Published on
Urgent message: “Wilderness” medicine is less exotic than one would think. Patients with complaints that began during or after an outdoor outing in any season are likely to present to urgent care, making wilderness medical knowledge of paramount importance.
Stewart Harsant, MMS, PA-C
Introduction
Every season holds its own unique appeal to those who love the great outdoors. Similarly, every season has its own distinct set of risks, ranging from gastrointestinal symptoms, dermatological conditions, and infection from insect bites to external and internal damage from exposure to frigid temperatures. Here, we focus on the proper urgent care management—and pitfalls—of relatively common wilderness-related presentations.
- Infectious Diarrhea
Infectious diarrhea is one of the most common presentations of the wilderness traveler. A common microbe is Giardia, though there are plenty of other culprits. As such, all patients presenting with infectious diarrhea should have a full abdominal exam.
The history should include fever, blood in stool, and weight loss, as well as a detailed travel history including timeline of symptom onset, water source, water treatment, and sick contacts. The exam will often be normal, but consider red flags of surgical illness including severe localized pain, peritonitis, hypotension, or altered consciousness.
Differential diagnosis depends on the geographic region of travel, but often includes Giardia, enterotoxic E coli, enterohemorrhagic E coli, Cryptosporidium, Cyclospora, and viruses. Diagnosis can either be clinical or by testing (eg, stool culture, antigen testing, or testing for ova and parasites).
Management
Most traveler’s diarrhea is self-limiting and requires only supportive therapy such as hydration. Antidiarrheal medication may be used for nonbloody diarrhea. Giardia is treated with metronidazole 2 g PO as a single dose or, alternatively, 500 mg PO twice daily 7 days or tinidazole 2.0g PO as a single dose with food.1 The use of antimicrobials to treat other forms of traveler’s diarrhea should be guided by severity: mild, moderate, and severe.
- Mild diarrhea is tolerable and does not interfere with planned activities. Treatment should entail oral rehydration, loperamide, and bismuth salicylate (BSS). Antimicrobial agents are not recommended. Sports drinks may be used if diluted to half strength with clean water. World Health Organization and the U.S. Public Health Service both have oral rehydration formulas whose recipes are available to the pubic online.
- Moderate diarrhea is distressing, interferes with planned activities, and may be treated with antimicrobials.2 Empiric antibiotics used to treat infectious diarrhea include azithromycin, ciprofloxacin, and rifaximin. Caution should be used when prescribing fluoroquinolones due to increasing resistance worldwide and side effects such as tendinopathy, aortic rupture, and neuropathy.
- Severe diarrhea is incapacitating, prevents planned activities, and should be treated with antibiotics. Strongly consider ED transfer if associated with hypotension and/or intractable vomiting.
Prevention
Infectious diarrhea can be prevented through proper water treatment or drinking bottled water only. As for water treatment modalities, one may disinfect water using heat, filter, chemical, and UV methods. Heat disinfects the most adequately, though other modalities are effective when used properly. If traveling in a developing country, drinking bottled water is advised. Avoid eating fresh fruits and vegetables that may have been washed with contaminated water. Daily BSS is an effective prophylaxis.2
Recent wilderness travel does not exclude a noninfectious or life-threatening cause of diarrhea. As with urban patients, the wilderness traveler can also develop appendicitis, cholecystitis, pancreatitis, bowel obstruction, etc. Patients suspected of having such conditions should be transferred to the ED.
- Contact Dermatitis Due to Exposure to Plants
Common plants that cause dermatitis include poison oak, poison ivy, and poison sumac (Figures 1, 2, and 3). Poison oak and poison ivy are three-leaved plants and can be difficult to distinguish from other nonpoisonous plants, which gives rise to the saying “leaves of three, let it be.” Poison sumac is a shrub or bush with two rows of seven to 13 leaflets. The causative agent for each is urushiol, which is an adherent, heat-stable, and persistent resin found on the leaf surface that can cause a type IV hypersensitivity reaction on the skin of an unsuspecting wilderness traveler. Due to the heat stability of urushiol, brush fires can cause serious respiratory distress. Even if recent wilderness travel is not reported, exposure can happen from urushiol-exposed pets, garden gloves, landscaping equipment, and shoes, with plant dermatitis occurring up to 3 weeks after exposure.3 Differential diagnosis can also include irritant contact dermatitis, impetigo, photocontact dermatitis, and viral exanthem, though diagnosis is largely clinical.
Management
Management depends on severity of reaction. All areas of contact should be rinsed with soap and cold water, as should other possible contacts such as clothes, gear, and pets. Cold water is recommended in order to keep pores closed to minimize urushiol skin penetration.
