Urgent message: Falls are a common reason for geriatric patients to present for medical care. In this population, even seemingly minor falls can lead to significant injury, and falls may occur in the first place because of serious underlying medical illnesses. It is critical for the urgent care provider to distinguish which of these patients can be treated in the urgent care setting and which require transfer to a higher level of care.
REBEKAH BLICKENDORF, MD
The U.S. population continues to age. By 2030, onequarter of Americans will be older than 65 years.1 Falls are a common reason for this population of patients to present for medical care. Approximately 30% to 40% of this group fall each year.2 In the decade between 2003 and 2013, falls accounted for 62.6% of nonfatal injuries3 and were the leading cause in the geriatric population of nonfatal hospital admissions because of injury.4 Falls are also the leading cause of fatal injury in the geriatric population.4 Although many falls are minor, it is crucial to remember that falls in this population are associated with high morbidity and mortality and loss of independence. One fall generally begets more falls: About two-thirds of geriatric patients who fall will have another fall within the following 6 months,5 and a fall is often the inciting event for a downward spiral of function. serious concern to practitioners working in urgent care centers because such centers treat many such patients and because the majority of elderly patients continue to live in the community either alone or with family members who assist them. Although falls have the potential to cause serious or fatal injury, two-thirds of falls do not result in serious injury.1 The urgent care provider can usually intervene in the many nonserious injuries caused by falls. Although patients with obvious life-threatening pathology will present to trauma centers, patients may sustain injuries with potential for significant morbidity, such as subdural hematomas and hip or extremity fractures, from seemingly insignificant trauma. The urgent care provider must maintain a high suspicion for serious injury in the geriatric patient who has fallen and be prepared to transfer the patient to a facility with resources for a comprehensive evaluation
Just as importantly, the urgent care provider must maintain a high suspicion for why the patient fell. A fall is often a symptom of serious underlying pathology, such as infection, electrolyte imbalance, stroke, or cardiac pathology, even if the patient reports a history of a mechanical fall. The urgent care provider can intervene and prevent future injuries by educating the patient and the family about physical therapy and fall prevention.
Approach to Evaluation
History
It is crucial to obtain a thorough history of the events surrounding the fall, to frame the approach to the workup, treatment, and case disposition. This is often challenging in a patient population that may have baseline neurocognitive deficits. In such situations, seek input from family and caretakers. Attempt to obtain information from witnesses. Determine a timeline of events:
- How long ago did the fall occur?
- Can the patient or the family estimate downtime?
- If there was a significant delay in presenting for care, why was there a delay, and what changed that caused the patient to present now?
Determining the amount of force and the mechanism of injury is important. Knowing the following can help the provider anticipate injury pattern and stratify the patient’s risk for severe injury:
- The height of the fall
- The surface on which the patient fell
- The point of impact on the body
Because a ground-level fall in an elderly patient can lead to significant injury, avoid the trap of accepting the patient’s conclusion that the mechanism was a minor one. Other medical conditions and certain medications may lead to an increased risk for more severe injuries (Table 1).
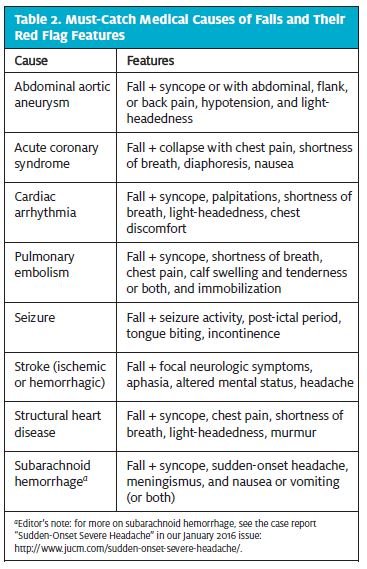
The cause of the fall will determine which way to turn in decision-making. There is a great difference in management of falls that are clearly mechanical (e.g., “I tripped on the garden hose while watering flowers”) and falls that might have been caused by syncope or another underlying medical condition (Table 2). Ask about prodromal symptoms prior to the fall such as the following:
- Light-headedness
- Nausea
- Shortness of breath
- Palpitations
Maintain a high suspicion of syncope, presyncope, or other medical cause of falls that should prompt transfer to an emergency department (ED) for further evaluation.
