Urgent message: Youth athletic programs are ubiquitous in the United States, with leagues requiring players to have a physical exam before they’re allowed to take part. Ensuring your urgent care center is ready to be a “go to” resource for a thorough work-up increases young athletes’ chances for a safe experience and bolsters your position as a valued community health resource.
INTRODUCTION
Millions of juveniles participate in organized athletics the world over every year. In the United States, preparticipation exams are required, though specific policies and forms vary significantly in various localities. There is controversy, for example, as to whether an EKG or other cardiac testing is necessary. Ultimately, it is usually up to the examiner’s discretion whether a candidate “passes” the exam or not, so it is essential to remain current on recommendations from professional societies and be consistent within your own practice as to what findings warrant further workup.
BACKGROUND
Preparticipation exams began in the 1970s, though early efforts amounted to little more than checking for heart murmurs and inguinal hernias. A collaborative effort among various specialty organizations has given birth to more comprehensive history and physical examination guidelines1 starting in the 1990s, however.
DISCUSSION
Recent Updates
The 2019 iteration of the preparticipation evaluation—a joint effort among the AAFP, AAP, ACSM, AMSSM, AOSSM, and AOASM—includes anticipated medical history elements such as current and past medical conditions, surgical history, medications and supplements (including over-the-counter medicines), and allergies, but also the PHQ-4, a brief screen for psychiatric morbidity. Today’s form differentiates between sex assigned at birth and gender identity. Also, the stratification of the athlete’s outcome (ie, “cleared,” “not cleared,” or “cleared with restriction”) has moved to a medical eligibility form that further breaks down possible outcomes of the evaluation and replaces the concept of “clearance” with “eligibility,” a subtle but important distinction.
General Principles
Preparticipation evaluation forms typically carry a validity period of 1 year. It is recommended these exams be conducted at least 6 weeks prior to the first (preseason) practice to allow time to further evaluate and treat any conditions that may preclude full clearance and participation. Realistically, though, many families will come in hours before the season’s first practice, treating the visit as a formality, rather than an important risk assessment tool.
Evaluations should be performed by licensed, qualified medical professionals (ie, MD, DO, MBBS, NP, PA), though some elements (eg, blood pressure, vision screening) may be performed by other staff members. While the actual location of the assessment (eg, a medical office versus a repurposed gymnasium space) depends on community resources, the athlete should be given at least a modicum of privacy.
Unless otherwise noted, a sports physical/medical eligibility form that deems a candidate “eligible” for sports permits them to engage in any sport, not just the one or ones mentioned at the outset of the encounter. Consequently, it is important to explicitly limit athletes from inappropriate activities, even if they were not mentioned previously. A patient with history of seizures (epilepsy), for instance, should avoid SCUBA diving, or one with hemophilia should avoid boxing and other “collision sports.” Though sports can be classified by physical intensity (static and dynamic components), activities within the same grouping may have dramatically different risks. For example, archery, auto racing, and diving all share the same classification, but the types of injuries a person could suffer in each are quite dissimilar.
The History Form
The young athlete should complete the medical history form—with parental help, if needed—prior to the medical provider’s evaluation. Any “yes” responses to questions should be explored further and explained. Key elements to review include personal history of asthma and/or concussions, use of vision and/or dental correction (eg, eyeglasses, contact lenses, dental braces), and family history of sudden death. Symptoms such as dyspnea, chest pain, and syncope or near-syncope also warrant exploration, as do recent history of mononucleosis (or other illnesses causing splenomegaly and/or hepatomegaly), seizure disorder, sickle cell disease, Marfan syndrome, hemophilia, long QT syndrome, cardiomyopathy, myocarditis/pericarditis, and/or eating disorders. Whether the candidate has participated in previous seasons (and whether they encountered difficulties during it) is also relevant to your assessment. Though it is not usually mentioned explicitly on the sports physical form, recent infection with mononucleosis may also impact upcoming involvement in sport.
Concussions
The number and context of past concussions may impact the athlete’s eligibility for sports. There is significant debate in the medical community about whether recurrent or severe concussions should disqualify athlete. Candidates currently experiencing postconcussive syndrome, however, should not be permitted to return to full play until their symptoms have resolved. Candid conversation with the student’s parents/caregivers is usually beneficial. Though theoretically some student─athletes’ collegiate and athletic future may hinge on high school sports, most caregivers do not want to put their child at undue risk. With the first concussion, you should assess why it happened: Did the athlete make a mistake, did someone else hit them illegally, was the equipment poorly fit, etc.? With the second concussion, you may wish to discuss restriction from particular sports, as three concussions may suggest a pattern of injury that should not be continued.
