Identifying Risk Factors in Preparticipation Physicals for Young Athletes
Urgent message: Doctors in the US and Europe are divided over what the cardiovascular component of a proper sports physical should include. Here is a reasonable approach.
NATHAN P. NEWMAN, MD, FAAFP
Sudden death in young athletes is not new. In 490 BC, when the Greeks improbably defeated the invading Persians at Marathon, a young herald, Phidippides, ran 25 miles back to Athens to announce the victory, whereupon he collapsed and died on the spot.1 Now, over 2,500 years later, the sudden death of an athlete while playing high school, college, or professional sports is still a rare event, but when it occurs, the ensuing shock and grief can shatter a community and devastate a nation.
Sports, in and of themselves, are rarely a cause of increased risk of death, but they can be the environment that triggers sudden death in athletes with predisposing heart or blood vessel abnormalities. Some wellknown athletes who have been victims of sudden deathinclude marathon runner Jim Fixx (1984), Olympic volleyball star Flo Hyman (1986), NBA basketball stars “Pistol Pete” Maravich and Hank Gathers (1990), and Darryl Kile, all-star pitcher for the St. Louis Cardinals (2002).1 Last March, a 16-year-old Michigan high school
basketball star, Wes Leonard, collapsed on the court after making the game-winning layup and later died of sudden cardiac arrest.2
Death in athletes in the United States can be due to a number of causes, many unrelated to cardiovascular dis- eases. Korey Stringer, an offensive tackle with the Min- nesota Vikings, died of heat stroke in 2001.3
Unfortunately, heat stress diseases and dehydration cause unexpected deaths annually throughout the country. Other reported causes include exercise-induced asthma, sickle cell trait, head and spinal trauma, rhabdomyolysis, and exercise-induced anaphylaxis. This review focuses on cardiovascular causes of sudden death in athletes.
The purpose of preparticipation screening is to identify those cardiovascular diseases responsible for athletic deaths in order to disqualify those at risk. The scope of screening needed to prevent sudden death is controversial. For example, should electrocardiography (ECG) or echocardiography be a routine part of the evaluation? The European Society of Cardiology recommends ECG for all high school and college athletes before athletic participation. Would this process reduce sudden deaths in the US athletes? This issue will be addressed later in this article.
Incidence of Sudden Death in Athletes
In our country, sudden death most commonly occurs in football or basketball, accounting for two-thirds of all sudden deaths of athletes. Soccer is the sport most com- monly associated with sudden death in the rest of the world. The exact frequency with which sudden death occurs in young athletes (those under 35 years of age) is unknown, as such data are limited. It has been reported that cardiovascular-related sudden death occurs in 1 to 2 in 200,000 high school athletes annually.1
The US National Registry of Sudden Death in Athletes reports that such deaths have increased at a rate of 6% per year. The proportion of deaths reported is predominately higher in male athletes. However, sudden deaths in female athletes have notably increased, reaching 12% in 2006. This may be a result of the increased numbers of female athletes participating in organized sports. Interestingly, the age at death showed no trend for change over time.4
Goals of Cardiovascular Assessment
The purpose of preparticipation screening is to determine the medical eligibility of athletes based on evaluations of several organ systems. The cardiovascular portion of the screening is focused on reducing cardiovascular risks associated with participating in athletics. It is important to note that once a potential cardiac abnormality is detected, subspecialty referral for further diagnostic testing is an appropriate next step.
A review of guidelines for preparticipation physicals shows that they relate primarily to mass screening of high school and college athletes of all races and both genders.5 However, these recommendations may also apply to athletes in youth (<13 years of age) or masters (>40 years of age), as well as to evaluations in other venues, such as individuals who are evaluated primarily in office practice settings.
Intense athletic activities may act as a trigger to increase the risk for sudden cardiac death in athletes with underlying heart disease. Most young athletes who die suddenly of cardiovascular disease do so during sports training or competition. So there appears to be a relationship between intense physical activity and sudden death. The key to preparticipation screening is the early detection of clinically significant cardiovascular disease and, at least in some cases, allow for timely therapeutic interventions that may alter the clinical course and prolong life.
