Published on
Urgent message: Musculoskeletal disorders result in costly, disabling outcomes for Americans—causing significant economic impact (work-related injuries, early retirement, days away from work) and representing a leading cause of chronic diseases nationwide. Frequently, the initial treating facility, which determines if the injured/ill patient is capable of returning to work or needs time away from work or modified duty, is an urgent care center.
Ashley Clay, MSPAS, PA-C
INTRODUCTION
An estimated one in two adults older than 18 years of age, or 126.6 million Americans, are affected by musculoskeletal disorders (MSDs),1 exceeding the percentage of adults with pulmonary and cardiovascular disease.1 In 2012─2014, the United States Bone and Joint Initiative estimated that $322 billion were spent treating MSDs.1 Factors contributing to cost include an aging population, overutilization of diagnostic studies, inappropriate visits to emergency departments, poor understanding of work functions, bodily requirements, and ergonomic design.
OVERVIEW OF MSDs
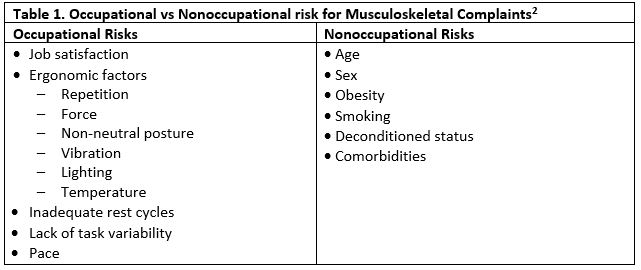
The likelihood of developing musculoskeletal complaints is multifactorial2; see Table 1 for categorization of occupational vs nonoccupational risks.
History and physical examination
The approach to the musculoskeletal exam begins with a detailed history and establishing symptom parameters. These include:
- Location/radiation
- Onset, timing
- Duration
- Aggravating/alleviating factors
- Quality
- Context, mechanism of injury
- Trauma, leisure or work-related, previous injury
- Other associated symptoms
The urgent care provider is responsible for understanding work duties, identifying exposure risk, and determining return-to-work status. Consideration may be given to restrictive duties, such as decreased or temporarily avoiding certain movements, repetitions, awkward postures, and enforcing weight limits; however, lost time for certain conditions may be unavoidable. Maintaining functional capacity and limiting muscle loss is paramount for the patient and practitioner.
After an appropriate history, the physical examination consists of a stepwise approach:
- Inspection (comparing contralateral side)
- Erythema
- Edema
- Previous surgical scarring
- Discoloration
- Bruising
- Muscle atrophy, tone
- Symmetry
- Palpation
- Crepitus
- Tenderness
- Warmth
- Range of motion (ROM)
- Active and passive
- Neurological testing
- Sensory
- Reflexes
- Strength assessment
- Peripheral pulses
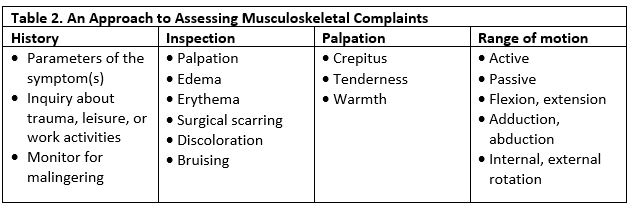
Clinical tests specific to the suspected diagnosis may also be required.3 All red flag symptomology should be ruled out and any signs of malingering documented. Secondary gain concerns may be involved with a reported work-related injury, and a detailed description of job duties is warranted. If the urgent care provider is encountering reported work-related injuries frequently, it may be helpful to tour the job site in order to better understand the working environment and accommodation process.
Repetitive motion injuries commonly seen in the urgent care setting include:
- Rotator cuff tendinopathy
- Carpal tunnel syndrome
- de Quervain tendinopathy
- Lateral and medial epicondylitis
- Trigger finger or thumb
ROTATOR CUFF TENDINOPATHY
Overview
Rotator cuff (RC) tendinopathy results in painful motion associated with inflammation and friction of muscles, tendons, and bursa related to multiple causes. RC tendinopathy falls into the spectrum of shoulder impingement syndrome.3 The RC is primarily responsible for internal/external rotation, shoulder abduction, and stabilization—composed of four muscles (the supraspinatus, infraspinatus, teres minor, and subscapularis) and corresponding musculotendinous attachments. Shoulder pain is a common presenting complaint in the urgent care setting, estimated to account for 16% to 34% of complaints with rotator cuff pathology as the most common reason patients seek treatment.4
Stress to the rotator cuff, specifically the supraspinatus muscle, occurs when the arm is in an elevated position.
