Urgent message: The COVID-19 worldwide pandemic has changed sports as we know it. Returning athletes back to sport safely continues to be widely debated among physicians in cardiology, primary care, infectious disease, and sports medicine. The return-to-play process after a COVID-19 infection will depend on the severity of their infection, duration of symptoms in the context of any concerning past medical history, and/or family history.
Brian Harvey, DO and Natalie Stork, MD
CASE PRESENTATION
A 15-year-old male presented to the urgent care seeking clearance after his COVID-19 infection. His symptoms lasted for 5 days and included loss of taste, cough, sore throat, and fatigue. He reports he had 3 days of fever at the start of his symptoms. Currently, he is asymptomatic and has not had symptoms for the past 2 weeks. He is an avid football athlete and wants to return as quickly as possible.
INTRODUCTION
SARS-CoV-2 is a novel coronavirus that causes a multitude of symptoms known as COVID-19, which has continued to spread exponentially across the world, killing millions, including over 600,000 in the United States. When the United States economy “shut down” in March of 2020, sports participation, ranging from professional to recreational, followed suit. Within a few short months, mitigation strategies in sport led to the resumption of practice and competition, even as the pandemic continued to spread.
As cases continued to rise, more information was discovered about COVID-19, including its effects on the athlete. SARS-CoV-2 can affect most major organs, including the cardiovascular system.
COVID-19 commonly affects the adult heart, with up to 78% of adult patients demonstrating changes on imaging or laboratory testing.1 Concern regarding the impact this virus may have on the cardiovascular system of athletes, and specifically the potential for sudden cardiac death in the athlete, quickly arose. The possibility of arrhythmias, particularly ventricular arrhythmias associated with myocarditis, has been an area of focus in sports medicine.
In May of 2020, these alarming reports led to initial recommendations for the evaluation of all athletes who had had history of COVID-19, prior to returning to sport. At the time, a conservative approach to the evaluation was recommended, with consideration to include screening electrocardiograms, laboratory evaluation, echocardiogram, and cardiac magnetic resonance imaging.2
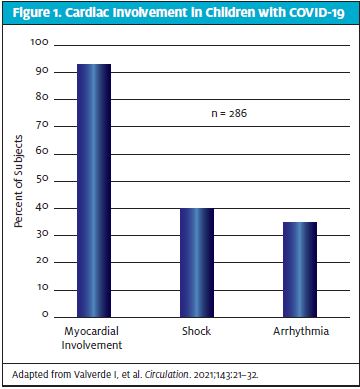
As pediatric cases increased, multi-inflammatory syndrome in children (MIS-C) has been reported. While there is still ongoing research, cardiac involvement in MIS-C has been high. Cardiac arrhythmias were shown to be present in 35% of hospitalized patients and echocardiographic changes, including 24% having coronary artery abnormalities3. However, cardiac involvement remains less defined currently in asymptomatic and mildly symptomatic pediatric patients.
In more recent studies, cardiac involvement in the young-adult, collegiate, and professional athlete has been reported at a much lower rate, ranging from 0.5% to 3%.4 As more evidence has been published, recommendations on how adult and college athletes return to play have changed. The most recent recommendations on screening the pediatric athlete after a COVID-19 infection have come from the American Academy of Pediatrics, updated in August of 2021.5
TREATMENT/RETURN TO PLAY STRATEGIES
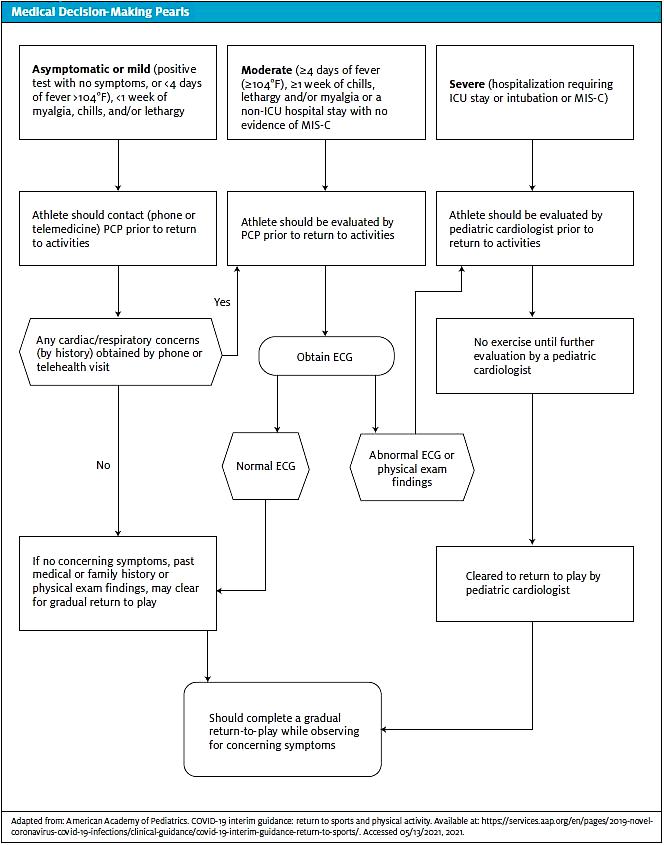
In the asymptomatic athlete, defined as no symptoms with a positive test, as well as mild symptoms (defined as fever 100.4° for ≤4 days, <1 week of chills, lethargy, myalgias), it is recommended to have at least a telehealth visit or a phone call with the primary care physician prior to returning to participation in sport. During the screening process, if there are any symptoms by history, it is recommended to have an in-office evaluation that consists of a full cardiac screen questionnaire, full physical exam, and consideration of an ECG. If there are any abnormalities or concerns, a referral to cardiology is warranted. If there are no concerning findings, a slow return to play process as described later in this article is recommended.