Causes of Sudden Cardiac Death
Atherosclerotic coronary artery disease is the primary pathological finding in individuals >40 years of age who die during physical activity from cardiovascular causes, whereas inherited cardiovascular conditions are primarily responsible for deaths in younger athletes. Hypertrophic cardiomyopathy (HCM) accounts for most (36%-44%) of these deaths in American athletes.4 Other abnormalities—including anomalous coronary arteries (17%), myocarditis (6%), arrhythmogenic right ventricular cardiomyopathy, mitral valve prolapse, intramyocardial coronary arteries, coronary artery dis- ease, aortic stenosis, and aortic rupture—are associated with many of the remaining deaths (all less than 5%).4 Athletes who smoke or have hypertension, diabetes, hyperlipidemia, or a strong family history of heart dis- ease are at an increased risk of heart attack. Jim Fixx, the renowned marathoner, who died suddenly of coronary artery disease at age 52,1 had been an overweight smoker with high cholesterol before taking up running. His father had died of a heart attack at age 43. Reports indicated that he had adamantly refused cardiac testing even though he had been noting chest pains prior to his heart attack.
Autopsy revealed three-vessel coronary artery disease.6 A similar situation occurred when Darryl Kile, a pitcher for the St. Louis Cardinals, died suddenly at age 33.1 The cause of death was attributed to a 90% blockage in two coronary arteries. His father had died of a heart attack at age 44.
Hypertrophic cardiomyopathy
HCM is the most common cause of sudden death due to cardiovascular disease in the US, accounting for about one-third of these events. HCM is an inherited disorder, characterized by an asymmetrically hypertrophied and non-dilated left ventricle. Sudden death is likely due to ventricular tachyarrhythmias.7
Pathologic hypertrophy vs “athlete’s heart”
An important delineation exists between physiologic hypertrophy or “athlete’s heart” and pathologic conditions. In physiologic hypertrophy, cardiac mass increases in response to systemic training in dynamic (aerobic) and/or isometric (static) exercises. The structural remodeling noted in many athletes with this condition includes enlargement of the left and right ventricles and left atrium; however, the function of the heart remains preserved.8 Physiologic hypertrophy can some- times present diagnostic challenges, especially when the echocardiographic dimensions are outside of clinically normal values.7
Unhealthy cardiac hypertrophy (pathological hyper- trophy), on the other hand, is a response to stress or dis- ease such as hypertension, myocardial infarction, valvular heart disease, or neurohormones. Pathological hypertrophy also leads to an increase in muscle mass, but the muscle does not increase its pumping ability. Instead it accumulates myocardial scarring (collagen). In pathological hypertrophy, the heart can increase its mass by up to 150%, with the potential for sudden cardiac death.9,10
Congenital coronary artery anomalies
Another common cardiovascular cause of sudden death in athletes is congenital coronary artery anomalies. The most common of these anomalies is when the left main coronary artery originates from the right sinus of Valsalva.7 Any history of chest pain or syncope should alert the clinician to the possibility of a coronary anomaly.11 A resting ECG exercise electrocardiogram may not be abnormal because the myocardial ischemia is episodic. This limits the value of random screening for coronary anomalies.12-14 The most likely cause ofischemia is either acute-angle kinking at the origin of the coronary artery or compression of the anomalous artery between the aorta and pulmonary trunk during exercise.
Myocarditis
Myocarditis has been associated with sudden cardiac death in its active or infectious phase or even in its healed stages due to arrhythmias.15 It may also be the consequence of drug abuse. Myocarditis may be challenging to diagnose clinically. A histological examination may be required with endomyocardial biopsy.