History/Clinical Presentation
- Complaints of pain with overhead activities
- Lateral deltoid area
- Daily activities such as putting on a shirt or brushing hair cause pain
- Vocational vs recreational history involving repetitive shoulder motion or working with hands over head
- Difficulty sleeping, more pronounced when lying on affected side
- Pain is gradual, nonradiating, and exacerbated by external rotation and elevation
Physical examination
- Tenderness of the supraspinatus, infraspinatus, and subacromial aspect
- Supraspinatus tendon—most frequently injured
- Crepitus (grating, cracking sound)
- Atrophy of supraspinatus and infraspinatus muscle
- Indicates longstanding disease
- Sunken appearance of scapular fossa
Testing
Exclusion of other etiologies (cervical spine issues, acute coronary ischemia, osteoarthritis) is important. Rotator cuff tendinitis is clinically diagnosed; many consider musculoskeletal ultrasound as the gold standard for initial evaluation of tendon disorders5; however, this is not routinely completed in the urgent care setting. Physical exam signs suggestive of rotator cuff pathology include:
- Painful arc test—Shoulder pain between 60o and 120o abduction
- Most useful when used in conjunction with Neer and Hawkins-Kennedy testing
- Neer—Pronate, passively forward flex affected arm
- Pain is a positive result
- Hawkins-Kennedy—Elevate the arm, flex shoulder and elbow to 90o and internally rotate
- Pain is a positive result3
- “Empty can” test—Straighten arm, 90o of abduction and 30o forward flexion, internally rotate
- Relative isolation of the supraspinatus tendon
- Many consider this the “gold standard” for evaluation of supraspinatus function
- Clinician then attempts to adduct arm against resistance
- Tendinopathy—pain without weakness
- Tear—pain with weakness
- Lidocaine injection test—distinguishes between tendinopathy and tear
- More accurate assessment of strength
- Tendinopathy—normal strength
- Tear—weakness
- More accurate assessment of strength
Diagnosis
Obtaining radiographs of the shoulders for nontraumatic shoulder pain is generally not warranted and provides little diagnostic benefit.6 Overutilization of x-rays is common; a chart review of 312 patients presenting to the ED with complaints of shoulder pain found that only 20% of the 185 patients for whom x-rays were ordered had a condition resulting in specific treatment; 0% of x-rays in patients in the absence of a fall or deformity provided diagnostic benefit resulting in treatment.7
MRI is recommended after failure of conservative measures or when suspicious for an RC tear. Electromyography (EMG) and nerve conduction velocity studies (NCVs) may be useful to rule out neurological involvement.
Treatment
RC tendinopathy is initially treated with conservative measures for 3-6 weeks:
- Patient education
- ROM exercises to prevent adhesive capsulitis
- Diabetes increases the risk of adhesive capsulitis
- Avoid aggravating activities (work restrictions may be of value)
- Work restrictions: Avoid prolonged, repetitive tasks requiring shoulder abduction, flexion especially above 60o (commonly written as “no overhead work”); avoid heavy lifting and vibration exposure
- In order to facilitate recovery, ergonomic redesign of the workplace may be recommended to employer, focusing on force, shoulder flexion, duration, and posturing
- Support return-to-work and daily activities within limitations of pain
- Based on ROM, strength, and function
- Prior to resuming full duty status, the patient should be able to perform work-activities without return or exacerbation of symptoms
- Physical therapy
- An exercise approach for the treatment of RC tendinopathy has been found to have the same patient outcomes as surgical intervention, even in the presence of partial and full-thickness RC tears3
- OTC NSAIDs for 7-10 days
- Self-application of ice or heat
- Ice believed to reduce acute inflammation
- Heat believed to accelerate healing by way of increased blood supply
- Follow-up appointment scheduled 1-2 weeks after initial assessment
- Assess work limitations and adjustments to activity modifications