Catastrophic injury
Because kidney injury from participation in sports is rare, professional society recommendations regarding athletes with a single functioning kidney have been vague, historically, if they existed at all. To be sure, severe brain, spinal cord, and cardiac injury are more common. Surprisingly, cycling and skiing are more likely to result in renal injury than football.2 As such, the routine, seemingly reflexive response of restricting athletes with a single kidney from contact sports is viewed as unnecessary.3,4
The Physical Form
Blood pressure and vision
Vital signs and a vision screen were likely obtained prior to you even seeing the patient. Unfortunately, most forms do not specify cutoffs for abnormal values. Resting blood oxygen saturation should be ≥90% on room air. Though 160/100 mmHg has been mentioned in the literature, this does not take age, gender, or height percentile into account (or, for that matter, the intended sports). Additionally, there is something to be said for those with hypertension needing exercise. As a rule of thumb, candidates with a blood pressure in the 95th percentile per the National Heart, Lung, and Blood Institute’s Blood Pressure Levels for Boys by Age and Height Percentile chart5 should receive further attention.
Neither body mass index (BMI) or body fat percentage are routinely asked on preparticipation evaluation forms.
Satisfactory vision, as tested via a Snellen chart, is necessary to avoid risk of injury to self and others. Again there is some controversy here, as it has been argued that 20/20 vision should be the minimum standard. Practically speaking, though, 20/40 (ie, seeing at 20 feet what a person with “normal” vision can see at 40 feet) may be sufficient for high school athletics and below. When performing the vision screen, it is advisable to have candidates remove their eyeglasses or, if possible, contact lenses. Thus, if they have a satisfactory score, they need not worry about appropriate lenses for sport. If their score is worse than 20/40, replace their vision correction and retest. If they again do not have an appropriate score, they should be referred to an optometrist. If, however, their vision is now satisfactory, you should confirm that their vision correction is appropriate for that sport. For example, wire-frame glasses might be sufficient for bowling or cross-country running, but would not be for swimming or wrestling. High-velocity sports like hockey require a protective face-shield, regardless. This holds true for monocular athletes; they should wear appropriate corrective lenses if their functional eye has an uncorrected visual acuity worse than 20/40. Given their reduced visual field, it would be unwise to allow a monocular athlete to participate in full-contact sports like wrestling, football, boxing, and judo. (One additional comment about the eyes: Do not forget to comment on whether the pupils are equal. Physiological anisocoria in which the pupils are unequal in size between 0.4 and 1 mm is benign. However, certain causes can belie mechanical trauma, infection, neurologic disease, and exposure to toxins. In the context of head trauma on the athletic field, this is likely to precipitate a head CT scan for the affected student. If physiological anisocoria has already been documented, this may avoid unnecessary radiation exposure and cost.)
Visual assessment
Stigmata of Marfan’s syndrome (eg, kyphoscoliosis, pectus excavatum, joint hyperlaxity) and evidence of communicable dermatologic conditions (eg, herpes gladiatorum, tinea corporis) warrant further evaluation. Evidence of eating disorders, injection drug use and/or anabolic steroids, or other substances (eg, odor of tobacco and/or alcohol), though not specifically listed on most evaluation forms, should also be explored.
Auscultation and palpation
The would-be athlete’s examination should include evaluation of all joints (including the neck and back) for deformity, pain, and range of motion; sensation and strength in the extremities; gait; cervical, axillary, and inguinal lymph nodes; heart sounds (specifically murmurs, with repeat auscultation during the Valsalva maneuver); lung sounds and effort; abdomen; and skin. As noted previously, the urogenital exam, once specifically listed for males (ostensibly with the purpose of identifying hernias, but later also used to further evaluate Tanner staging), has been removed from the current iteration, likely to the relief of many adolescent boys.
Murmurs
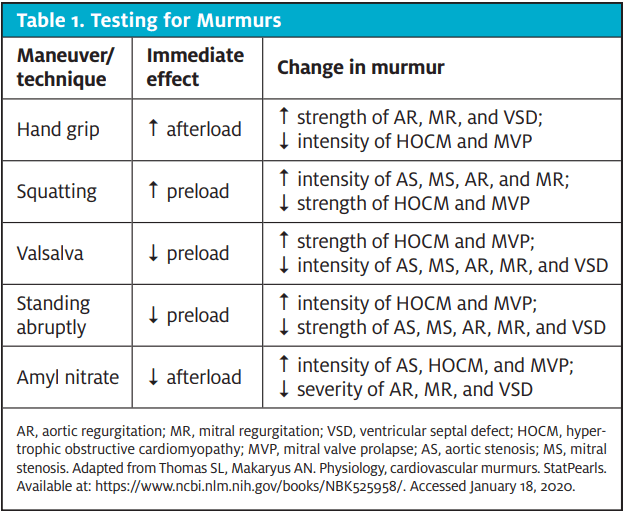
Heart murmurs are very common, and can last through adolescence and into adulthood or resolve over time. Benign cardiac murmurs include systolic ejection murmurs (eg, Stills murmur, innocent pulmonary flow murmur, peripheral pulmonary artery stenosis, and arterial supraclavicular murmur) and benign continuous murmurs (eg, venous hum, mammary souffle). Innocent murmurs tend to be soft, short, and systolic (ie, not holosystolic), and “sweet.” They do not radiate and are not associated with clicks or gallops. Table 1 lists specific testing for murmurs.