Marfan syndrome
Marfan syndrome is an inherited, degenerative disorder of the connective tissue.16 Several organ systems are affected, including the ocular, cardiovascular, and skeletal systems. The number and severity of symptoms vary from person to person. In a typical case, the affected individual is taller than average for his age, is nearsighted, has an arm span exceeding his height, is loose-jointed (espe- cially in the knees, wrists, and fingers), is excessively flexible, and may have kyphoscoliosis. Olympic volleyball star Flo Hyman had undiagnosed Marfan syndrome and died of aortic rupture sitting on the sidelines of a volley- ball game. A three-week-old clot was found around the tear, indicating that an earlier rip in the same spot had already begun to heal when the fatal second rupture occurred in her aorta.17 Florida State basketball player Ronalda Pierce also died from an aortic rupture that was thought to be a result of this syndrome.18
Other cardiovascular causes
About 2% of young athletes who die suddenly have normal cardiac structure at autopsy, and death is presumed to be due to ion-channel disorders (eg, long QT syndrome22 and Brugada syndrome23), Wolff-Parkinson- White syndrome,24 and coronary vasospasm.
Other Noncardiac conditions
Athletes without underlying heart disease have been victims of sudden cardiac death following a seemingly innocent blow to the chest by a baseball or hockey puck. This is called “commotiocordis” or “cardiac concussion.” Death presumably occurs due to ventricular fibrillation.1
Performing the Preparticipation Screening
The tremendous number of athletes requesting preparticipation physical examinations (approximately 12 million per year) and the rarity of cardiac disorders causing sudden death (<0.3%) are major barriers to effective screening.25 US high school and college athletes’ preparticipation evaluations are typically restricted to history taking and a physical examination. Only 3% of trained athletes who died suddenly of heartdisease were suspected of harboring cardiovascular disease on the basis of a history and physical examination during screening.21
Clinical history
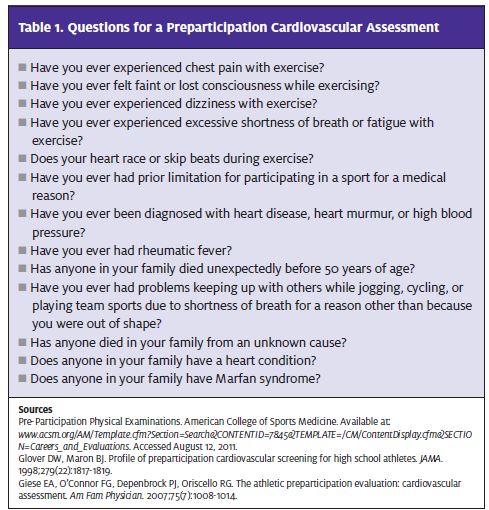
A complete clinical history is more likely to uncover a cardiovascular abnormality than the physical examination portion of a preparticipation screening. Likewise, physicians are more likely to recommend limiting activity due to a history indicating possible cardiovascular concerns than due to clinical findings on examination.26,27 If any of the history questions yields a positive response, further questioning and evaluation are recommended (Table 1). If possible, the athlete’s parents should be involved in answering questions about their child’s history.28
The keys to the preparticipation cardiovascular examination are blood pressure measurement, palpation of radial and femoral pulses, and dynamic cardiac auscultation. A quick screen for Marfan syndrome should also be considered when athletes may have common characteristics for this disorder.25,29,30 Blood pressure should be measured while the patient is seated using an appropriately sized cuff. If an athlete’s blood pressure is initially high, have the patient sit quietly for about five minutes and repeat the reading at least twice to ensure an accurate reading. Hypertension in children and adolescents is defined as an average sytolic blood pressure and/or diastolic blood pressure that is above the 95th percentile on at least three occasions for the patient’s sex, age, and height. Recommended guidelines for evaluation of hypertension this age group are shown in
Table 2.
In adult athletes (>18 years of age), stage 1 hypertension is defined as blood pressure greater than 140/90 mm Hg. Stage 2 hypertension is defined as blood pressure greater than 160/100 mm Hg. Blood pressure readings indi- cating Stage 2 hypertension or any evidence of target-organ damage should prompt discontinuation of athletic participation until a full evaluation is conducted and the hypertension is controlled.31
An athlete’s heart rate and rhythm can be easily determined by palpation of the radial and femoral pulses. The pulse should have a smooth, rapid upstroke, a smooth summit, and a more gradual downstroke.32 The radial and femoral pulses should be synchronized without significant delay. Coarctation of the aorta may be evidenced by a diminished or delayed femoral pulse relative to the radial pulse.
