Urgent message: Symptoms from stones in the ureter can mimic other conditions, making for a diagnostic dilemma in urgent care. Imaging is the key to accurate assessment and appropriate treatment.
WILLIAM GLUCKMAN, DO, MBA, FACEP and KATE ABERGER, MD
Ureterolithiasis, which literally translates to stones in the ureter, is sometimes referred to improperly as “kidney stones,” which are properly known as nephrolithiasis. Although stones do form within the kidney, they do not typically cause acute pain. Ureterolithiasis can cause extreme pain, discomfort that sometimes is considered to be worse than experienced with childbirth. Such pain is referred to as renal colic because it waxes and wanes. The abdominal and back pain associated with ureterolithiasis sometimes mimic other conditions, making cases a diagnostic dilemma.
Epidemiology
Seven percent of American women and 12% of American men will develop stones at some time in their lives, and prevalence is rising in both sexes. Incidence is twice as high in individuals who have a family member with stones. Every year in the United States, 2 million people seek outpatient treatment for stones, which is a 40% increase from 1994. In this country, kidney stones account for 1% of hospital admissions, and $2.1 billion in healthcare expenditures per year.
Most kidney stones occur in patients aged 20 to 49, with the peak age of onset at between ages 35 and 45. An initial stone attack in a patient older than age 50 is unusual, and it rarely happens in children up to age 16. The male to female ratio is 3:1. Stones due to infection (struvite) are more common in women, and women have a higher incidence of infected hydronephrosis. Asians and whites have a far greater incidence of stones than do African Americans, Africans, and Native Americans. The recurrence rate for urinary calculi is 50% within 5 years and 70% or higher within 10 years.
Risk
People of low socioeconomic status are at lower risk of ureterolithiasis than are those of higher socioeconomic status. The southern and southwest regions of the United States are known as the “stone belt” because the incidence of stones is higher there than in other areas of the country. Obesity, hypertension, and osteopenia are conditions associated with the disorder. Diet plays a significant role in the incidence of stones. High intake of animal protein and salt and low fluid and calcium intake also are contributing factors.
Stone Types
The four main chemical compositions of renal calculi and their incidence are:
- Calcium (75% to 80%)
- Struvite or magnesium ammonium phosphate (10% to 15%)
- Uric acid (6% to 9%)
- Cystine (1% to 3%)
The main mechanism of stone formation is super saturation. This is a phase change in which dissolved slats condense into solids. Supersaturation depends on the balance of promoters (calcium and oxalate) and inhibitors (magnesium and citrate) of crystallization.
Calcium stones are the most common, comprising about 80% of all cases of ureterolithiasis. These calculi typically are composed of calcium oxalate with a calcium phosphate core, and stones made entirely of calcium phosphate are less common. The characteristic appearance of calcium stones under the microscope is of an envelope. They form in patients who have low urine volume and high concentrations of calcium and oxalate.
Arguably the most important factor in the formation of stones is low fluid intake. Because of that, the volume of urine production is low, which in turn produces high concentrations of stone-forming solutes – calcium and oxalate – in the urine. Hypercalciuria can result from increased dietary intake or overactive calcium absorption, or excess resorption of calcium from bone, as in hyperparathyroidism. Hypercalciuria also can be related to inability of the renal tubules to absorb the calcium in the glomerular filtrate. Decreased levels of magnesium and citrate – the inhibitors of stone formation – in the urinary tract predispose to stone formation.
Once the etiology of a patient’s calcium stones is discerned, treatment can be tailored to the cause. The current trend is NOT to restrict dietary intake of calcium, especially in postmenopausal women. Many studies have shown this to be ineffective and possibly even harmful.
Struvite stones are associated with chronic urinary tract infections (UTIs) caused by gram-negative rods. These specific bacteria are capable of splitting urea into ammonium, which then combines with phosphate and magnesium. The usual bacteria that do this are Proteus, Pseudomonas, and Klebsiella. Escherichia coli cannot split urea. Urine pH usually is greater than 7.
For these types of stones, the infection will not resolve until the entire stone is removed. Underlying etiology for chronic UTIs must be investigated.
Uric acid stones are associated with low pH (less than 5.5) and elevated levels of purine related to high intake of organ meats, fish, or legumes, or because of malignancy. These stones are associated with gout; 25% of patients with uric acid stones suffer from gout. Alkalization of the urine with sodium bicarbonate or citrate (which is converted to sodium bicarbonate) is the mainstay of therapy, plus ensuring adequate hydration. In patients with high serum uric acid levels, allopurinol is useful for lowering serum levels and helping to prevent stone formation, but it will not dissolve an already formed stone.
Cystine stones, which are the rarest type, arise from an intrinsic metabolic defect that results in failure of the kidneys to reabsorb cysteine, ornithine, lysine and arginine. The urine then comes supersaturated and stones form. Diet, binders, and alkalizing agents can be used for treatment.
