Urgent message: Septic arthritis can lead to significant morbidity if not treated in a timely manner. Bacteria within the synovial space can lead to rapid joint destruction and irreversible loss of function. When patients present to the urgent care center with a red, hot, swollen, painful joint, every attempt must be made to rule out this disease entity to prevent significant morbidity and mortality.
Introduction
Patients frequently present to urgent care with a red, swollen, and painful joint in the absence of trauma. Causes of acute monoarticular arthritis can range from gout to septic arthritis. Because septic arthritis can result in significant morbidity and up to an 18% mortality, it is important to exclude this diagnosis as rapidly as possible so that definitive treatment can be instituted as soon as possible. Special consideration should be given to patients with prosthetic joints, as these infections can be especially challenging. Obtaining joint fluid by aspiration and then analysis in the lab is essential to the proper diagnosis and treatment.
Case Presentation
 An 84-year-old male presents to the urgent care center with a chief complaint of right wrist pain, redness, and swelling for 1 day. The patient noted tingling in the area before the swelling and redness developed. He denies injury, previous similar symptoms, inflammatory arthritis, or a history of gout. He had no fever, chills, or systemic symptoms. The patient had hydrocodone at home from a previous surgery, but did not think to take it.
An 84-year-old male presents to the urgent care center with a chief complaint of right wrist pain, redness, and swelling for 1 day. The patient noted tingling in the area before the swelling and redness developed. He denies injury, previous similar symptoms, inflammatory arthritis, or a history of gout. He had no fever, chills, or systemic symptoms. The patient had hydrocodone at home from a previous surgery, but did not think to take it.
Past medical history was significant for an abdominal aortic aneurysm repair 4-5 months ago and peptic ulcer disease in the remote past. He did admit to being diabetic. He could not recall his medications.
He was a daily smoker, denied alcohol, and lived at home with aide service. Review of symptoms was negative except as noted above.
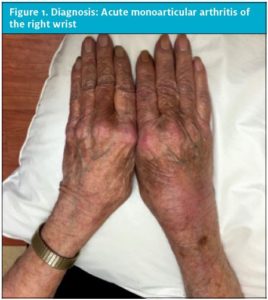
On exam, he was healthy appearing, afebrile, and had a normal pulse and blood pressure. His right wrist was red and swollen. A joint effusion was present. It was diffusely tender. Any movement in any plane caused severe pain. There was normal sensation and capillary refill at the fingers. The remainder of the exam was normal. See Figure 1 for a photo of the wrist.
- Axiom 1: An acute hot, swollen, and tender joint with restriction of movement is bacterial septic arthritis until proven otherwise.1
- Axiom 2: If a diagnosis of septic arthritis cannot be reliably excluded after clinical evaluation, including arthrocentesis, transfer the patient to the emergency department.1
- Axiom 3: Identifying crystals in joint fluid does not rule out simultaneous septic arthritis.2
Discussion
As urgent care clinicians, we should first think about the worst-case scenario; only when that has been ruled out can a more benign diagnosis be considered. In the case of the “red-hot joint,” the most serious threat is septic arthritis.
An adequate history and physical should be conducted, with the goal of determining if the pain is arising from the joint itself or from an adjacent structure such as bursa, tendon, ligament, bone, or muscle, or if it is referred from a visceral organ or nerve root. For example, hip pain can arise from lumbar disc disease or lumbar stenosis.
Conversely, hip joint pain can refer to the buttocks or groin.3 Bursitis, especially in the elbow and hip, may easily be mistaken for septic arthritis and should be excluded by physical exam.
Other useful information includes onset, duration, temporal pattern, number of joints, symmetry of involvement, and extra-articular manifestations. A history of previous damage to a joint by either arthritis or trauma may predispose to septic arthritis. It should be noted that recent joint surgery or an overlying cellulitis are the only findings on history and physical that can significantly increase the probability of septic arthritis.4
Determine the onset of pain, history of trauma, previous joint diseases such as gout or arthritis, medications taken, fever, chills, home treatments, past medical history (especially diabetes), and a past surgical history regarding the joint, or joint replacement. Although elements of the history cannot reliably rule out infectious causes, they may make them less likely. For example, if the patient has a previous history of gout, this diagnosis becomes more likely. Acute symptoms can develop in hours to days. More chronic conditions develop over weeks to months.
On physical exam, inspection should compare one side of the body to the other, specifically looking for symmetry, swelling, and redness. The joint is usually held in the position that allows the maximal intraarticular space. Palpate for swelling, warmth, effusion, and tenderness, distinguishing between bony and soft tissue. Assess range of motion, crepitus, and compare with the unaffected side. Assess for instability. If possible or applicable, observe the patient walking.