Athletes with HCM may have a large-amplitude, rapidly rising pulse or a double-peek pulse. Alternatively, athletes with a small-amplitude, slowly rising pulse may have aortic stenosis and low cardiac output (congestive heart failure). Any significant variation of alternating strong and weak pulse may signal left ventricular systolic dysfunction. Any irregular rhythm may indicate arrhythmia or a conduction problem.
Many preparticipation sports examinations are per- formed in gymnasiums or other large venues, making auscultation of the heart challenging. The cardiac examination is best performed in a quiet setting. First, inspect the precordium to look for any asymmetry or abnormal impulses. Then palpate the chest wall to detect any thrill or parasternal heave. Next, with your stethoscope, listen carefully for any murmurs, extra heart sounds, and splitting of the first and second heart sounds (ie, S1 and S2). Remember that the S2 is composed of closure of the aortic valve followed by closure of the pulmonic valve. As we inspire, increased blood flow into the pulmonary vascular bed occurs, slightly delaying closure of the pulmonic valve. This widening of the S2 (“physiologic split”) can be a sign of normal cardiac function.32 Any narrowing of the S2 split may be a sign of severe aortic stenosis, HCM, or left bundle branch block. A “fixed split,” with- out inspiratory changes of the S2, may be a sign of atrial septal defect.33

Murmurs are particularly important to detect. They may vary due to location, intensity, timing, and character. Some murmurs may be difficult to hear. Dynamic auscultation, or having the patient perform a squat-to- stand exercise or the Valsalva maneuver, may change the intensity of the murmur.32 Increasing stroke volume usually causes murmurs to become louder (with squat- ting) and decreasing stroke volume may make murmurs quieter (with standing or the Valsalva maneuver). On the other hand, HCM or mitral valve prolapse should be considered if a murmur is softer when the patient squats or is louder or longer when he returns to a standing position or during the Valsalva maneuver.29,34
Marfan syndrome, a genetic disorder of the connective tissue, may be suspected due to characteristic clinical manifestations (Table 3). Aortic root dilatation is a common trait and can cause aortic dissection and sudden death. Further evaluation may include electrocardiography, slit-lamp eye examination, and echocardiography.32
Red Flags
If syncope or presyncope, palpitations, dyspnea and easy fatigue, exertional chest pain, or family history of sudden death are present, further evaluation may be warranted.
Syncope or presyncope
Exercise-related syncope or presyncope may indicate HCM from left ventricular outflow tract obstruction or ischemia from congenital coronary anomalies. Other causes may be due to hypoglycemia, side effects from medications, or a vasovagal reaction.35 Participation in athletics is not recommended when being evaluated for syncope and/or pr syncope. Referral to a cardiologist should be considered if no cause can be determined. 35-37
Athletes who experience palpitations should be evaluated for arrhythmia.32 Characteristics of abrupt or gradual onset, regular or irregular heart rate, and frequency of episodes and their relationship to exercise may be important. Supraventricular tachycardia may occur with an abrupt onset with a rapid heart rate and stop with vagal maneuvers. On the other hand, sinus tachycardia may have a slower onset and gradual resolution with exercise.32 Ventricular arrhythmias may also cause symptoms of palpitations. Common ven-ricular arrhythmias include long QT syndrome or arrhythmogenic right ventricular cardiomyopathy. Comprehensive evaluation of an athlete’s use of tobacco, caffeine, alcohol, over-the-counter drugs, supplements, and illegal drugs should be conducted. If these questions do not lead to a probable cause, basic laboratory testing should be performed, including TSH, electrolytes, and an ECG. Possible review of event monitor or Holter evaluation may be considered if no clear etiology is determined. Athletes should not engage in sports until further evaluation is conducted by a cardiologist.32
Dyspnea and easy fatigue
Complaints of dyspnea on exertion and easy fatigue are difficult to evaluate. They may simply be the result poor conditioning. However, they may also be signs of anemia, exercise-induced asthma, an underlying cardiovascular disorder, or primary pulmonary hypertension.32 If an athlete with dyspnea has a past history of high blood pressure, hyperlidemia, or other cardiac abnormalities, echocardiography should be considered prior to exercise testing to rule out aortic stenosis and HCM.32
Exertional chest pain
Symptoms of exertional chest pain in young athletes demand further evaluation, although the cause may simply be exercise-induced asthma.29 Exertional chest pain can be a sign of ischemia from coronary artery abnormalities or left ventricular outflow tract obstruction from HCM.7 However, a resting ECG or exercise stress test may not detect the episodic nature of this ischemia. Diagnosis might require a cardiology consultation for further diagnostic imaging including echocardiography or cardiac catheterization.