- Mild reactions can be treated with topical steroids and an oral antihistamine. Calamine lotion and oatmeal baths can offer relief to some patients. Patients should be advised to not scratch the area in order to prevent secondary bacterial infection.
- Moderate reactions involve significant amount of body surface area or regions that cause particular discomfort. If not contraindicated, consideration should be given to a steroid taper, with a duration of 14-21 days, which may help preclude rebound dermatitis.1 Initial IM or IV steroid can be given in the urgent care setting followed by adequate outpatient steroid taper. Note that the fluid in the vesicles is sterile and does not contain urushiol, so a ruptured vesicle does not cause spread or contagion.
- Severe reactions involve respiratory distress. Strongly consider ED transfer.
Figure 1.

Poison oak
Figure 2.

Poison ivy
Figure 3.

Poison sumac
- Tick-Borne Illness
Tick-borne illness should be suspected in any symptomatic patient resident of or with recent travel to endemic areas. Symptoms range from simply dermatologic to constitutional, musculoskeletal, cardiac, and neurological.
Differential diagnosis of tick-borne illness should include Lyme disease, Rocky Mountain spotted fever (RMSF), ehrlichiosis, southern tick-associated rash illness, babesiosis, and tularemia; we will focus on RMSF and Lyme disease.
Blacklegged ticks (commonly referred to as deer ticks) are known vectors for Borrelia burgdorferi, which causes Lyme disease. Dog ticks and wood ticks are known vectors for Rickettsia rickettsii, which causes RMSF.
- Lyme is characterized as primary (erythema migrans), with flu-like symptoms developing shortly after onset; secondary (constitutional, AV block, pericarditis, myocarditis, arthralgia, myalgia, cranial nerve palsy, meningitis, encephalitis); and tertiary (large joint arthritis, neurological symptoms of secondary Lyme). ELISA and Western blot antibody testing for Lyme serological antibody testing may be used to aid in diagnosis but should not delay treatment or rule out need for treatment in patients with clinically suspected Lyme disease. The CDC advises to not delay the empirical treatment of suspected Lyme disease.4
- RMSF presents with onset of fever, chills, sweats, body aches, rash, and headache with the appearance by days 4–7 of a fine pink rash. Just as with Lyme disease, ELISA and Western blot antibody testing for Rickettsia serological antibody testing may be used to aid in diagnosis but should not delay treatment or rule out need for treatment in patients with clinically suspected RMSF. Even with treatment, mortality is 4%. Children have higher rates of mortality than adults.5 The CDC advises to not delay the empirical treatment of suspected RMSF.4,6
Management
Doxycycline 100 mg PO BID x 14-21 days is the treatment of choice to treat both Lyme and RMSF.
- For RMSF, doxycycline is the recommended treatment, regardless of age.7,8
- For Lyme disease, in children <8 years of age and for doxycycline-allergic patients, effective alternatives include amoxicillin, cefuroxime, and ceftriaxone.
- Providers may be hesitant to prescribe doxycycline to children <8 due to staining of teeth, though a 2017 study “failed to demonstrate dental staining, enamel hypoplasia, or tooth color differences among children who received short-term courses of doxycycline at <8 years of age.”7
Tick removal is an unnecessarily daunting task for the urgent care provider. If the tick is still attached to patient, remove the tick by grasping its mouth with tweezers and pulling perpendicular to the attachment point. (See Figure 4.) Do not twist tick, apply petroleum jelly, or touch the tick with a match. Do not attempt to remove retained tick body parts.
Figure 4.
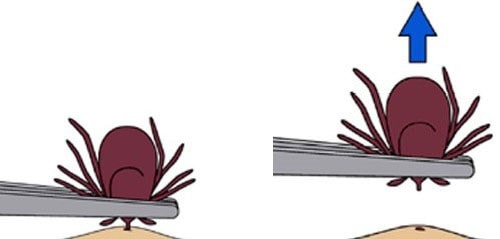
Source: Centers for Disease Control and Prevention
There is controversy regarding chronic Lyme disease; ie, whether persistent Lyme symptoms after treatment are due to ongoing infection or from treated Lyme disease. Prolonged antibiotic treatment in such patients showed no clinical benefit.9 The CDC recommends using the term post-treatment Lyme disease syndrome (PTLDS) as opposed to “chronic Lyme disease”.10
Patients with PTLDS may complain of nonspecific symptoms such as fatigue, headaches, joint and muscle aches, and pain, most of which are difficult to discern from normal aches and pains of daily living. Patients complaining of such concerns should be treated with respect, taken seriously, and referred to their PCP for proper management of such chronic ailments. Further research and evidence are needed to more definitively understand this phenomenon. Patients with confirmed PTLDS should be referred to an infectious disease specialist.