Role of the EKG
Electrocardiography, echocardiography, and/or referral to a cardiologist may be considered if abnormalities are uncovered in the patient’s personal or family history and/or physical exam. Though EKGs seem to be the standard of care for similar young athletes in Europe, they have not been shown to be cost-effective for identification of previously unknown conditions during routine screening. In fact, the AAFP specifically advises against cardiac screening tests for asymptomatic, low-risk patients.6
Athletes with disabilities
Discuss with the would-be athlete (as appropriate) and caregivers if there are any conditions that may require special accommodations and/or result in restrictions in participation. As in other contexts, not all disabilities are visible. Autism, cerebral palsy, fetal alcohol syndrome, fragile X syndrome, and spina bifida, for example, all have a wide variety of presentations. Down syndrome and cognitive impairment do not necessarily preclude involvement in sport. Assistive devices and durable medical equipment (eg, hearing aid, removable prosthetic, insulin pump, colostomy bag) should be noted and considered in the context of which sport the child plans to engage in. During the physical examination, providers should look for evidence of spinal cord compression and atlanto-axial instability, which can arise from congenital conditions such as osteogenesis imperfect and Down syndrome, or acquired causes like degenerative changes from rheumatoid arthritis. Other considerations include dietary restrictions (both religious and medical), epilepsy, paralysis (which can lead to difficulties with thermoregulation), hemophilia, and certain mood disorders.
Billing and coding
Some practices charge a flat-fee for preparticipation evaluations and do not bill insurance. If you do use an ICD-10 code, Z02.5 (routine sports physical exam) should be sufficient. In the event that this evaluation is part of a longer well-child exam, the codes Z00.129 and Z00.121 (without and with abnormal findings) may be appropriate, potentially with the additional code Z02.9 (administrative encounter) to indicate work above and beyond the well-child exam.
References
- American Academy of Family Medicine. Preparticipation Physical Evaluation History Form. Available at: https://www.aafp.org/dam/AAFP/documents/patient_care/fitness/ppehistoryform2010.pdf. Accessed April 16, 2020.
- Grinsell MM, et al. Single Kidney and Sports Participation: Perception Versus Reality. Pediatrics. 2006 Sept; 118(3): 1019-27. https://pediatrics.aappublications.org/content/118/3/1019
- Grinsell MM, et al. Sport-Related Kidney Injury Among High School Athletes. Pediatrics. 2012 July; 130(1): e40-5. https://pediatrics.aappublications.org/content/130/1/e40
- (see also https://www.aap.org/en-us/about-the-aap/aap-press-room/pages/Young-Athletes-Unlikely-to-Injure-Kidney-Playing-Contact-Sports.aspx)
- https://www.nhlbi.nih.gov/files/docs/guidelines/child_tbl.pdf.
- Mirabelli MH, et al. The Preparticipation Sports Evaluation. Am Fam Physician. 2015 Sept; 92(5): 371-6. https://www.aafp.org/afp/2015/0901/p371.html.
Additional Resources
Bernhardt DT, Roberts WO. PPE – Preparticipation Physical Evaluation. (5th ed. American Academy of Pediatrics, 2019.
Caswell SV, et al. State-specific differences in school sports preparticipation physical evaluation policies. Pediatrics. 2015;135(1):26-32.
Frank JE, et al. Evaluation and management of heart murmurs in children. Am Fam Physician. 2011;84(7):793-800.
Horn F, et al. An athlete’s eyesight: what you need to know when conducting pre-season vision tests. NATANews. August 2011. Available at: https://www.aoa.org/Documents/optometrists/sports-vision-section-athletes-eyesight.pdf.
Landau DA, et al. Physical examination and ECG screening in relation to echocardiography findings in young health adults. Cardiology. 2008;109(3):202-207.
Lehman PJ, et al. The preparticipation physical evaluation. Ped Ann. 2017;46(3):e85-e92.
Mejia E, et al. Innocent murmur. StatPearls. Available at: https://www.ncbi.nlm.nih.gov/books/NBK507849/. Accessed January 18, 2020.
Mesropyan L, et al. Innocent Heart murmurs from the perspective of the pediatrician. Pediatr Ann. 2016;45(8):e306-e309.
National Federation of State High School Associations. State Association Listing. Available at: https://www.nfhs.org/resources/state-association-listing. Accessed April 16, 2020.
American Academy of Pediatrics. Preparticipation Physical Evaluation (PPE). Available at: https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Pages/PPE.aspx. Accessed December 15, 2019.
Pujalte GGA. Eye injuries in sports. Athletic Therapy Today. 2010;15(5):14-18.
Van der Waal EE. ECG screening in athletes: optional or mandatory? Neth Heart J. 2015;23(7-8): 353-355.
Adapted from the American Academy of Family Physicians’ Practice Management Handbook (2020).
The author would like to thank Kevin Bernstein, MD MMS CAQSM FAAFP, for his thoughtful feedback during the development of this article.