 It is also vital to obtain a current list of medications. Medications can often predispose patients to falls, and polypharmacy is associated with an increased incidence of falls.2 [Editor’s note: For more on polypharmacy, see the article “Medication Issues in Urgent Care” in the February 2015 issue of JUCM: https://www.jucm.com/medicationissues-urgent-care/.] Table 3 lists medications frequently associated with geriatric falls. Also, the urgent care practitioner should be aware that elderly patients frequently take anticoagulants, which can cause life-threatening internal bleeding from relatively minor trauma.
It is also vital to obtain a current list of medications. Medications can often predispose patients to falls, and polypharmacy is associated with an increased incidence of falls.2 [Editor’s note: For more on polypharmacy, see the article “Medication Issues in Urgent Care” in the February 2015 issue of JUCM: https://www.jucm.com/medicationissues-urgent-care/.] Table 3 lists medications frequently associated with geriatric falls. Also, the urgent care practitioner should be aware that elderly patients frequently take anticoagulants, which can cause life-threatening internal bleeding from relatively minor trauma.
Ask whether this is the first time the patient has fallen or whether falls are recurring. If falls are a new problem, the provider should consider what could have changed with the patient to predispose them to fall. If this has been an ongoing issue, have the patient and the family made efforts to reduce fall risk? Is there a possibility of old untreated injuries?
Obtaining a brief past medical and surgical history is necessary to uncover potential medical illness as a cause of a fall and chronic conditions that may predispose to falls or are associated with risk for more severe injury. Table 4 lists medical conditions associated with an increased risk of falls.
Physical Examination
Vital Signs
A work-up for a patient who has fallen should start with assessment of vital signs. Patients with abnormal vital signs for which the provider cannot easily account should be sent to an ED. Tachycardia and bradycardia may increase suspicion that a fall was caused by arrhythmia. Postural blood pressure changes may also lead to falls. Remember that a “normal” blood pressure in an elderly person may actually be low, considering that the population often has slight hypertension.
Mental Status
Begin with brief orientation questions. Questions about well-known current events may be helpful, as can simply seeing if the patient can provide the history of the fall. Occasionally, patients seem on first interaction to have a normal mental status, but subtle deficits surface as the medical history and physical examination proceed. Family members can help the provider determine whether the patient’s current mental status differs from baseline. Patients with variance from baseline require evaluation in an ED.
General Examination
Lacerations, skin tears, ecchymosis, and joint deformities may be obvious even in a clothed patent. However, failing to have the patient disrobed can cause a provider to miss significant injuries. Likewise, it is impossible to do a good examination of a knee or hip while the patient is wearing pants, or of a shoulder if the patient does not remove a sweater.

Head, Eyes, Ears, Nose, and Throat
Be sure to do the following:
- Examine for obvious signs of facial or head trauma such as deformity, ecchymosis, and hematomas.
- Assess pupils for shape and reactivity, and the conjunctiva for hemorrhage.
- Assess extraocular movement for signs of entrapment and nystagmus.
- Examine the nose for septal hematoma.
- Look for signs of basilar skull fractures, which include ecchymosis behind the ear (Battle sign), periorbital ecchymosis, and hemotympanum.
Patients with hematomas, signs of basilar skull fracture, or findings concerning for facial fracture or injury to the globe will need advanced imaging and consultation with a specialist.
Neck and Back
Assess range of motion and palpate for midline tenderness. Midline tenderness, pain with range of motion, and any report of neurologic symptoms (focal numbness or weakness) should prompt placement of a cervical collar and transfer for advanced imaging.
Geriatric Falls
Cardiopulmonary
Look for signs of injuries to the chest wall—for example, crepitus, bruising, or tenderness (especially to anteroposterior compression). Patients with unequal breath sounds will require chest imaging. An absence of breath sounds suggests pneumothorax, although diminished breath sounds at the lung bases may indicate hemothorax. A murmur found on cardiac examination could indicate that a structural or functional cardiac issue caused the fall.
Abdomen and Flanks
Examine the abdomen and flanks for tenderness, distention, and hematomas. Patients who take anticoagulants may require transfer to an ED for large hematomas of the abdominal wall or flank. In the acute setting, abdominal distention associated with abnormal vital signs should prompt immediate transfer to a facility with access to a surgeon, because of concern for hemorrhage.
Extremities
In most patients, the extremity examination can be focused according to pain and presenting symptoms. For patients who are unable to communicate, a systematic approach is required. Be sure to do the following:
- Document areas of swelling, deformity, or ecchymosis.