- Frostbite
Frostbite is the freezing of the skin and deeper tissues and can happen in an urban or backcountry environment. The most commonly affected areas are fingers, toes, nose, ears, and cheeks due to vasoconstriction away from the periphery in attempts to maintain adequate core body temperature. Pathophysiology is divided into four overlapping stages:8
- Pre-freeze: Vasoconstriction occurs though no ice crystals have formed yet.
- Freeze-thaw: Both intracellular and extracellular ice crystal formation lead to cell death. After the rewarming and during the thawing process, damage can continue with ischemia-reperfusion injury and ischemia.
- Vascular stasis: Small vessel thrombosis and plasma leakage occur.
- Late ischemia. Ischemia occurs due to progressive tissue ischemia and infarction from inflammatory cascade of thromboxane and prostaglandin, intermittent vasoconstriction, showers of emboli in microvessels, and thrombus formation in larger vessels. Destruction of the microvasculature is the root of continued cell death.
Frostbite is classified as superficial (first- and second-degree), and deep (third- and fourth-degree).
- First-degree presents with numbness and erythema, raised white, yellow plaque at site of injury, and, commonly, mild edema.
- Second-degree results in blisters filled with clear, milky fluid surrounded by erythema and edema.
- Third-degree frostbite produces hemorrhagic blisters, which are indicative of penetration to the reticular dermis, surrounded by erythema and edema.
- Fourth-degree leads to complete penetration through the dermis, resulting in necrosis of deeper structures.
Deep injuries should be referred immediately to the ED. Superficial frostbite victims may be treated safely and effectively in the urgent care setting.
Management
Remove patient from causative cold environment into a controlled, warm environment. Prior to any rewarming intervention, ensure there is no chance of refreezing, as this can lead to more severe injury. The injury should be warmed with warm, gently circulated water (98.6⁰-102.2⁰F, roughly “hot tub temperature”) for at least 15 to 30 minutes or until skin regains pliability and its color returns to normal, red, or purple. You can use a water basin as your warming bath, consistently monitoring temperature. If the water is too hot, it can cause burn injury; if it is too cool, it can delay thawing. Thawing of a body part is very painful, sometimes requiring an opioid analgesic, though NSAIDs are recommended as sole analgesic or in conjunction with opioid to help inhibit the prostaglandin and thromboxane inflammatory cascade, which leads to worsening ischemia and necrosis.8,11 Prior to thawing, it can be difficult to accurately gauge the extent of the injury. As such, if an initially suspected superficial injury demonstrates deep characteristics after rewarming, the patient must be transferred to a higher level of care.
Do not:
- Rub or massage the area in attempt to thaw.
- Attempt rewarming with dry heat (eg, fire or a heater) because this temperature is not controlled. Frostbitten skin with decreased sensation can be prone to burn injury without the patient being aware. If too cool, it can delay thawing.
- Debride blisters, especially hemorrhagic blisters, as this will increase risk of infection.
After the rewarming process has been completed and it is clear that the injury is superficial, apply topical aloe vera ointment and wrap in gauze every 6 hours; like NSAIDs, this helps to decrease the inflammatory cascade after rewarming to prevent further injury. Rest and elevate the affected body part. If injuries are on toes or feet, avoid weightbearing until completely healed. Update tetanus vaccine if needed. Prophylactic antibiotics are not recommended.11 One can expect tissue loss with deep injuries, and no tissue loss with superficial injuries. Concurrent hypothermia may also be present in frostbite victims and should be treated accordingly. Patients with superficial frostbite that you have treated in your urgent care should be re-evaluated the next day.
Prevention
Frostbite can be prevented by adequate preparation, including proper gear and clothing, being aware of the weather forecast, and having an evacuation plan that you decide on prior to leaving for wilderness activity. It is said that “cotton kills” because it absorbs moisture, including sweat, and accelerates body heat loss, increasing vasoconstriction, ultimately increasing risk of frostbite. Layering with moisture-wicking performance material or wool clothing is recommended.
- Hypothermia Due to Exposure
Hypothermia is a serious and life-threatening condition that can happen in any season, even in temperate and tropical climates. Additional risk factors include alcohol ingestion and overexertion (eg, running a marathon) leading to fatigue, sweating, and dehydration. Heat is lost from the body through the mechanisms of conduction (body to object), convection (body to air or liquid), radiation (electromagnetic wave), and evaporation (sweat, respiration).
