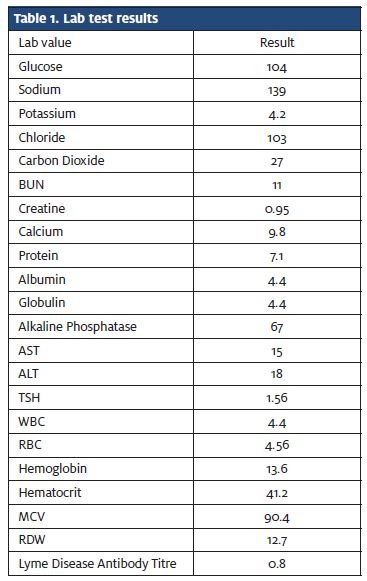
Published on
Urgent message: The key to this case was in the details of the presenting symptoms in the patient history: Alarm symptoms including extreme fatigue and weight loss, which warranted further diagnostic work up.
ABRAR KHAN, MD, MBA, REVATHY NAIR, MD, and MARIANN MELICHAREK, MD, FACEP
Introduction
Sarcoidosis is a multisystem granulomatous disorder of unknown etiology. Most patients with sarcoidosis present to urgent care providers with symptoms such as cough, dyspnea, chest pain, eye pain and/or skin lesions. These symptoms should not go unnoticed because most cases of sarcoidosis are diagnosed through incidental radiologic findings. The case we present underscores the importance of obtaining a solid history from the patient. Further investigative studies are often warranted, despite routine complaints and a normal physical exam, especially if “alarm symptoms” are present, that is, weight loss, fatigue, loss of appetite, mental status changes, motor and sensory changes, or vision changes.
Case Presentation
A 32-year-old Caucasian male presented to the urgent care center with “fevers of up to 102°F” for about 2 days. In addition to the fever, he presented with a sore throat, which he describes as aching. The patient reports no cough, chills, or hemoptysis. Further diagnostic questioning reveals some back pain and fatigue with a 20-lb weight loss over the past “few months.” The patient was seen 8 months prior for a similar complaint, which he said got better with azithromycin, Proventil inhaler, and prednisone. A chest x-ray taken at the time was read as normal (Figure 1).
The man’s past medical history is significant for acid reflux and sciatica. At the time of evaluation the patient was taking rabeprazole. He reported no known malignancies in his family history and his social history was negative for smoking (quit in 2010). He admitted to being a social drinker and has never used illicit drugs.
Observation and Findings
Observation of the patient revealed the following vital signs:
- BP – 111/69 mmHg
- P – 94
- RR – 16
- T – 98.7° F
- SpO2 – 98%
- Height – 5’ 11”
- Weight – 170 (change from 8 months prior, 190 lb)
- BMI – 25.80 (change from 8 months prior, 26.5)
The patient’s physical exam was within normal limits. However, he had several “alarm” symptoms, including weight loss and fatigue that warranted further investigation.
Labs/Imaging
- Rapid Strep A antigen
- Throat Culture
- Chest X-ray (frontal and lateral)
- CBC
- BMP
- TSH/Free T4
- Lyme Disease Serology
The initial encounter of pharyngitis warranted immediate testing with a Rapid Strep Test, which was negative. The culture was sent for laboratory analysis (later reported as negative) and a chest x-ray was performed with frontal and lateral views. The attending physician noticed that the right hilum appears abnormal and comparison with the patient’s previous chest x-ray suggested that the right hilum was enlarged. The patient’s current chest x-ray was sent to Radiology as a STAT read.
At that point, the patient was allowed to return home and discharged with specific instructions for follow up with his primary care provider. Chest x-ray impressions were read 8/21/2013 (Figure 2). Table 1 lists results of lab tests, which do not reveal any abnormalities.

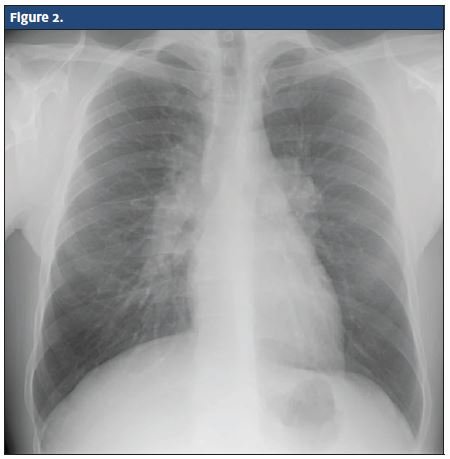
The Radiology report on the chest x-ray confirmed bilateral hilar lymphadenopathy and recommended a thoracic computed tomography (CT) scan to differentiate between sarcoidosis and lymphoma. The thoracic CT scan revealed enlarged hilar and mediastinal lymph nodes with small bilateral pulmonary nodules. The Radiology report also recommended further follow up for a differential diagnosis including sarcoidosis and lymphoma. The patient then was referred to a pulmonologist for follow up and diagnosis.