Signs of inflammatory joint disease include synovial hypertrophy, joint effusions, pain with motion, particularly at extremes, erythema and warmth, limited range of motion, and joint tenderness. Limited range of motion can result from a tense effusion, a markedly thickened synovium, adhesions, capsular fibrosis, or simply pain. Joint tenderness is not specific for any one type of acute arthritis.
Differential Diagnosis
Fortunately, the differential diagnosis of acute nontraumatic inflammatory monoarthritis is relatively short (Table 1). This includes septic arthritis, gonococcal arthritis, gout and pseudogout, and systemic rheumatic disease manifesting in only one joint, such as RA, and Lyme arthritis. The rheumatologic diseases are generally polyarticular, but can present singly. Gonococcal arthritis is also frequently polyarticular. All can include redness, warmth, acute onset, and pain on movement. The pain is present at rest and with motion, but generally worse at the beginning of the motion than at the end. In advanced or severe cases, any motion of the joint is prohibited by severe pain. An onset within hours should raise the suspicion of joint sepsis.5 Although patients may appear toxic, vital signs, including temperature, are usually normal.5
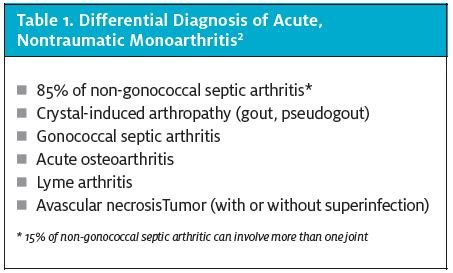
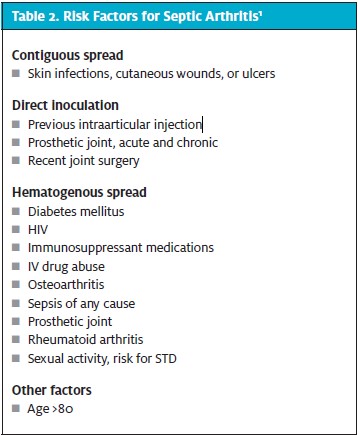
Before the advent of antibiotics, two-thirds of patients with septic arthritis died. The incidence of septic arthritis is variable and can range from 4‒29 cases/100,000 patient years. The most common bacteria responsible is Staphylococcal species, and arises from hematogenous spread during bacteremia of any cause. Streptococcus may also be responsible. Spread can also be from direct inoculation during an injection into the joint. Eighty-four percent of adults who develop septic arthritis have an underlying chronic medical condition, and 59% will have a previous joint disorder in the affected joint. Patients on immunosuppressant therapy (but, oddly, not immune modulators) have a fourfold increased risk of septic arthritis.6 Risk factors for septic arthritis are listed in Table 2.
In native joints, the knee is the most common site of infection, followed by the hip, shoulder, ankle, elbow, and wrist.2 Other joints, including the axial spine and costochondral joints can also be affected, and are more common in intravenous drug abusers. Septic arthritis can coexist with crystal arthropathy, making diagnosis even more difficult. Identifying crystals in joint fluid does not rule out septic arthritis.2
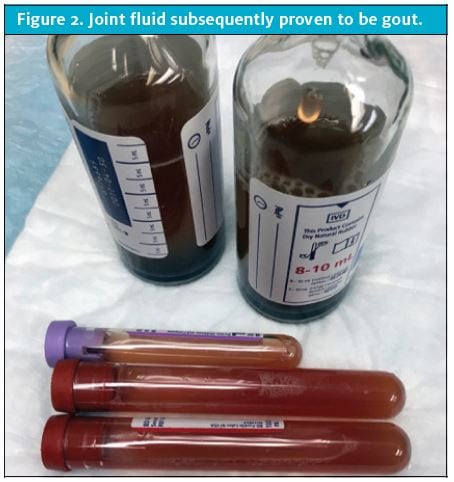
Joint fluid subsequently proven to be gout.
The mortality rate from septic arthritis remains about 18% despite adequate treatment. Preexisting conditions such as older age, renal or cardiac disease, synthetic material present in the joint, and immunosuppression contribute to mortality. Most patients will regain 50% to 90% of their preexisting level of joint mobility. This means most patients will experience some level of permanent joint dysfunction.
Infections occur in prosthetic joints in approximately 1% of all knee arthroplasties.2 This may result in failure of the prosthesis and is difficult to treat due to bacterial adherence to the prosthetic surface. This causes the formation of a biofilm which leads to the resistance to the host’s natural immune response. Many times, the hardware will eventually need to be removed to eradicate the infection. Any suspected septic prosthetic joint should be evaluated by the orthopedic surgeon who placed it as soon as possible, or be sent to emergency if that evaluation is not possible on the same day.