- Assess painful joints for range of motion, point tenderness, stability, and crepitus.
- Examine the joint above and below the site of injury, and beware of referred pain (e.g., hip pain may present as knee pain, and arm pain could be due to a neck injury).
- Always assess neurovascular status distal to an injury.
Neurologic Examination
In a patient without head or neck injury or focal symptoms, a simple assessment of gross strength and sensation often constitutes sufficient neurologic examination. Patients with any abnormal findings on a neurologic examination will require transfer to an ED for advanced imaging. The Romberg test, in which the patient stands with the feet together and closes the eyes, tests proprioception, the loss of which can contribute to ataxia and falls.
Gait Assessment
Observing the walking patient is a fundamental part of the neurologic examination. Watch for ataxia and a wide-based gait. Have the patient walk with whatever assist device he or she uses at home. The “get up and go” test is a quick and easy way to assess gait: The patient begins seated in a chair. They are instructed to stand up without using the armrests, walk 10 ft (approximately 3 m), turn around, walk back, and return to a seated position in the chair as quickly as possible. Patients should be able to perform this in <16 seconds. Patients who are unable to do so or who have difficulty completing the test require further evaluation of their strength, gait, and balance.
The urgent care provider often has limited diagnostic resources—sometimes only x-ray and point-of-care laboratory testing. The medical history and physical examination are the most important tools. Many patients will need additional diagnostic studies and will require transfer to an ED.
Point-of-Care Urinalysis
Infection can cause gait change and disequilibrium in the aged. High specific gravity could be a sign of dehydration, perhaps leading to positional hypotension. Hemoglobin can be an indication either of renal injury (leading to red blood cells in the urine) or of myoglobin in the urine, which is associated with rhabdomyolysis (muscle death).
X-Rays
Common sites of fracture include the distal radius, the humerus, and the hip. Rib fractures and vertebral compression fractures are also common in the geriatric population. Rib fractures can be difficult to appreciate on chest x-ray, and computed tomography (CT) scanning may be required for diagnosis. Plain films may miss occult hip fracture, especially femoral neck fracture. If clinical concern for fracture persists despite negative findings on film, the patient should be immobilized and referred for additional imaging.
Common Injuries
Skin Tears and Lacerations
Most skin tears and lacerations can be treated in the urgent care setting with irrigation and primary repair. For simple, superficial injuries, wound glue may be sufficient for closure. Injuries that require suturing can be challenging to repair in the geriatric population because of thin subcutaneous tissue. Techniques for improving success involve suturing through adhesive skin closures (e.g., Steri-Strip closures) placed either horizontally across the wound or vertically along the wound edges.9,10 Patients with especially frail skin may not tolerate sutures and may be simply dressed and bandaged and referred for wound care as necessary. Bio-occlusive dressings may be associated with poor healing and thus are not preferred.
Contusions and Hematomas
Contusions and hematomas due to falls are usually self-limited injuries that can be treated with ice and anal gesia. Patients who have large contusions or hematomas and are taking anticoagulants may require ED referral for CT scanning. This is especially true of abdominal wall hema tomas, which can be of large volume, or flank hema tomas, which can be associated with retroperitoneal hematoma or renal injury. Hematomas that appear to be rapidly expanding should raise concern for arterial injury. Apply direct pressure and transfer the patient to an ED.
Sprain and Strains
Muscle strains and joint sprains generally respond well to conservative treatment such as ice and elevation, pain control, and early mobilization. However, pain and symptom management can be difficult in the geriatric population. Nonsteroidal anti-inflammatory drugs should be avoided in patients with renal insufficiency and should generally be used with caution in the geriatric population. Patients with liver disease may be unable to take acetaminophen. Benzodiazepines are sometimes prescribed for muscle spasm but can lead to drowsiness, instability, and recurrent falls. Before sending patients home, consider how their mobility and their ability to perform activities of daily living will be affected by their injuries. A wrist sprain may be a minor injury for a 22-year-old, but it may render an elderly patient unable to rise from a chair or to use an assist device.