- Subacromial glucocorticosteroid injection
- Considered if more conservative approaches (including PT) fail after several weeks
- Initially, a single injection is scheduled; if adequate response, a second should be attempted after waiting at least 2 weeks
- Lateral vs posterior approach
- Lateral approach significantly reduces risk of injecting into RC tendons
- Locate lateral edge of acromion; entry point of needle is 1 to 1.5 inches below
- Needle inserted parallel to acromial angle
- Depth dependent on body habitus of patient
- Inject local anesthetic
- Deltoid muscle (1 mL)
- Deep deltoid fascia (0.5 mL)
- “Popping” sensation appreciated = in appropriate place (subacromial bursa)
- 1 to 2 mL of anesthetic
- Needle left inserted
- Retest strength; if the following conditions are met, inject shoulder with 1 mL methylprednisolone (Depo Medrol) (80 mg/mL)
- 50% reduction in pain
- 75%-80% strength (abduction, external rotation) is 75%-80% of unaffected side
- Absent any “red flag” symptoms or actual diagnosis of an RC tear (in which case referral should be made earlier), refer to orthopedist after 6-9 months of conservative treatment or if suspicion of RC tear
- Retest strength; if the following conditions are met, inject shoulder with 1 mL methylprednisolone (Depo Medrol) (80 mg/mL)
- Needle left inserted
- ROM exercises to prevent adhesive capsulitis
CARPAL TUNNEL SYNDROME (CTS)
Overview
CTS may be acute or idiopathic in nature, resulting from compression of the median nerve causing pain and numbness in the hand. The median nerve passes through the carpal tunnel (formed by the carpal bones and the flexor retinaculum).
Characteristics of CTS include:
- Female predominance
- Personal medical factors increase risk of development3
- Diabetes
- Obesity
- Pregnancy
- Hypothyroidism
- Rheumatoid arthritis
- Anatomic
In addition to personal risk factors, repetition, vibration, awkward postures, forceful exertion, dominant hand overuse, and prolonged task duration are suspected contributing factors.3
Figure 1. Carpal tunnel syndrome
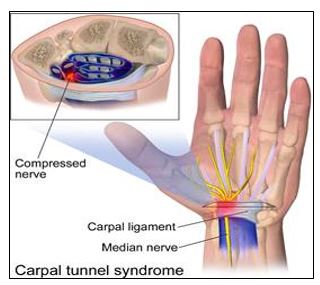
Source: WikiJournal of Medicine. Medical Gallery of Blausen Medical 2014.
History/Clinical Presentation
Pain and numbness occur along the distribution of the median nerve:
- Thumb
- Index and middle fingers
Radial aspect of fourth finger
- Complaints progress over time
- Frequently dropping items
- Weakness, decreased dexterity, and tingling/numbness in the wrist and palm
- Report feeling the need to “shake out” hands to alleviate symptoms
- Difficulty with sustained grasping (eg, holding a steering wheel)
- Often with increased symptoms while in bed
Physical examination
- Strength: Weakness with thumb opposition and abduction may be appreciated
- Muscle Loss: Thenar atrophy may be present in long-standing cases
- Sensory: Fixed sensory loss over the median nerve distribution (not appreciated over the thenar eminence) is another late characterization3
Testing
- Tinel’s sign (percussing lightly over the median nerve)
- Phalen’s test (request the patient hold the dorsal aspect of their flexed wrists together for 60 seconds)
- These are considered positive if a tingling sensation occurs along the distribution of the median nerve
- Phalen’s has both greater sensitivity and specificity than Tinel’s sign3
- Other pertinent clinical testing include:
- Monofilament, vibration, hand elevation test, and carpal compression
Electrodiagnostic tests help confirm the diagnosis; however, electromyography (EMG) is only indicated to rule out other pathology or determination of severity when contemplating surgical intervention. Patients with high clinical suspicion for CTS can undergo injections without having an EMG/NCS completed.
Diagnosis
CTS is a clinical diagnosis, highly suspicious when signs and symptoms are present over the median nerve with characteristic factors providing diagnostic value. If a patient presents with classic symptoms of CTS, confirmed by nerve conduction studies (NCS) and does not wish to undergo surgical decompression, EMG is not warranted or needed for diagnosis.
Treatment
Nonsurgical treatment may provide relief.