Stones typically form in the kidney and then enter the ureter. Some stones pass and never cause discomfort, whereas others become stuck in the ureter or begin to rub against the ureter during movement, triggering pain. As a result of the “trauma” to the ureter, patients with stones often have blood in their urine, which can vary from microscopic to gross hematuria.
Work-Up for the Suspected Stone
The first step in work-up for the suspected stone in the urgent care environment is a dipstick urinalysis to evaluate for presence of blood, leukocytes, ketones, and nitrite. Ketosis in the face of vomiting should warrant intravenous (IV) fluid hydration and evidence of infection also should be addressed. Determining whether infection is the sole cause of the patient’s pain or presenting in conjunction with a stone is not always easy.
Microscopy is helpful to identify the presence of crystals, which can help further support a stone diagnosis over other causes of urinary complaints, and a urine culture can rule in or out the presence of bacterial infection. Routine serum renal function testing is not required but should be considered for patients who have a history of renal disease or have or in whom you suspect significant hydronephrosis.
Radiographic imaging (x-ray, computed tomography [CT], ultrasound [U/S]) is very helpful in evaluating stones, as described in the next section of this article. Stone analysis can be useful for determining stone composition, which can help determine preventative measures. Patients who are being treated at home should be given a strainer and asked to return a stone that they pass, if possible.
Imaging for Stones
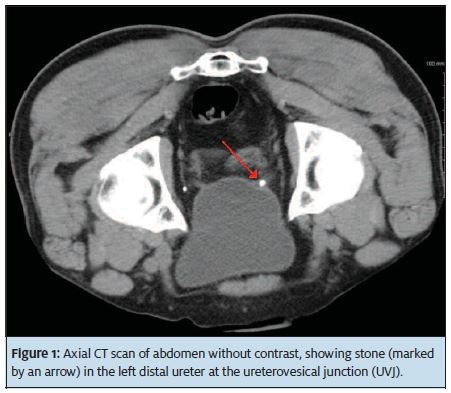
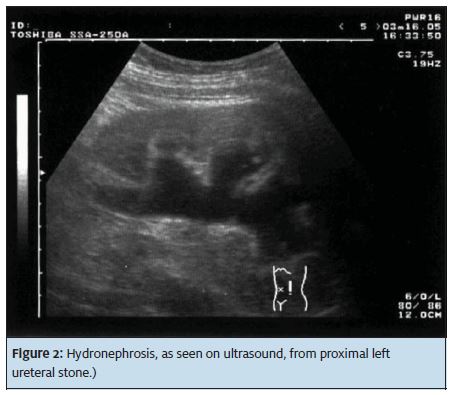
Because 80% of stones are calcium-based and radiopaque, x-ray imaging is useful for diagnosis. A non-contrast enhanced CT scan of the abdomen and pelvis (Figure 1) has a 95% to 100% sensitivity and 95% to 98% specificity and is our preferred initial exam because it provides all of the important initial management information: Stone location, size, number (Stone burden), and extent of hydronephrosis, if present. U/S imaging is limited because it does not demonstrate the exact stone location outside of the kidney and image quality can be affected by obesity and excessive bowel gas. U/S (Figure 2) has the advantage of not using ionizing radiation, which is a consideration in pregnant women, young females, and patients with recurrent stones who may have had several CT scans in the past.
Use of ultra-low dose CT scans, which delivers almost half of the radiation dose of typical Ct scans, also is increasing. On these scans, organs have a more “grainy” appearance because detail is reduced, but they still demonstrate stones very well.
An abdominal x-ray of “flat plate of the abdomen” (KUB) may be useful in the urgent care setting for screening because CT scan and U/S may not be readily available. A KUB also can be used to screen patients with a known history of radiopaque kidney stones. Before the advent and advanced technology of CT scanning and U/S, plan KUB and intravenous pyelograms, in which IV contrast was injected and a series of abdominal plain films were taken, were the main diagnostic modalities. A KUB has a sensitivity of approximately 50% and sensitivity of approximately 75%, thus a negative KUB does not rule out of a stone. A KUB also does not show mild or moderate hydronephrosis, although it can demonstrate severe hydronephrosis.
Management with Medication
Initial urgent care treatment of renal colic is pain management. Intramuscluar (IM), or even better IV, ketorolac is a typical initial medication. The nonsteroidal effect has been shown to prevent ureteral spasm and thus provide very good pain relief. Opiates often are needed to control the pain of renal colic. IM or IV morphine or hydromorphine are good choices. If a patient is not vomiting and can tolerate medication by mouth, a nonsteroidal anti-inflammatory medication, such as naproxen or intranasal ketorolac along with oral oxymorphine or oxycodone/APA for breakthrough pain is a good start. Encouraging the patient to drink lots of fluids such as water (with lemon) and Gatorade also is important. Nausea and vomiting can be managed with metoclopramide or ondansetron parenterally if needed initially, and then orally.
