Urgent message: Chest pain in young adults is often benign but it’s important to always consider conditions that increase risk of cardiovascular disease when evaluating these patients.
RAFAEL ILYAYEV, MD, FACP, MOHAMED A. MOHAMED, MD, AND HASSAN FARHAT, MD
Overview
This case illustrates the importance of considering and ruling out rare causes of coronary artery disease (CAD) in young patients who present with chest pain. One of these rare causes is a hypercoagulable state secondary to homocysteinemia, which can be associated with other vascular events including stroke. The case presented here illustrates the approach to management and work up of chest pain in young patients to identify the underlying cause of CAD.
Case Presentation
A 25-year-old African-American male with a past medical history of diabetes mellitus and hypertension presented with a complaint of left-sided chest discomfort associated with some shortness of breath for 3 days. His pain score was 10/10 and the pain was constant, pressure-like, and radiated to the left shoulder. He denied palpitations, lower extremity swelling, orthopnea, cough, fever, chills or dizziness.
Observations and Findings
Physical examination revealed a patient in moderate distress with the following vital signs:
Temp: 98.5oF
Pulse: 123
RR: 22
BP: 136/90
O2 Sat: 98%
The patient’s chest was clear with bilateral air entry. Tachycardia was present but no murmurs, gallop or rub. The patient’s abdomen was soft, non-tender and bowel sounds were normal. Neurological exam also was normal.
Laboratory and Test Results
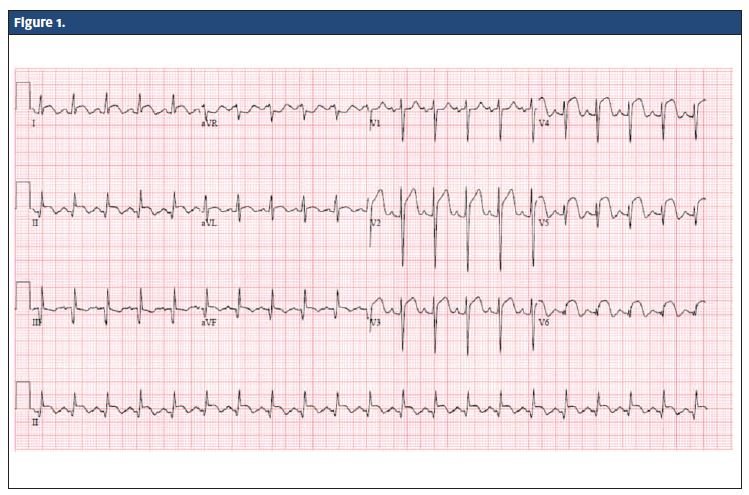
Urine toxicology was negative for cocaine. Figure 1 shows the patient’s electrocardiogram (EKG).
Diagnosis
ST elevation myocardial infarction (STEMI) as demonstrated on EKG by ST elevation in leads I & aVL, V2-3-4-5-6 (Acute Anterolateral STEMI) and old inferior MI (Q waves in lead III, aVF). Upon further questioning, the patient revealed that he had an acute MI 5 years ago with stent placement in the proximal left anterior descending (LAD) coronary artery.
Additional laboratory tests, including complete blood count, complete metabolic profile, and coagulation profile were normal but cardiac enzymes were elevated, with troponin 12.3 ng/mL.
Course and Treatment
The patient was transferred to a nearby facility and percutaneous coronary intervention was performed, which showed a patent proximal LAD stent and 100% distal LAD occlusion (Figure 2) due to thrombus. Thrombectomy was performed with about 30 mL of blood and the thrombus was aspirated. Echocardiogram showed left ventricular apical thrombus with ejection fraction 40%.
This was a very unusual case in that the patient was a young man who had experienced two MIs.
The patient’s diabetes, while certainly a risk factor for premature CAD, was thought to be a less likely cause given that it had been well-controlled for some time. (His HbA1C was 5.6 g/dL 2 months prior). Therefore, further work up for additional risk factors was done, including C-ANCA, P-ANCA, antiphospholipid antibodies, and anticardiolipin antibodies. All results came back negative. Additional investigations were done and revealed an elevated homocysteine level at a value of 34.4 g/dL (normal = 0 to 15 g/dL).
Upon further questioning the patient revealed that he had a cerebrovascular accident at age 19. Review of previous records confirmed the history as evidenced by presence of a thrombotic cerebellar stroke on CT and MRI (Figures 3 and 4).

Discussion
Homocysteinemia appears to be an independent risk factor for cerebrovascular, peripheral arterial, and coronary heart disease (CHD) and for venous thromboembolic disease. Homocysteine has primary atherogenic and prothrombotic properties. Histopathologic hallmarks of homocysteine-induced vascular injury include intimal thickening, elastic lamina disruption, smooth muscle hypertrophy, marked platelet accumulation, and the formation of platelet-enriched occlusive thrombi.1 Sensitive assays allow quantification of the total plasma homocysteine concentration, with the following values: Moderate (15 to 30 μmol/L), intermediate (30 to 100 μmol/L) and severe (>100 μmol/L).
Hyperhomocysteinemia has been linked to the following vascular events:
- MI, other acute coronary syndromes, and recurrent coronary events;
- Premature CHD;
- Cardiovascular and total mortality;
- Adverse outcomes after angioplasty; and
- Carotid artery stenosis, stroke, recurrent stroke, and silent brain infarct.2
Acute pericarditis is an inflammation of the sac surrounding the heart, the pericardium, which usually lasts <6 weeks. It is by far the most common condition affecting the pericardium. That is evident on ECG as diffuse, positive, ST elevations with reciprocal ST depression in aVR and V1.3
Brugada Syndrome is a genetic disease that is characterized by abnormal EKG findings and an increased risk of sudden cardiac death. EKG shows ST elevations in leads V1-V3 with a right bundle branch block appearance with or without the terminal S waves in the lateral leads. A prolongation of the PR interval (a conduction disturbance in the heart) is also frequently seen.4
EKG changes of hyperkalemia include peaked T waves, widening of the QRS complex in severe hyperkalemia, and the EKG complex can evolve to a sinusoidal shape.5
Conclusion
It is crucial to consider a hypercoagulable state as a cause of CAD in young patients who present with chest pain. Patients with a hypercoagulable state, such as the homocysteinemia seen in our case, are at risk of vascular events including CAD and stroke. Although acute coronary syndrome is rare in those ages 18 to 35, some conditions significantly increase the risk and should always be explored carefully before concluding that their chest pain has a benign, non-cardiac cause.
References
- Nygård O, Nordrehaug JE, Refsum H, et al Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med. 1997;337(4):230-236.
- Arnesen E, Refsum H, Bønaa KH, et al. Serum total homocysteine and coronary heart disease. Int J Epidemiol. 1995;24:704–709. [PubMed]
- Khandaker, MH, Espinosa RE, Nishimura RA, et al:; Pericardial disease: diagnosis and management. Mayo Clinic Proc. 2010;85(6):572–593.
- Nademanee K, Veerakul G, Nimmannit S, et al. Arrhythmogenic marker for the sudden unexplained death syndrome in Thai men. Circulation. 1997;96(8):2595–2600.
- Wrenn, KD, Slovis, CM, Slovis BS. The ability of physicians to predict hyperkalemia from the ECG. An Emerg Med. 1991;20(11):1229–1232.