For a moderate illness in the athlete (as defined as symptoms ≥4 days of symptoms, ≥1 week of chills, lethargy, myalgias OR non-ICU hospitalization), it is recommended that an in-office evaluation be performed prior to the return to sport. Again, this would include a cardiac questionnaire, physical exam, and an ECG. If there are any concern or abnormalities, a referral to cardiology should be made. If there are no concerns, following the return to play process is recommended.
For severe infections, defined as an ICU stay, intubation, or diagnosis of MIS-C, athletes should be followed clinically by pediatric cardiology. Athletes are asked to refrain from any exercises or exertion for a minimum of 3-6 months as directed by pediatric cardiology. A slow return to play process after clearance is recommended.
Keys to History and Physical Exam
The American Academy of Pediatrics (AAP) continues to recommend that all children and adolescents who test positive for COVID-19 notify the primary care physician, who knows the athlete, prior to return to sports or physical activity.5
Children who are asymptomatic or have mild symptoms (<4 days of fever (>100.40F), and/or <1 week of myalgias, chills, and lethargy) are recommended to have at least a phone call or telemedicine visit with their primary care physician prior to return to sports or physical activity. This phone consultation or telemedicine visit should specifically address questions concerning for any associated cardiovascular symptoms, including but not limited to chest pain, shortness of breath out of proportion for upper respiratory illness, new-onset palpitations, or syncope. If any concerning symptoms are identified, the child/adolescent should be evaluated in person prior to clearance for sports or activities.5
Children or adolescents with moderate symptoms (>4 days of fever (>100.40F), and/or >1 week of myalgias, chills, and lethargy and/or a non-intensive care unit hospital admission, and no evidence of MIS-C), should be evaluated in person by their primary care physician after symptom resolution and appropriate quarantine. The primary care physician should review cardiac symptoms described in the American Heart Association (AHA) 14-point screening evaluation, with emphasis on the cardiac symptoms below, including shortness of breath that is new or out of proportion to prior upper respiratory tract infections5. Any child or adolescent who has had severe COVID-19 symptoms (ICU stay and/or intubation) or MIS-C should be restricted from sports and physical activity for a minimum of 3-6 months and should be evaluated by a cardiologist prior to return to sports or physical activity. This follow-up should be arranged prior to discharge from the hospital.5
MEDICAL HISTORY
Personal History
- Exertional chest pain/discomfort
- Palpitations or abnormal heartbeat
- Exertional syncope or near syncope
- Excessive exertional and unexplained fatigue/fatigue associated with exercise
- Prior recognition of a heart murmur
- Elevated systemic blood pressure
- Prior restriction from participation in sports
- Prior testing for the heart ordered by a physician
Family History
- Premature death – sudden and unexpected for the age of 35 due to heart disease in one or more relatives
- Disability from heart disease in a close relative
- Specific knowledge of certain cardiac conditions in family members, specifically: hypertrophic or dilated cardiomyopathy, long-QT syndrome, or other ion channelopathies, Marfan syndrome, or clinically important arrhythmias
Physical Exam
- Heart murmur – exam supine and standing with Valsalva, specifically to identify murmurs of dynamic left ventricular outflow tract obstruction
- Femoral pulses to exclude aortic stenosis
- Physical stigmata of Marfan syndrome
- Brachial artery blood pressure, sitting, preferrable both arms
If there is any new shortness of breath with exercise or shortness of breath out of proportion to a typical upper respiratory tract infection, dyspnea on exertion, new chest pain, syncope, or palpitations, an ECG or referral to cardiology is recommended.
The physical exam should be comprehensive but focus specifically on the cardiac and pulmonary systems. The cardiac exam should be performed in the supine, standing, and squatting position, specifically listening for new murmurs, abnormal rhythms, or gallops. Any new murmur, gallop, or arrhythmia should be referred to cardiology for clearance.
Any athlete who is experiencing a new-onset exercise intolerance, chest pain with exercise, syncope, or near syncope as they return to sport should be evaluated.
If an athlete has a remote history of COVID-19 and has returned to exercises on their own without issues, a phone call to update the patient’s primary care provider is recommended.
Diagnostics
As mentioned previously, diagnostic testing and imaging depend on severity of the infection, duration of symptoms, and past medical and family history. While primary care physicians may consider ordering an ECG depending on the clinical history and exam, further workup will occur at the discretion of a cardiologist.