- Activity modification and exercise8
- Work restrictions: Not always warranted, consider avoid high force combined with repetitive gripping or pinching and handheld tools that vibrate
- Night splinting8
- Oral corticosteroids3
- For patients who do not want to undergo injection therapy
- Dosing recommendations vary, consider prednisolone 20mg daily for 10 to 14 days8
- Studies note short-term benefit
- Corticosteroid injections3
- Superior to oral forms
- Used if unresponsive to nocturnal splinting with symptoms lasting > than 3 weeks
- Technique: A minimum dose of methylprednisolone 40mg using a 25 or 27-gauge needle at a 45o angle entering the skin near the distal crease8
- No more than once every 6 months per wrist
- Recurrent symptoms after two injections warrant additional adjunct treatment or surgical evaluation
- Lidocaine patches
- Recommended for select cases of acute, subacute and chronic CTS8
- Phonophoresis (ultrasound utilized to deliver topical medications, glucocorticosteroids or NSAIDs via electrical current)8
- Splints and/or injection are generally attempted first as those are believed to provide greater relief8
- NSAIDs
- Not as primary treatment unless thought to have an inflammatory component8
Surgical intervention is considered if nonoperative measures fail; temporary relief following an injection represents a favorable prognostic factor in terms of surgical outcome.
Treatments not recommended include:
- Gabapentin
- Opioids
- Magnets
- Pulsed magnetic field therapy
- Acupuncture
de QUERVAIN TENDINOPATHY
Overview
de Quervain tendinopathy is a noninflammatory thickening of the extensor retinaculum, resulting in tendon entrapment of the abductor pollicis longus and extensor pollicis brevis (housed in the first dorsal compartment). As the overlying retinaculum thickens, pain develops over the radial aspect of the wrist.9 It is a common condition, affecting 1.3% of women and 0.5% of men worldwide.10 The etiology is not well-understood; however, suggestive causative factors include:
- Repetitive motion (overuse)
- Awkward postures (thumb held in extension and abduction)
- Postpartum period
- Diabetes
- Advanced age
- Increased BMI9
Figure 2. de Quervain tendinopathy
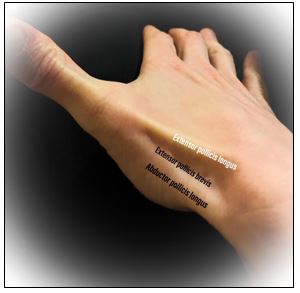
Source: Ashley Clay, MS, PA-C. Used with permission.
History/Clinical Presentation
Gradual onset of pain over the radial styloid.
- Atraumatic history
- Difficulty with gripping objects
- Common in mothers of infants
- Thought to be related to repetitive lifting of the baby9
Physical examination
- Radial sided wrist pain/pain at base of thumb with wrist or thumb motion
- Exacerbated by resisted radial deviation, grasping or gripping
- Tenderness with/without swelling over the first dorsal compartment
Testing
Radiographs do not improve clinical diagnosis but can assist in ruling out other suspected pathology.9
Diagnosis
A classic diagnostic maneuver, Finkelstein’s test, is considered positive if pain is reproduced when the patient has thumb flexed, fingers wrapped around it and the examiner deviates the hand towards the ulna.9
Treatment
- Rest
- Ice
- NSAIDs
- Splinting (thumb spica)
- Follow-up visits are generally required every 1-2 weeks
- Allows determination of treatment benefit vs relief of symptoms
- Work restrictions may require restricted lifting, gripping, and twisting of affected hand; can also consider limiting repetitive wrist flexion and ulnar deviation
- Ergonomic recommendations provided to employer may include identification of localized pressure from sharp objects and forceful use of digits
Refractory cases may require an injection of corticosteroid into the sheath of the first dorsal compartment to reduce tendon thickening, inflammation.9 Researchers continually advocate for conservative approaches. Earp, et al demonstrated that a single injection abated symptoms in 82% of participants at 6 weeks, and 52% were estimated to remain symptom-free at 6 and 12 months postinjection.10 If injection therapy fails, surgical release of the first dorsal compartment relieves the entrapment; this intervention is completed on an outpatient basis9.
LATERAL/MEDIAL EPICONDYLITIS
Overview
The term epicondylitis is a misnomer by name as it suggests “inflammation” of either the medial or lateral aspects of the elbow; however, microscopic analysis of the tendon does not reveal inflammation. Epicondylitis, an overuse condition, is a constellation of micro-tears, collagen distortion, and angiofibroblastic degeneration11 resulting in tendinosis.