The pathophysiology of hypothermia is due to tissue cooling which results in a decreased resting metabolism and an impairment of neurologic function, the severity of which correlates to lower core body temperatures.12 Patient presentation may range from being cold, shivering, and nonhypothermic to profoundly hypothermic, in cardiac arrest, and coma.
Diagnosis is made by measuring the core body temperature. Hypothermia is defined as having a core body temperature <35⁰C and is classified as mild, moderate, severe, and profound.
- Mild hypothermia temperatures are 35⁰C to 32⁰C
- Moderate, 32⁰C to 28⁰C
- Severe, 28⁰C to 24⁰C
- Profound <24⁰C8,13
The best means to obtain an accurate core temperature in the urgent care setting is by using a rectal thermometer. Oral, infrared tympanic, and temporal thermometers should be avoided due to inaccuracy of measurements. Oral thermometers may be used only to rule out hypothermia.
- Mild: Patients in mild hypothermia will manifest uncontrollable shivering and have varying levels of alertness and hemodynamic stability. Vital sign abnormalities such as tachypnea, tachycardia, and hypertension may be present. Urinary frequency is common due to increased renal blood flow from vasoconstriction. Shivering increases metabolism, cardiac output, ventilation, and mean arterial pressure. Shivering is triggered at core body temperature of approximately 37⁰C and starts to decrease at 32⁰C. Patients will lose their ability to shiver at <30⁰C, which is an ominous sign.
- Moderate: Patients in moderate hypothermia will have a minimal to completely absent capability of shivering. Depressed vital signs are common, and include hypotension, decreased heart rate, and decreased respirations. Mental status will be altered, and patients may have dilated pupils with muscle rigidity. Cardiac arrhythmias are common at such core body temperatures, and can be precipitated by even the slightest of stimulation of the periphery such as taking one’s wet clothes off.
- Severe: Severely hypothermic patients will be in a coma with dilated pupils and muscular rigidity. Pulse may be barely palpable as the heart rate drops to as low as 10-20 beats per minute. Life-threatening cardiac arrhythmias, such as ventricular fibrillation, are common at such temperatures and tend to be recalcitrant to chemical or electrical conversion until rewarming is accomplished.
- Profound: Profound hypothermia is defined as <24⁰C, at which point the patient has a high likelihood of cardiac arrest and death.
Management
The degree of hypothermia guides management (see Table 1).
The patient with mild hypothermia who is shivering, has no altered mental status, has no concurrent trauma or co-morbidities, and is hemodynamically stable may be safely treated in the clinic. Such patients should be kept horizontal, as standing can lead to a drop in BP and hemodynamic instability. Wet clothing should be removed by cutting, taking care to minimize peripheral stimulation, which may precipitate cardiac arrhythmia. Rewarming methods should include insulating patient with blankets, towels, sleeping bag, dry clothes, etc. Warming equipment such as warm water bottles or warming pads may be placed in the axillae and groin. Always place a barrier between warming equipment and the patient’s skin to avoid causing burn.
Once the patient has been rewarmed to 37⁰C, is hemodynamically stable and unaltered, and has been horizontal for at least 30 minutes, they may attempt to stand. At this point they may be seated upright and given warm liquids and foods rich in carbohydrates to meet the elevated metabolic demand.12 These patients should have next day follow-up visits and should be given strict ED precautions. They should remain indoors, warm, and insulated from the outside environment.