Family history of sudden death
Any athlete’s family history of premature sudden death (ie, <50 years of age) must be evaluated thoroughly.32 Further diagnostic tests—including ECG, echocardiography, and exercise stress testing, as well as fasting lipids—should be considered.32
Electrocardiography: To Test or Not to Test?
The ECG has been reported to be abnormal in up to 75%-95% of patients with HCM.29 An ECG may also identify individuals with the long QT syndrome or Brugada syndrome, and it may raise suspicion of myocarditis by premature ventricular complexes and ST-T abnormalities. Despite this, an ECG may not be a viable addition to a preparticipation history and physical examination screening of US athletes. A key reason: ECGs are commonly misread—even by experts.
A study published in the Journal of Pediatrics last July reviewed the accuracy of pediatric cardiologists reading ECGs with common cardiac abnormalities causing sudden death in athletes vs normal con- trols.38 Results noted a sensitivity of only 68% and a specificity of 70% for recognition of ECG abnormalities by US cardiologists. The false-positive and false-negative rates were 30% and 32%, respectively. The investigators concluded that preparticipation screening ECGs are difficult to interpret and mistakes in ECG interpretation— even by cardiologists—could lead to high rates of inappropriate sports guidance and overuse of ancillary diagnostic tests.
These results appear to validate the common belief on this side of the Atlantic that preparticipation screening of US athletes with ECGs would not duplicate the results of a 25-year-long Italian study.39 In this study, the rate of sudden cardiac death among competitive athletes in Italy was reported to have been significantly reduced by including ECGs in preparticipation physicals as standard procedure. However, these physicals were performed—and the ECGs evaluated—by sports physicians and other cardiovascular specialists “with extensive clinical experience with young competitive athletes.”
In the US, the situation is quite different. Here, primary care physicians perform the majority of the 12 million-plus preparticipation physicals conducted each year. The results of the Italian experience may not translate in a country in which evaluation of competitive athletes by non-cardiologists is the rule.32,40 Given the rarity of HCM and other cardiac anomalies requiring accurate reading of ECGs to detect, changing our system to include specialist evaluation of ECGs would not be a cost-effective approach.41
Automated External Defibrillators: To Adopt or Not to Adopt? Identifying an athlete predisposed to sudden cardiac death with a preparticipation physical examination is one way to prevent this devastating event. But what if an athlete has sudden arrhythmia? A cohort study published in 2009 reviewed the use of automated external defibrillators (AEDs) in US high schools. There were 36 cases of sudden cardiac arrest (SCA) reported between December 2006 and July 2007 for athletes and non-athletes at the responding 1,710 high schools. Of the 36 SCA cases reported, 35 (97%) were witnessed, 34 (94%) received bystander cardiopulmonary resuscitation, and 30 (83%) received an AED shock. Twenty-three SCA victims (64%) survived to hospital discharge. The investigators concluded that school- based onsite AED programs could provide high survival rates for SCA victims. As more people participate in strenuous activities and exercise programs, availability of AEDs and coordinated emergency response programs should be considered a standard for all locations where athletic competition and participation occur.42
Conclusion
Cardiovascular-related sudden death in high school and other athletes is rare but worrisome. Common causes include hypertrophic cardiomyopathy, congen- ital coronary artery anomalies, myocarditis, and Marfan syndrome. Obstacles to diagnosis include the large number of student athletes needing preparticipation physicals each year, the rarity of the condition, the cost of ECGs and echocardiograms, and the high rate of ECG misreadings, even by cardiologists. A good clinical history is likely to detect more cardiovascular anomalies than a physical examination, the main components of which are blood pressure measurement, palpation of radial and femoral pulses, dynamic cardiac auscultation, and, in athletes with common characteristics of the disorder, screening for Marfan syndrome. If syncope, presyncope, palpitations, dyspnea and easy fatigue, exertional chest pain, or family history of sudden death are present, further evaluation may be warranted. n
References
- McMicken D. Sudden death in athletes. Hughston Clinic Website. Available at: www.hughston.com/hha/a_16_4_4.htm. Accessed August 17, 2011.