- Annually affects 1%-3% of the population11
- Women and men are affected equally
- Average onset between the ages of 40 and 60 years11
- Lateral epicondylitis—Injury to the extensor carpi radialis brevis muscle (ECRB)
- Effects wrist extension
- Referred to as “tennis elbow”
- Medial epiconylitis—Injury to the pronator teres and flexor carpi radialis muscles
- Effects wrist flexion
- Referred to as “golfers’ elbow”
History/Clinical Presentation
Patients will likely present with pain around the lateral or medial aspects of the epicondyle (dominant hand) and subjective complaints with gripping activities. Causative factors include:
- Forceful use (managing loads greater than 44 pounds)
- Repetition, especially for greater than 2 hours per day11
- Smoking
- Obesity
Physical examination
- Tenderness along respective epicondyle
- 1─2 cm distal to ECRB
- Pain is commonly elicited with resisted pronation of the forearm12
- Lateral epicondylitis—Pain with wrist extension
- Medial epicondylitis—Pain with wrist flexion
- Full ROM
- Rarely associated numbness or tingling
- Suggests additional ulnar or radial neuropathy
- 1─2 cm distal to ECRB
Testing
Diagnostic studies are rarely warranted or useful during the initial workup; however, if complaints persist following 4 weeks of treatment, plain radiographs should be considered; if there is concern for C-6 radiculopathy, MRI may be of value. It should be noted that ultrasound can be employed to characterize the areas of tendinosis and may assist in treatment modalities.11
Diagnosis
Typically clinical and based on history and physical examination findings.
Treatment
Treatment recommendations are similar for both medial and lateral presentations. The cornerstone of therapy includes:
- Rest, ice, compression, elevation (RICE therapy)
- Work restrictions: Avoid vibrating hand tools, high-force gripping or pinching13
- As this is not a progressively worsening condition, no basis for permanent restrictive duty
- NSAIDs
- Oral vs topical
- Tylenol
- Counterforce bracing—circumferential forearm band
- Applied 10 cm distal to elbow joint11
- Stretching, strengthening12
- A 2012 study of 297 patients found that structured physical therapy provided greater pain relief than corticosteroid injections or NSAIDs
- Patients treated with PT also found to have lower recurrence rate11
- Corticosteroid injection
- Provides acute relief; however, long-term outcomes remain unchanged for both conditions11,12
TRIGGER FINGER/THUMB
Overview
Entrapment (thickening, stenosis) of the flexor tendons at the level of the A1 pulley system results in trigger finger (TF).
- One of the most common upper limb issues evaluated in orthopedic practice14
- Occurs 20 times more often than de Quervain’s10
- Female predominance
- More common between the ages of 52 and 6214
- Associated with
- Diabetes
- Connective tissue disorders
- Nontraumatic events
- Occupations with repetitive tasks requiring force and grip; exposure to vibration
History/Clinical Presentation
This condition results in the finger or thumb feeling “stuck” or causing a sensation of “catching” during flexion (bending) or extension (straightening) of the digit.12 Initially, patients complain of joint stiffness or pain over the palmar aspect radiating along the digit.
Physical examination
- Palpable snapping sensation or crepitus over the A1 pulley system (overlying the MCP joint) with associated tenderness
- Nodule may be present distal to the metacarpophalangeal (MCP) joint14
- Puckering of the skin is common
- Thickening of palmar fascia decreases ROM
Testing
No routine lab or imaging tests are required if other diagnoses have been ruled out. X-rays can be utilized if there is concern for joint abnormalities or inflammatory arthritis exists, but are not required if presentation supports a clinical diagnosis.
Diagnosis
Clinically diagnosed, locking or clicking observed as patient opens and closes hand.
Treatment
- Corticosteroid injection into the tendon sheath
- First-line treatment
- Injections are reported to be 64%-93% successful in nondiabetic patients15
- Surgical intervention is generally considered after failing two or three injections
- Ice
- NSAIDs
- Splinting
- Often affects dexterity and mobility, resulting in noncompliance
- Shown to resolve in 55% of manual labor population if splinted early16
- Work restrictions: Avoid repetitive activities that aggravate complaints; consider padded gloves
URGENT CARE IMPACT
Responsibilities of the urgent care provider often encompass occupational health roles, especially in rural areas, as preferred provider networks within Worker’s Compensation are limited; urgent care clinicians provide initial medical management for musculoskeletal complaints and reported work-related injuries.