Wrist Fractures
A common fracture pattern after a fall is the FOOSH injury—a fall on an outstretched hand. In geriatric patients, this most commonly leads to fractures of the distal radius. Nondisplaced fractures of the distal radius or the ulnar styloid may be amenable to splinting and outpatient follow-up. Splint preferences vary by provider and may be guided by the recommendations of the orthopedic surgeons that provide follow-up for the urgent care patients. A sugar-tong splint or volar short arm splint is a typical choice. Ensure good follow-up for patients who are given splints, because splints can affect daily functions and the use of assist devices. More frequently, distal radius fractures are significantly displaced with intra-articular involvement, requiring closed reduction. Splint displaced fractures to stabilize the injury, and then transfer the patient to an ED. Open fractures should be covered in a sterile dressing prior to splinting. Patients with neurovascular deficits, skin tenting, or open fractures require urgent fracture reduction and expedited transfer to an ED.
Humeral Fractures
Mid-shaft or proximal humeral fractures are common in the geriatric population because of osteoporosis and age-related bone loss. These fractures may also result from a FOOSH injury with an extended elbow or with direct impact to the humerus. Proximal fractures that are minimally angulated (<45°) and displaced (<1 cm) and uncomplicated mid-shaft fractures can be treated with a sling and swathe, pain control, and early orthopedic follow-up. All other fractures require transfer to an ED for orthopedic consultation. Humeral fractures are associated with several neurovascular complications. A thorough neurovascular examination is essential. Proximal humerus fractures are associated with damage to the axillary nerve or the brachial plexus. Radial nerve injury is a complication seen with mid-shaft and distal humerus fractures. Any patient with motor or sensory deficits requires immediate ED transfer.
Hip Fractures
The majority of patients with hip fractures will present primarily to an ED. Occasionally, however, a hip fracture will present subacutely. Hip fractures are usually clinically and radiographically apparent. When a provider suspects injury despite negative findings on radiographs, the patient should undergo magnetic resonance imaging or CT scanning to rule out occult fracture. Significant pain with weight-bearing and inability to bear weight are red flags. Confirmed hip fractures require hospital admission for surgical treatment. The urgent care provider should document a neurovascular examination prior to transport.
Head Injury
Age-related brain atrophy not only increases the risk of intracranial hemorrhage and injury by minor mechanisms but may also delay the onset of signs and symptoms of intracranial hemorrhage, because more blood can collect before there is a change in significant intracranial pressure. Bridging vessel fragility is another important age-related risk factor. Therefore, providers should maintain a high index of suspicion for intracranial injury in geriatric patients. Up to 26% of these patients may present with a normal findings on neurologic examination and still have intracranial hemorrhage.11 This is especially true of patients who take anticoagulants, including aspirin and clopidogrel. These patients can also have delayed bleeding. Intoxicated patients and those have a history of chronic alcoholism are at high risk as well. The urgent care provider should have a low threshold for transferring the elderly patient who has fallen to an ED for CT imaging. Giving clear discharge instructions to the patient and their caregivers, including signs and symptoms for delayed intracranial bleeding, is paramount.
Neck Injury
Although most patients with gross neurologic deficits will present to the ED, sometimes significant neck injuries can present subtly. Have a low threshold to transfer any patient with significant neck pain for CT imaging. Plain x-rays are no longer the standard of care for evaluating traumatic neck injury and are notoriously difficult to interpret in this age group, given the near omnipresent degenerative changes. A classic injury in the elderly patient who has fallen is central cord syndrome. This occurs from a whiplash injury, because the patient’s neck is extended during impact with an object during a fall. Patients with central cord syndrome present with greater muscle weakness in the upper extremities than in the lower extremities and with loss of sensation to temperature and pinprick in a “cape” distribution. Fracture of the dens is another common injury, and it is potentially unstable. Patients with any suspected neck injury require immobilization with cervical collar and transfer to an ED.
Rib Fractures
Suspect rib fractures in patients with ecchymosis and tenderness of the chest wall, pleuritic chest wall pain, or pain with anteroposterior compression. Nondisplaced rib fractures are frequently radiographically occult, requiring a CT scan for diagnosis. Elderly patients with rib fractures often require admission for pain control and monitoring of their pulmonary status.
Rib fractures in the elderly can be deadly because splinting from pain can lead to atelectasis and pneumonia. Have a low threshold for transferring to an ED patients whose respiratory status is limited by pain even if films do not reveal fracture.
Rhabdomyolysis
Patients with prolonged or an unknown downtime should have a creatinine kinase level checked, which often requires ED transfer. Rhabdomyolysis as a result of immobility after a fall can lead to significant morbidity and mortality because of renal damage, electrolyte abnormalities, and disseminated intravascular coagulation. These patients will require laboratory monitoring and intravenous fluid administration on an inpatient basis. Signs of rhabdomyolysis include tenderness to the muscle, discoloration of the overlying skin, and dark urine. However, patients may have muscle death without these signs or symptoms.