- Wes Leonard collapsed on court. ESPN.com news services. Available at: http:/ sports.espn.go.com/ncaa/highschool/news/story?id=6180469. Accessed August 15, 2011.
- Korey Stringer. Available at: http://en.wikipedia.org/wiki/Korey_Stringer. Accessed August 15, 2011.
- Maron, BJ. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the Unites States, 1980-2006. 2009, 119:1085-1092.
- Maron BJ, Thompson PD, Ackerman MJ, et Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Car- diology Foundation. Circulation. 2007;115(12):1643-1655.
- Altman The doctor’s world; James Fixx: the enigma of heart disease. New York Times. July 24, 1984. Available at: www.nytimes.com/1984/07/24/science/the-doctor-s-world- james-fixx-the-enigma-of-heart-disease.html. Accessed August 19, 2011.
- Maron Sudden death in young athletes. N Engl J Med. 2003;349(11):1064–1075.
- Salberg Sudden Death in Athletes Registry. Hypertrophic Cardiomyopathy Founda- tion. Available at: www.4hcm.org/hcm/scainathletes/40256.html. Accessed August 19, 2011.
- Weber KT, Clark WA, Janicki JS, Shroff Physiologic vs pathologic hypertrophy and the pressureoverloaded myocardium. J Cardiovasc Pharmacol. 1987;10(suppl 6):S37-S50.
- Maron BJ. Distinguishing hypertrophic cardiomyopathy from athlete’s heart: a clinical problem of increasing magnitude and Heart. 2005; 91(11):1380-1382.
- Goldschlager N, Epstein AE, Grubb PB, et Etiologic considerations in the patient with syncope and an apparently normal heart. Arch Intern Med. 2003;163(2):151-162.
- Basso C, Maron B, Corrado D, Thiene Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden death in young competitive athletes. J Am Coll Cardiol. 2000;35(6):1493-1501.
- Davis JA, Cecchin F, Jones TK, Portman Major coronary artery anomalies in a pedi- atric population: incidence and clinical importance. J Am Coll Cardiol. 2001;37(2):593-597.
- Post JC, van Rossum AC, Bronzwaer JC, et Magnetic resonance angiography of anomalous coronary arteries. A new gold standard for delineating the proximal course? Circulation. 1995;92(11):3163-3171.
- Maron BJ, Pelliccia A, Spirito Cardiac disease in young trained athletes. Insights into methods for distinguishing athlete’s heart from structural heart disease, with particular emphasis on hypertrophic cardiomyopathy. Circulation. 1995;91(5):1596-1601.
- National Marfan About Marfan Syndrome. National Marfan Foundation Website. Available at: www.marfan.org/marfan/2280/About-Marfan-Syndrome. Accessed August 19, 2011.
- Volleyball Hall of Flo Hyman. Available at: www.volleyhall.org/hyman.html. Accessed August 24, 2011.
- Ronalda Pierce. Available at: http://en.wikipedia.org/wiki/Ronalda_Pierce. Accessed August 19, 2011.