There is literature to support the use of alpha blockers, specifically tamsulosin, administered daily at 0.4 mg. The thinking is that because the distal ureters contain alpha receptors, treatment with drugs may produce enough dilation to permit passage of more stones that reach the ureterovesical junction.
Red Flags in Management
Ureteral stones in the face of infection are potentially problematic. An infection can be difficult to clear with antibiotics alone without addressing the stone. Patients who are febrile and have chills should be evaluated for infection.
Definitive Management
In approximately 80% of patients whose stones are small (that is, < 4 mm) typically, the calculi will pass spontaneously. Stones larger than 4 mm often require surgical intervention such as ureteroscopy and removal with or without stent placement. Patients who have stones > 4 mm with or without hydronephrosis should be referred to a urologist within a few days, and sooner than that if their pain is difficult to control.
Extracorporeal shockwave lithotripsy (ESWL) is another procedure used to treat kidney and proximal ureteral stones. A focused shockwave is generated and targeted at the stone, essentially pulverizing in into smaller fragments that are then passed easily in the urine. Advantages of ESWL include generally less anesthesia time and less risk of ureteral damage. ESWL is considered a first-line treatment and may be advantageous for patients in whom expectant management and unexpected pain may be problematic, such as pilots and surgeons. Patients with a solitary kidney or those at higher risk from longer anesthesia time also may benefit from ESWL.
Admission Criteria
No definite laboratory or radiographic criteria have been established for admission of patients with stones. Clinical judgment should be used to make the determination, but the following situations should prompt admission:
- Ureteral obstruction in a solitary or transplanted kidney
- Ureteral obstruction associated with severe hydronephrosis and/or infected hydronephrosis
- Persistent vomiting and inability to tolerate oral fluids or pain medications
- Pain uncontrolled by oral analgesics
- Acute elevation in BUN/creatinine or worsening of underlying renal insufficiency
Conclusion
Ureterolithiasis is a common cause of flank and abdominal pain. The goal is to rule our other potentially life-threatening causes of pain such as abdominal aortic aneurysm, appendicitis, and diverticulitis, and to control the patient’s pain. Use a diagnostic imaging modality early to solidify the diagnosis and determine if the patient requires urologic referral and intervention of watchful waiting and conservative therapy.
Bibliography
- Berrington de Gonzalez A, Mahesh M, Kim P, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med, 2009; 169(22): 2071-2077.
- Ciaschini MW, Remer EM, Baker ME, et al. Urinary calculi: radiation dose reduction of 50% and 75% at CT – effect on sensitivity. Radiology. 2009; 251(1): 105-111.
- Dellabella M, Milanese G, Muzzonigro G. Efficacy of tamsulosin in the medical management of juxtavesical ureteral stones. J Urol. 2003; 170(6 Pt 1): 2202-2205
- Hall PM. Neprolithiasis: Treatment, Causes, and Prevention. Cleveland Clinic Journal of Medicine. 2009; 76(10): 583-591.
- Kluner C, Hein PA, Gralla O, et al. Does ultra-low-dose CT with a radiation dose equivalent to that of KUB suffice to detect renal and ureteral calculi? J Comput Assist Tomogr. 2006; 30(1): 44-50.
- Miller JC. CT and radiation safety issues. Radiology Rounds. 2010; 8(3)
- National Council on Radiation Protection and Measurement (2009). Report No. 160 – Ionizing Radiation Exposure of the Population of the United States. www.ncrponline.org
- Paulson EK, Weaver C, Ho LM, et al. Conventional and reduced radiation dose of 16-MDCT for detection of nephrolithiasis and ureterolithiasis. AJR Am J Roentgenol. 2008; 190(1): 151-157.
- Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attribute risk of cancer. Arch Intern Med. 2009; 169(22): 2078-2086.
- Soto JA. Ureteral and kidney stones. In: Sahani DV, Samir AE, eds. Abdominal Imaging. Maryland Heights, MO: Elsevier; 2010; 1: 185-189.
- Wasserstein AG. Nephrolithiasis. Am J Kidney Dis. 2005; 45(2): 422-428.
- Wen CC, Coyle TL, Jerde TJ, Nakada SY. Ketorolac effectively inhibits ureteral contractility in vitro. J Endourol. 2008; 22(4): 739-742.
- Wolf SJ Jr., Fields BF. Nephrolithiasis. Medscape. emedicine.medscape.com, emedicine.medscape.com/article/437096overview#aw2aab6b2b4aa. Updated June 16, 2011. Accessed January 23, 3012.
- Wolf SJ Jr., Fields BF. Nephrolithiasis Treatment and Management. Medscape. http://emedicine.medscape.com/article/437096-treatment. Updated January 23, 2012. Accessed February 9, 2010.
Worcester E. Kidney stone disease. J Clin Invest. 2005; 115(10): 2598-2608