Disposition
Patients whose presentations are concerning for a medical or pharmacologic cause of fall should be immediately transferred to an ED. This is especially important in patients with syncope or presyncope. These patients are frequently admitted for work-up and treatment. Patients with confirmed or suspected significant injuries will require transfer for definitive treatment. Those who are unsteady on gait assessment or who have frequent falls should have a physical therapy assessment. Never hesitate to transfer a patient to an ED if there are immediate concerns about safety in the home.
Even if the patient has no significant injuries after a fall, the urgent care provider has the opportunity to profoundly affect the health of a geriatric patient by identifying modifiable risk factors for falls and counseling the patient and the family about fall prevention. Although the provider may not have the time or the resources to fully address fall-reduction interventions, taking a few minutes to discuss basic fall prevention and the importance of primary-care follow-up is an important component of care of these patients.
Several commonly cited modifications to the home may decrease the risk of falls2:
- Removing throw rugs
- Placing nonslip rugs and assist bars in bathrooms
- Installing additional lighting
- Removing any cords or wires
Other interventions often require input from the primary-care physician, a physical therapist, or another specialist. Although it may not be appropriate for the urgent care provider to modify medications if the cause of falls might be related to polypharmacy, strongly encourage primary-care follow-up for medication modification. If there is concern for visual deficit as a cause of falls, the patient may benefit from an ophthalmology referral. Some patients may benefit from outpatient physical therapy for strength and balance training, home environment assessment and modification, and instruction on how to properly use assist devices.12
Take-Home Points
- Falls in the elderly are common and have the potential for great morbidity and mortality.
- Never assume that a fall is purely mechanical; take a few minutes to elicit a clear medical history to rule out a medical cause of the fall.
- Elderly patients may have significant injuries despite minor mechanisms; maintain a high index of suspicion when obtaining the medical history and performing the physical examination.
- If there are red flags during the work-up in these cases, be ready to transfer the elderly to a higher level of care.
- Even if the patient has only minor injuries, taking the time to provide education and to ensure good follow up can have a profound impact on the patient’s health and on the family.
References
- Sterling DA, O’Conner JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001;50:116–9.
- Rao SS. Prevention of falls in older patients. Am Fam Physician. 2005;72:81–8.
- Centers for Disease Control and Prevention. Injury Prevention & Control: Data & Statistics (WISQARSTM). Atlanta, GA: Centers for Disease Control and Prevention [last updated 2015 December 8; cited 2015 November 6]. Available from: http://www.cdc.gov/injury/wisqars/index.html.
- National Council on Aging. Falls prevention facts. Arlington, VA: National Council on Aging [cited 2015 November 6]. Available from: https://www.ncoa.org/news/resourcesfor-reporters/get-the-facts/falls-prevention-facts/.
- Perry BC. Falls among the elderly. J Am Geriatr Soc. 1982;30:367–71.
- Bauer TK, Lindenbaum K, Stroka MA, et al. Fall risk increasing drugs and injuries of the frail elderly—evidence from administrative data. Pharmacoepidemiol Drug Saf. 2012;21:1321–7.
- Zia A, Kamaruzzaman SB, Tan MP. Polypharmacy and falls in older people: balancing evidence-based medicine against fall-risk. Postgrad Med. 2015;127:330–7.
- Homann B, Plaschg A, Grundner M, et al. The impact of neurological disorders on the risk for falls in the community dwelling elderly: a case-controlled study. BMJ Open. 2013;3:e003367.
- Lin M. Trick of the trade: Steristrip–suture combo for thin skin lacerations. 2011 March 30 [cited 2015 November 6]. In: Academic Life in Emergency Medicine blog [Internet]. 2011. Available from: http://www.aliem.com/trick-of-trade-steristrip-suture-combo/.
- Davis M, Nakhdjevahi A, Lidder S. Suture/Steri-strip combination for the management of lacerations in thin-skinned individuals. J Emerg Med. 2011;3:322–3.
- Mack LR, Chan SB, Silva JC, Hogan TM. The use of head computed tomography in elderly patients sustaining minor head trauma. J Emerg Med. 2003;24:157–62.
- Enderlin C, Rooker J, Ball S, et al. Summary of factors contributing to falls in older adults and nursing implications. Geriatr Nurs. 2015;36:397–406.