- Maron Cardiovascular risks to young persons on the athletic field. Ann Intern Med. 1998;129(5):379-786
- Van Camp SP, Bloor CM, Mueller FO, et Nontraumatic sports death in high school and college athletes. Med Sci Sports Exerc. 1995;27(5):641-647.
- Maron BJ. Sudden death in young competitive athletes. Clinical, demographic, and pathological JAMA. 1996;276(3):199-204.
- Priori SG, Schwartz PH, Napolitano C, et Risk stratification in long-QT syndrome. N Engl J Med. 2003;348(19):1866-1874.
- Brugada J, Brugada R, Antzelevitch C, et Long-term follow-up of individuals with electrocardiographic pattern of right bundle-branch block and ST-segment elevation in precordial leads V1 to V3. Circulation. 2002;105(1):73-78.
- Wellens HJ, Rodriguez LM, Timmermans C, Smeets The asymptomatic patient with Wolff-Parkinson-White electrocardiogram. Pacing Clin Electrophysiol. 1997;20(8 pt 2):2082- 2086.
- Maron BJ, Thompson PD, Puffer JC, et Cardiovascular preparticipation screening of competitive athletes. A statement for health professionals from the Sudden Death Com- mittee (clinical cardiology) and Congenital Cardiac Defects Committee (cardiovascular dis- ease in the young), American Heart Association. Circulation. 1996;94(4):850-856.
- Beckerman J, Wang P, Hlatky Cardiovascular screening of athletes. Clin J Sport Med. 2004;14(3):127-133.
- Joy EA, Paisley TS, Price R Jr, et Optimizing the collegiate preparticipation physical evaluation. Clin J Sport Med. 2004;14(3):183-187.
- Mick TM, Dimeff RJ. What kind of physical examination does a young athlete need before participating in sports? Cleve Clin J 2004;71(7):587-597.
- Preparticipation Physical 3rd ed. New York, NY: McGraw-Hill; 2004:19-23, 47-50.
- Maron BJ, Douglas PS, Graham TP, et Task Force 1: preparticipation screening and diagnosis of cardiovascular disease in athletes. J Am Coll Cardiol. 2005;45(8):1322–1326.
- National Heart, Lung, and Blood The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. NHLBI Web- site. Available at: www.nhlbi.nih.gov/health/prof/heart/hbp/hbp_ped.pdf. Accessed August 17, 2011.
- Giese EA, O’Connor FG, Depenbrock PJ, Oriscello The athletic preparticipation eval- uation: cardiovascular assessment. Am Fam Physician. 2007;75(7):1008-1014.
- National High Blood Pressure Education Program Working Group on High Blood Pres- sure in Children and The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 suppl 4th report):555-576.
- Chizner The diagnosis of heart disease by clinical assessment alone. Dis Mon. 2002;48(1):7-98.
- O’Connor FG, Oriscello RG, Levine Exercise-related syncope in the young athlete: reassurance, restriction or referral? Am Fam Physician. 1999;60(7):2001-2008.
- Maron BJ, Zipes Introduction: eligibility recommendations for competitive athletes with cardiovascular abnormalities—general considerations. J Am Coll Cardiol. 2005;45(8):1318–1321.
- American Academy of Pediatrics Committee on Sports Medicine and Cardiac dysrhythmias and sports. Pediatrics. 1995;95(5):786-788.
- Hill AC, Miyake CY, Grady S, Dubin Accuracy of interpretation of preparticipation screening electrocardiograms. J Pediatr. 2011 July 9. [Epub ahead of print.]
- Corrado D, Pelliccia A, Bjornstad HH, et Cardiovascular preparticipation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005;26(2):516-524.
- Murry PM, Cantwell JD, Heath DL, Shoop The role of limited echocardiography in screening athletes. Am J Cardiol.1995;76(11):849-850.
- O’Connor DP, Knoblach Electrocardiogram testing during athletic preparticipation physical examinations. J Athl Train. 2010;45(3):262-272.
- Drezner JA, Rao AL, Heistand J, et Effectiveness of emergency response planning for sudden cardiac arrest in United States high schools with automated external defibrillators. Circulation. 2009;120(6):518-525.