoacidosis, Addison’s disease, nephrolithiasis, and others.2
Previously documented diagnoses of GI disease, such as H pylori, gastritis, GERD, PUD, IBS, etc., should not preclude the clinician from suspecting the presence of new problems and proceeding with further investigation.
CASE PRESENTATION
A 74-year-old woman presented to our clinic with complaints of nausea, vomiting, and worsening abdominal pain for 3 days. Patient stated that she was unable to keep any food or water down. She denied hematemesis or coffee-ground emesis. No fever or chills.
The abdominal pain was described as generalized but seemed to be more prominent in the lower quadrants.
A comprehensive review of systems was positive for weight loss and several GI symptoms which included progressively worsening abdominal distension, flatulence, bloating sensation, early satiety, decreased appetite, constipation alternating with diarrhea, and epigastric and retrosternal burning sensation over a period of many months. There was no family history of ovarian malignancy to the patient’s knowledge.
The patient reported that the abdominal distension was starting to limit her movements and was keeping her from breathing normally, with resulting shortness of breath. She also noticed swelling of the feet and ankles for 2 weeks prior to presentation.
Review of the patient’s EMR revealed many office visits for GI complaints, dating back to at least 2014, for which she was prescribed a variety of PPIs, H2 blockers, sucralfate, dicyclomine (Bentyl), and GI cocktails.
Patient’s social history and medical history were significant for a cholecystectomy performed in 2015, a diagnosis of H pylori infection in 2018 (each followed by adequate treatment), allergic rhinitis, and degenerative joint disease.
Patient’s medications at the time of the visit included famotidine (Pepcid) 20 mg PO QD and cetirizine HCl (Zyrtec) 10 mg PO QD.
Physical exam revealed a well-developed woman, alert and cooperative, with:
- BP 130/82, HR 110, temp 97.5⁰ F, RR 18, SpO2 97%
- Cardiovascular: RRR, no rubs/gallops/murmurs
- Pulmonary: normal breath sounds
- Abdomen: significant distension, soft, normal BS, no fluid wave, generalized tenderness, particularly in the lower quadrants; no rebound tenderness, no rigidity
- Ext: pedal and ankle edema bilaterally
Results of diagnostic studies:
- CBC showed mild anemia, H/H 11.2/34.8, MCV 94.8
- A comprehensive metabolic panel and lipase were within normal limits
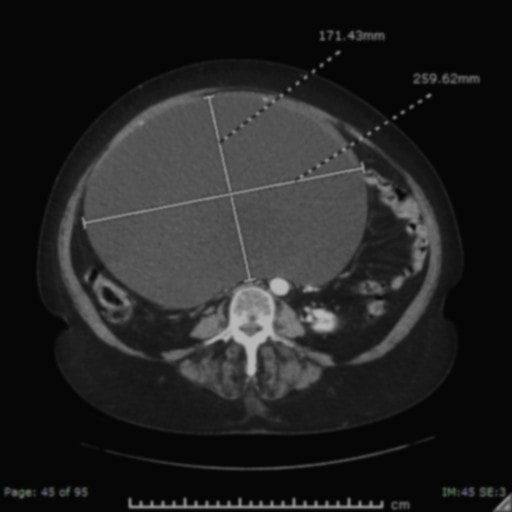
- A CT abdomen and pelvis with contrast was requested and was read as follows:
- Reproductive organs: large cystic mass measuring 25.1×17.9×21.7 cm likely represent a left ovarian cystic neoplasm (see Figures 1, 2, and 3).
Differential Diagnosis
Prior to the CT abd/pelvis, the differential diagnosis was quite broad and included gastric mass, pancreatic pseudocyst, kidney mass, liver pathology/hepatomegaly, hepatosplenomegaly, pyloric stenosis, and so forth. The CT showed a large left ovarian cystic neoplasm with no evidence of malignant features. So, the differential became much smaller and largely limited to the possibility of a large cystadenoma, serous vs mucinous vs endometrioid, or clear-cell cystadenoma.