Appropriate referrals to specialists, coordination of care, determination of work-relatedness, and management of the return-to-work (RTW) process are aspects of these visits. Utilization of ambulatory centers for the treatment of MSDs (work and non─work-related) continue to increase; according to the Bone and Joint Initiative, 85% of individuals with MSDs will have at least one ambulatory care visit annually, averaging slightly below six office visits per year.17
As the population ages, it is reasonable to expect an increase in healthcare utilization for MSDs. The U.S. Census Bureau projects that by the year 2060, one-quarter of the population will be 65 years and over (nearly doubling in size from 2017 to 2060).18 Efficient, cost-effective management of MSDs is well within the field of expertise for urgent care providers.
A 12-month retrospective review of 12,722 patients treated at a physician-owned urgent care facility specializing in orthopedics found that access to care for ambulatory conditions in an urgent care setting improved patient care and decreased overall health costs for the patients and the facility. The average wait time to be seen by a provider was 17 minutes at the UC, compared with 45 minutes in the hospital ED; time to follow-up with an orthopedist was 1.2 days post UC compared with 3.4 days post ED; overall cost per visit was $461 (UC) and $8,150 (ED).19
Work-Related Musculoskeletal Disorders
Clinicians can incorporate basic screening tools with a detailed understanding of workplace responsibilities to establish causation and potential need for work restrictions. Occupational history should include:
- Job satisfaction
- Employment length
- Rotation schedule
- Reported cause
- Job description
- Subjective employee description
- Employer-provided description vs job site survey
- Occupational risk factors, exposure duration
- Exertional demands
According to the American College of Occupational and Environmental Medicine (ACOEM), medical causation refers to a causal link between an injury, illness, disease, or disorder and a known risk factor.20 MSDs can be attributed to both work and non─work-related activities. Work relation is suspected when an event or exposure during work results in a bodily reaction.
MSDs are considered work-related musculoskeletal disorders (WMSD) if the following conditions are met: 1) The work environment and work duties contributed significantly to the disease and/or 2) the injury or illness is exacerbated or persists longer, secondary to work conditions.
Nearly one-third of injuries and illnesses reported in 2017 resulted in days away from work.21 Major events resulting in injuries included:21
- Bodily reaction
- Sprains, strains, tears
- Overexertion
- Pushing, pulling, lifting, carrying
The U.S. Bureau of Labor Statistics (BLS) reported that approximately 2.8 million nonfatal workplace injuries and illnesses occurred in 2017, at a rate of 2.8 cases per 100 full-time employees.21 Of those cases, tendinitis resulted in 33 median days away from work; carpal tunnel syndrome resulted in 30; and sprains/strains/tears accounting for 11 median days.21
In addition to having familiarity with epidemiological evidence supporting direct correlation with accepted risk factors,18 the urgent care clinician must fully understand the work environment and duties. MSDs are associated with high costs to employers secondary to absenteeism, lost productivity, increased healthcare premiums, disability, and workers’ compensation.
Determining Work Relationship
Urgent care providers may need to determine work-relatedness based on presenting symptoms and work exposure—causation of MSDs is not always easily identified and nonacute subjective symptoms can progressively worsen and manifest as a multifactorial consequence. Often, cause-effect relationships between clinical diagnosis and occupational exposure are difficult to ascertain.
The initial assessment of a reported work injury often occurs at the urgent care level; causality findings during initial evaluation are often preliminary, and the provider should communicate the level of uncertainty to the patient, employer, and workers’ compensation.20 Objectives during the initial evaluation include:21
- Determine diagnosis
- Accounting for subjective complaints, clinical signs, and objective diagnostic findings
- Review previous medical records
- Including pre-existing symptoms, diagnoses, previous injury or trauma
- Results of medical surveillance and preplacement testing
- Consideration of other contributing factors
- Document any signs of malingering or concerns for secondary gain
- Workplace exposure (as detailed above)
- Data review
- Supports or refutes an occupational relationship
- Literature, studies, case reports
- Supports or refutes an occupational relationship
Determining causation should account for occupational/nonoccupational risk, socioeconomic, and psychological factors.20 Causation must be evidenced-based.