All other hypothermia patients should be referred to the ED. While waiting on EMS transfer for the hypothermic patient, warming methods should be initiated. Remove wet clothing by cutting. Keep the patient horizontal and insulated. Be prepared to perform CPR and have the AED ready if necessary. Table 1. Staging and Treating Accidental Hypothermia
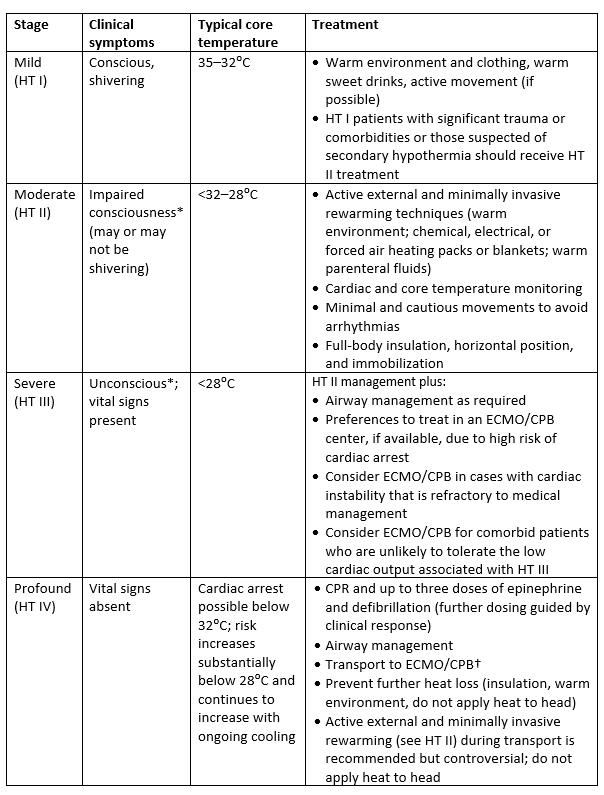
Adapted from: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 8th ed. New York, NY: McGraw-Hill Education; 2016.
Prevention
Hypothermia can be prevented by wearing proper clothing, staying dry, taking shelter as needed, and having an evacuation plan.
Teaching Points
- Doxycycline is the recommended treatment for RMSF, regardless of age.
- A prolonged steroid taper of 14-21 days is the preferred treatment for poison ivy.
- Azithromycin, not ciprofloxacin, is the first-line empiric antimicrobial choice for infectious traveler’s diarrhea.
- Hypothermia can happen in any season, even in temperate and tropical climates.
Citation: Harsant S. Top 5 wilderness medicine presentations for the urgent care provider. J Urgent Care Med. June 2019. Available at: https://www.jucm.com/top-5-wilderness-medicine-topics-for-the-urgent-care-provider/.
References
- Curtis G, Lewis AC. Treatment of severe poison ivy: a randomized, controlled trial of long versus short course oral prednisone. J Clin Med Res. 2014;6(6):429-343.
- Riddle MS, Connor BA, Beeching NJ, et al. Guidelines for the prevention and treatment of travelers’ diarrhea: a graded expert panel report. J Travel Med. 2017;24(suppl 1):S57-S74.
- Miller DM, Brodell RT, Herr R. Wilderness dermatology: prevention, diagnosis, and treatment of skin disease related to the great outdoors. Wilderness Environ Med. 1996;7(2):146–169.
- Centers for Disease Control and Prevention. Tickborne Diseases of the United States: A Reference Manual for Healthcare Providers. 5th ed. Centers for Disease Control and Prevention; 2018.
- Centers for Disease Control and Prevention. Fatal cases of Rocky Mountain spotted fever in family clusters — three states, 2003.” Available at: www.cdc.gov/mmwr/preview/mmwrhtml/mm5319a1.htm. Accessed May 10, 2019.
- Biggs HM, Behravesh CB, Bradley KK, et al. Diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever and other spotted fever group rickettsioses, ehrlichioses, and anaplasmosis – United States. MMWR Recomm Rep. 2016;65(No. RR-2):1-44.
- Todd SR, Dahlgren FS, Traeger MS, et al. No visible dental staining in children treated with doxycycline for suspected Rocky Mountain spotted fever. J Pediatr. 2015;166(5):1246-1251.
- Ingerbretsen R. Advanced Wilderness Life Support: Prevention, Diagnosis, Treatment, Evacuation. Wilderness Medical Society; 2016.
- Oliveira CR, Shapiro ED. Update on persistent symptoms associated with Lyme disease. Curr Opin Pediatr. 2015;27(1):100–104.
- Maloney EL. Controversies in persistent (chronic) Lyme disease. J Infus Nurs. 2016;39(6):369-375.
- McIntosh SE, Opacic M, Freer L, et al. Wilderness Medical Society practice guidelines for the prevention and treatment of frostbite: 2014 update. Wilderness Environ Med. 2014;25(4 Suppl):S43-S54.
- Zafren K, Giesbrecht CG, Danzi DF, et al. Wilderness Medical Society practice guidelines for the out-of-hospital evaluation and treatment of accidental hypothermia: 2014 update. Wilderness Environ Med. 2014;25(4 Suppl):S66-S85.
- Strapazzon G, Procter E, Paal P, Brugger H. Pre-hospital core temperature measurement in accidental and therapeutic hypothermia. High Alt Med Biol. 2014;15(2):104–111.
Stewart Harsant, MMS, PA-C is an adjunct faculty member in Rush University’s PA program. The author has no relevant financial relationships with any commercial interests.