COURSE AND TREATMENT
The patient was referred to gynecology. Further laboratory investigation included a CA-125 level which was normal. A chest CT did not show evidence of metastatic disease. The patient underwent a THS with BSO. Pathology tissue exam showed a large serous cystadenoma of the left ovary, benign cervix with nabothian cysts, negative for dysplasia, endometrial polyps, atrophic endometrium, unremarkable right ovary, and right fallopian tube with no histopathological alterations.


DISCUSSION
Ovarian cystadenomas are benign epithelial neoplasms with an excellent prognosis.
Epithelial neoplasms of the ovary are classified as benign, borderline, or malignant tumors. They account for 60% of all ovarian tumors and 40% of benign tumors.3
The two most frequent types of cystadenomas are serous and mucinous cystadenomas, whereas endometrioid and clear-cell cystadenomas are rare. Despite advances in imaging studies, a definitive diagnosis of cystadenoma is achieved by histopathological examination of the surgical specimen.
The symptoms and signs associated with cystadenomas generally include pelvic pain, bloating sensation, and discomfort. However, larger masses can trigger many more GI symptoms due to the direct pressure on the bowel and the stomach, as in this patient.
Several imaging techniques are useful in the diagnosis of ovarian cystadenomas. They include pelvic ultrasonography, computed tomography, and magnetic resonance imaging.4 The features more suggestive of a benign cystic neoplasm include unilocularity of the cyst, minimal or no septation, thin walls, and absence of papillary projections.4
The tomographic appearance of our patient’s cyst was consistent with a benign process.
Although our patient underwent a cholecystectomy in 2015, the only imaging study available at that time in our EMR was an abdominal US which showed the presence of cholelithiasis. There was no reference to any visible intra-abdominal mass. All we can infer is that the ovarian cyst must have been present and limited to the pelvic area at that time, only to grow exponentially in the following years.
The management of ovarian cystadenomas depends on symptoms, size of the cyst, age of the patient, medical history, and menopausal state of the patient.5-7
CASE RESOLUTION
Given the size of the cyst and the symptoms our patient was experiencing, a TAH with BSO was performed without delay. After surgery, the patient reported a marked improvement of her GI symptoms, with resolution of the nausea, vomiting, abdominal distension, bloating sensation, abdominal pain, early satiety, and constipation/diarrhea.
CONCLUSION
This case is a reminder that clinicians should keep an open mind when evaluating a patient with recurrent GI symptoms who has been previously diagnosed with a number of GI ailments.
REFERENCES
- Myer PA, Mannalithara A, Singh G, et al. Clinical and economic burden of emergency department visits due to gastrointestinal diseases in the United States. Am J Gastroenterol. 2013;108(9):1496-1507.
- Viniol A, Keunecke C, Biroga T, et al. Studies of the symptom abdominal pain—a systematic review and meta-analysis. Family Practice. 2014;31(5):517–529.
- Buy JN, Ghossain MA, Sciot C, et al. Epithelial tumors of the ovary: CT findings and correlation with US. Radiology. 1991;178(3):811-818.
- Jeong YY, Outwater EK, Kang HK. Imaging evaluation of ovarian masses. Radiographics. 2000;20(5):1445-1470.
- Fatema N, Mubarak Al Badi M. A postmenopausal woman with giant ovarian serous cyst adenoma: a case report with brief literature review. Case Rep Obstet Gynecol. 2018;2018:5478328.
- Gonzalez DO, Minneci PC, Deans KJ. Management of benign ovarian lesions in girls: a trend toward fewer oophorectomies. Curr Opin Obstet Gynecol. 2017;29(5):289-294.
- Muto MG. Ovarian cyst overview. In: UpToDate. Available at: https://www.uptodate.com/contents/ovarian-cysts-beyond-the-basics. Accessed May 27, 2021.
Author affiliations: Fabrizia Faustinella, MD, PhD, FACP, Professor of Medicine, Department of Family and Community Medicine, Baylor College of Medicine. L. Alexandre Frigini, MD, Professor, Department of Diagnostic and Interventional Radiology, Baylor College of Medicine.