Incorrectly correlating the injury to the occupation or failing to associate job hazards with reported complaints may negatively impact multiple stakeholders, including worker compensation carriers, employers, personal health insurance companies, and the employee.
Figure 3. Number of Americans with MSDs by Age, United States, 1996–1998 and 2012–2014
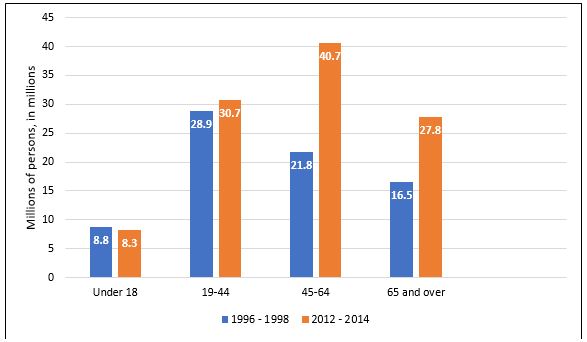
Adapted from: Medical Expenditures Panel Survey (MEPS). Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services, 1996–2014.
Returning to Work/Modified Duty vs Lost Time
The initial treating facility—often an urgent care center—determines if the injured/ill patient is capable of returning to work, requires time away from work, or may return with restricted/modified duties. The American Medical Association strongly recommends that providers return patients to their usual duties as soon as possible. Strong evidence links positive benefits of mental and physical health to re-employment. The longer an injured worker is placed off work, the more likely they will remain off work.
Navigating the RTW process requires that the clinician understand tolerance, capacity, associated risks, work environment, and bodily requirements of a full return to duty. Assess if the employer accommodates modified duty status; many have progressive, robust RTW programs. The ACOEM offers guidance in terms of anticipated functional status based on a variety of MSDs; see Table 3.
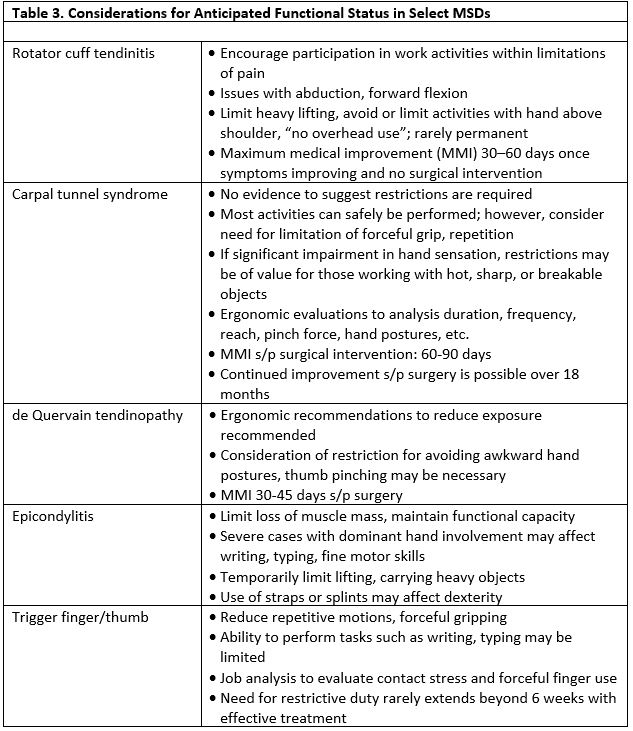
Adapted from the American College of Occupational and Environmental Medicine.
CONCLUSION
The ever-changing medical climate requires the urgent care provider be cognizant of economic impact and implications of cost burden and care. MSDs are costly, potentially disabling diagnoses requiring complex diagnostic and therapeutic approaches that encompass facilitation of care, understanding dynamic work environments, promoting total health, and improved functional status for work and non─work-related conditions.
Citation: Clay A. Repetitive motion injuries: urgent diagnosis, patient-centered management. J Urgent Care Med. July 2019. Available at: https://www.jucm.com/repetitive-motion-injuries-urgent-diagnosis-patient-centered-management/.
References
- Weinstein S, Yelin E. Musculoskeletal Diseases. The Burden of Musculoskeletal Diseases in the United States, Fourth Edition. Available at: https://boneandjointburden.org/fourth-edition/viiia0/definitions. 2019. Accessed March 20, 2019.