The cardiologist will determine further workup and evaluation. This may include ECG, echocardiogram, laboratory evaluation, cardiac MRI, Holter monitory, or exercise stress test depending on the severity of the disease, symptoms, and/or abnormalities found on history, physical, and diagnostic workup. There is no standard workup approach currently for cardiologists in the asymptomatic, mild, or moderate categories; these should be symptoms based.
ECG T-wave inversion to T-wave abnormalities, flattening or other abnormalities in the T-wave, as well, have been seen in the hospitalized patient with MIS-C and reported in the asymptomatic/mild symptom patient population, as well. These abnormalities appear to resolve with time.
Special Considerations: Return to Play Steps
Once an athlete has been diagnosed with COVID-19, it is recommended that they hold off on sports participation and exercise for 10 days after the positive test or symptom onset, and 10 days after symptom resolution without fever-reducing agents. Athletes may begin Phase 1 of the following return-to-play progression once they are able to complete activities of daily living (ie, walking around the house, dressing, daily hygiene tasks, etc.) without worsening of symptoms and have been cleared by a healthcare provider for exercise or sports activities. Over a 7–10-day period, athletes can slowly return into activity adapted from Elliot, et al.6
- Phase 1: At least two sessions of light aerobic activity (up to 70% maximum heart rate) for up to 15 minutes. Sessions should be at least 24 hours apart. Activities may include brisk walking, light jogging or using a stationary bike. No strength training.
- Phase 2: At least one session of aerobic exercise (up to 80% maximum heart rate) for up to 30 minutes. Simple movement activities such as running drills may be added to increase the level of difficulty. No strength training.
- Phase 3: At least one session of exercise (up to 80% maximum heart rate) for up to 45 minutes. May add some simple sport specific activities and strength training to increase the level of difficulty.
- Phase 4: At least two sessions of sport specific training (up to 80% maximum heart rate) for up to 60 minutes. Sessions must be at least 24 hours apart.
- Phase 5: Resume normal training activities and duration for at least one session.
- Phase 6: Return to competition with no restrictions
Prevention
Mitigation strategies should be used throughout practice and competition to decrease the spread of COVID-19 transmission. Appropriate handwashing hygiene, use of individual water bottles, and cleaning procedures should be followed. The AAP currently recommends that all athletes participating in indoor athletics wear a mask. This can reduce the transmission equal to that of outdoor sports. If an athlete is unvaccinated, masks should be worn while not participating actively in sport and while on the sideline if 3 feet of social distancing cannot be maintained.5
The best prevention is the COVID-19 vaccine. The vaccine has been shown to be safe and effective in reducing severe disease and hospitalizations.
The AAP continues to recommend an annual health evaluation performed in the medical home (ie, the primary care physician/provider office). In an ideal world this would incorporate components of the pre-participation evaluation. The frequency of the actual pre-participation evaluation however does fluctuate by state requirement with some states requiring an annual evaluation while other states have recently switched to every two-year requirement for the PPE (preparticipation evaluation) component. The AAP recommends however, physicians and healthcare providers should ask about any COVID-19 prior infection since their last pre-participation and/or annual exam and vaccine status in the pre-participation evaluation5.
SUMMARY
For the 15-year-old male athlete who presented with moderate symptoms, it was recommended he be evaluated in person by his primary care physician once his symptoms resolved and that he finish the recommended quarantine. Upon evaluation by his primary care physician, a review of the 14-point AHA screening evaluation questions and a thorough physical exam were conducted and did not reveal any concerning symptoms. He was instructed to complete a 7-day gradual return-to-play protocol as outlined above.6 He was able to return to football without symptoms.
A CAVEAT
It is important to note that presentation of this case reflects recommended best practices at the time of this publication. Recommendations will continue to evolve quickly, however, as we continue to learn and discover more. As such, recommendations included in this review may change with time.
REFERENCES
- Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265-1273.
- Phelan D, Kim JH, Elliott MD, et al. Screening of potential cardiac involvement in competitive athletes recovering from COVID-19: an expert consensus statement. JACC Cardiovasc Imaging. 2020;13(12):2635-2652.
- Valverde I, Singh Y, Sanchez-de-Toledo J, et al. Acute cardiovascular manifestations in 286 children with multisystem inflammatory syndrome associated with COVID-19 infection in europe. Circulation. 2021;143(1):21-32.
- Clark DE, Parikh A, Dendy JM, et al. COVID-19 Myocardial Pathology Evaluated Through scrEening Cardiac Magnetic Resonance (COMPETE CMR). medRxiv. 2020.
- American Academy of Pediatrics. COVID-19 interim guidance: return to sports and physical activity. Available at: https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/covid-19-interim-guidance-return-to-sports/. Accessed 05/13/2021, 2021.
- Elliott N, Martin R, Heron N, et al. Graduated return to play guidance following COVID-19 infection. Br J Sports Med. 2020;54(19):1174-1175.
Author affiliations: Brian Harvey, DO, Children’s Mercy Kansas City. Natalie Stork, MD, Children’s Mercy Kansas City.
Read Similar Articles
- Conducting Preparticipation Sports Physicals In The Urgent Care Center
- Concussion Care Adds Value To An Urgent Care Sports, Camp, And School Physical Program