Diagnosis
Sarcoidosis
Discussion
In urgent care medicine, one must know that a single solitary diagnostic test should not deter a physician from paying attention to the history of present illness. The patient described here does not fit the typical profile for sarcoidosis, but his presentation of fatigue, weight loss, and chronic symptomology should evoke suspicion even after the negative strep test.
Epidemiology
Sarcoidosis is a disease of inflammation of unknown etiology, characterized by the presence of non-necrotizing granulomas along the lymphatic tract of the lungs. The estimated prevalence is 10 to 20 per 100,000. The disease appears to vary in incidence amongst various ethnicities. It seems to be more prevalent in the black population, however, at a 2.4% lifetime risk versus 0.85% in the white community.1 Sarcoidosis is predominately seen in African-American women. Seventy to 90% of cases of sarcoidosis are seen in patients aged 10 to 40 years.2
Clinical Presentation
Sarcoidosis can appear in practically any organ of the body, but it originates most often in the lungs and lymph nodes. Thus, the most common presenting symptoms include cough, dyspnea, and chest pain. Other features of sarcoidosis include fatigue, malaise, fever, and weight loss,2 which were apparent in this case. On physical examination of the lungs, wheezing may also be present.2
Lung involvement occurs in over 90% of patients with sarcoidosis.3 Chest radiography at this time is both an accessible and cost-effective initial imaging diagnostic study for sarcoidosis. The classic chest x-ray finding is bilateral hilar adenopathy. However, that finding may be absent, or if present, may occur in combination with parenchymal opacities.4 The stage of pulmonary involvement is based on the chest x-ray findings. Although the x-ray can be useful in terms of anatomical findings, it is not a good predictor of disease activity or outcome.
In this case, x-ray exhibited right-sided hilar lymphadenopathy, which required follow up with CT to assess whether sarcoidosis or lymphoma was present. Although the results of the CT were inconclusive and no further diagnostic studies were required, CT and high-resolution CT radiography are superior to chest radiography in assessment of the degree of pulmonary parenchymal disease and lung fibrosis. CT and high resolution CT may show parenchymal disease in patients with normal chest radiographs or in those patients who demonstrate only hilar lymphadenopathy on chest xray. CT can also serve as a guide for lung or lymph node biopsy, and may be also used to evaluate response to therapy.5
Treatment
Most patients with pulmonary sarcoidosis do not require treatment because their disease is asymptomatic, limited disease, spontaneously remits. For patients with asymptomatic pulmonary sarcoidosis and no substantial extra pulmonary involvement, initiating therapy with oral glucocorticoids is not compulsory. Symptoms, chest radiograph, and pulmonary function should be monitored at 3- to 6- month intervals. Oral glucocorticoids have been the most commonly used agents for the relief of symptoms and control of potentially disabling respiratory impairment from pulmonary sarcoidosis, even if they do not cure the disease.4-6
The standard dose of oral glucocorticoids is the equivalent of prednisone 0.3 to 0.6 mg/kg ideal body weight (usually 20 to 40 mg/day). The initial dose of prednisone is continued for 4 to 6 weeks.7 If a patient’s symptoms, radiographic abnormalities, and pulmonary function tests are unimproved, oral prednisone should be continued for another 4 to 6 weeks at the dosage initially prescribed. In patients who are stable or whose symptoms are improving, the drug dosage can be tapered gradually.8
References
- Thomas KW, Hunninghake GW. Sarcoidosis. JAMA. 2003;289(24):3300-3303.
- Sharma OP. Fatigue and Sarcoidosis. Eur Respir J. 1999;13(4):713-714.
- Baughman RP, Teirstein AS, Judson MA, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med. 2001;164(10 Pt 1):1885-1889.
- Baughman RP. Pulmonary Sarcoidosis. Clin Chest Med. 2004;25(3):521-530, vi.
- Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med. 2007;357(21):2153-2165.
- du Bois RM. Corticosteroids in sarcoidosis: friend or foe? Eur Respir J. 1994;7(7):1203-1209.
- Baughman RP, Costabel U, du Bois RM. Treatment of sarcoidosis. Clin Chest Med. 2008;29(3):533-448, ix-x.
- Schutt AC, Bullington WM, Judson MA. Pharmacotherapy for pulmonary sarcoidosis: a Delphi consensus study. Respir Med. 2010;104(5):717-723.