- da Costa BR, Vieira E. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind Med. 2010;53(3):285-323.
- Karnath, B. Common musculoskeletal problems of the upper extremity. Hosp Physician. 2003;48-52.
- McFarland EG. Examination of the Shoulder: The Complete Guide. Kim TK, Park HB, Rassi GE, et al (Eds). ; New York, NY: Thieme Medical Publishers; 2006:142.
- Lewis J, McCreesh K, Roy JS, Ginn K. Rotator cuff tendinopathy: navigating the diagnosis-management conundrum. J Orthop Sports Phys Ther. 2015;45(11):923-937.
- Broadhurst N, Simmons, N. Musculoskeletal ultrasound—used to best advantage. Aust Fam Physician. 2007;36(6):430-432.
- Fraenkel L, Lavalley M, Felson D. The use of radiographs to evaluate shoulder pain in the ED. Am J Emerg Med. 1998;16(6):560-563.
- Hegmann KT, ed. Hand, wrist and forearm disorders: carpal tunnel syndrome, treatment recommendations. American College of Occupational and Environmental Medicine (ACOEM) Practice Guidelines. 11 Jul. 2018. Reed Group, Ltd. 15 May 2019.
- Earp B, Han C, Floyd E, et al. de Quervain tendinopathy: survivorship and prognostic indicators of recurrence following a single corticosteroid injection. J Hand Surg Am. 2015;40(6):1161–1165.
- Meals RA. de Quervain Tenosynovitis. Medscape. 2018. Available at: https://emedicine.medscape.com/article/1243387-overview. Accessed on March 11, 2019.
- Walrod B. Lateral epicondylitis. Medscape. 2018. Available at: https://emedicine.com/article/96969. Accessed March 18, 2019.
- Young C. Medial epicondylitis. Medscape. 2019. Availablet at: https://emedicine.com/article/97217. Accessed March 18, 2019.
- Hegmann KT, ed. Elbow disorders: diagnosis and treatment recommendations, lateral epicondylalgia and medial epicondylalgia. American College of Occupational and Environmental Medicine (ACOEM) Practice Guidelines. 23 Aug. 2018. Reed Group, Ltd. 23 Oct. 2018.
- Kale S, Gellmanm H. Medscape. Available at: https://emedicine.com/article/1244693. Accessed March 11, 2019.
- Murphy D, Failia JM, Koniuch MP. Steroid versus placebo injection for trigger finger. J Hand 1995;20(4):628:631.
- Rodgers JA, McCarthy JA, Tiedeman JJ. Functional distal interphalangeal joint splinting for trigger finger in laborers: a review and cadaver investigation. Orthopedics. 1998;21(3):305-309.
- United States Bone and Joint Initiative: The Burden of Musculoskeletal Diseases in the United States (BMUS), Fourth Edition, forthcoming. Rosemont, IL. Available at http://www.boneandjointburden.org. Accessed on 15 March 2019.
- Vespsa J, Armstrong D, Medina L. Demographic turning points for the United States: population projections for 2020 to 2060. Current Population Reports. 2018. Available at: https://www.census.gov/content/dam/Census/library/publications/2018/demo/P25_1144.pdf. Accessed June 18, 2019.
- Anderson T, Althausen P. The role of dedicated musculoskeletal urgent care centers in reducing cost and improving access to orthopaedic care. J Orthop Trauma. 2016;30:Suppl S3-S6.
- Greaves W, Das R, McKenzie J, et al. Work-relatedness. American College of Occupational and Environmental Medicine. 2018;60(12):640-646.
- Bureau of Labor Statistics. 2018. Employer-Reported Workplace Injuries and Illnesses – 2017. Available at: http://www.bls.gove/news.release/pdf/osh.pdf. Accessed June 18, 2019.
Ashley Clay, MSPAS, PA-C is an Occupational Health and Wellness Clinic Coordinator and Certified Physician Assistant working at Medcor, Inc. providing occupational health and wellness services to a manufacturing facility located in Huntington, WV. She is also a Certified Ergonomic Assessment Specialist III providing insight on ergonomic risk and cost-effective solutions for a variety of workplace settings. The author has no relevant financial relationships with any commercial interests.