Gout is caused by elevated levels of uric acid and occurs in 1%‒2% of the Western civilization. The uric acid develops into urate crystals which then deposits in the joints as crystals or tophi. This then triggers an inflammatory pathway leading to a swollen painful joint in as little as 2-4 hours.7 This frequently occurs at night. Although the first metatarsal phalangeal joint is the most commonly affected, gout may also occur in the first metacarpal phalangeal joint, knee, ankle, wrist, or (rarely) other joints. Kidney stones can also occur. Rarely, there is widespread joint inflammation, fevers, and fatigue. Gout is more common in males, and those of African descent. An attack may be triggered by a high intake of meat and seafood, alcohol (beer more common than wine), and fructose-sweetened drinks.8 Chronic gout also occurs.
In the urgent care setting, the diagnosis of gout is almost always a clinical diagnosis. A definitive diagnosis of gouty arthritis is made by identification of monosodium urate crystals in synovial fluid obtained from an inflamed joint via arthrocentesis. Monosodium urate crystals are recognizable using polarized light microscopy. They are needle-like and have negative birefringence.
Pseudogout, also known as calcium pyrophosphate dehydrate (CPPD) crystal deposition disease, may cause joint inflammation and synovitis that presents in a manner similar to gout. The knee is the most commonly affected, and presents with gradually worsening pain, redness, and swelling over 12-24 hours. Joints with preexisting osteoarthritis are more likely affected. Women are more commonly affected, as are the elderly. The diagnosis of pseudogout is definitively made by testing synovial fluid for calcium pyrophosphate crystals. CPPD crystals are found on polarized light microscopy to be rhomboid shaped and have weakly positive birefringence.10
Gonococcal arthritis is a manifestation of disseminated Neisseria gonorrhea infection. These patients are usually young, healthy, and sexually active. The arthritis is generally in multiple joints, but may start as a single joint. The patient frequently has migratory arthralgia. Tenosynovitis is common. A painless, asymptomatic pustular rash may also be present. The arthritis is nonerosive in most cases. Both blood and joint cultures are typically negative, but the urethra, rectum, and pharynx may yield positive results and should be cultured.2 Patients should also be tested for coexisting sexually transmitted diseases such as chlamydia, hepatitis B and C, HIV, and syphilis.
Fungal arthritis does occur but is very rare in developed countries. Mycobacterium may also cause a subacute monoarthritis. Lyme arthritis can present as one joint, but is usually more. The onset is more indolent and may be intermittent. Borellia cannot be cultured from synovial fluid.
Rheumatoid arthritis usually occurs in multiple joints, but can present acutely with a single inflamed joint. Most commonly affected are the hands and wrists. The incidence is higher in women and increases with age. Onset is much more gradual than infection and gout. The diagnosis can be made clinically, but confirmed with x-rays, and bloodwork.
Other systemic autoimmune processes such as lupus, psoriatic arthritis, and reactive arthritis or Reiter’s disease may present with a monoarticular swollen joint, but these are far rarer and cause more systemic symptoms, or have a constellation of associated symptoms (rashes, vision, and urinary symptoms). It is important to always consider autoimmune processes as a cause of a red-hot joint, and obtaining a further history regarding systemic symptoms will help clue in to the possibility of a more systemic cause of the swollen joint.
Testing
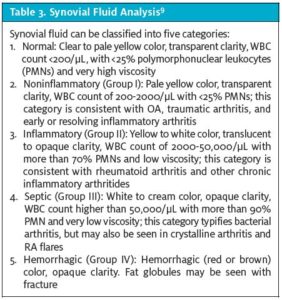
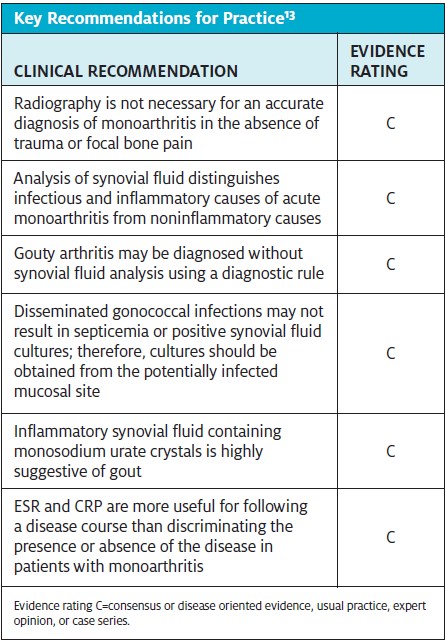
Blood tests are not useful in ruling septic arthritis in or out, and are not usually recommended in urgent care. If ordered, or in the emergency department, a WBC with differential, ESR, and CRP testing may be useful, but not diagnostic. Rheumatoid factor, ANA, and other markers of rheumatologic diseases are not useful acutely and should not be ordered from the urgent care center. Blood tests for uric acid are not a reliable test for gout, as the uric acid is normal 50% of the time during an acute attack. Blood cultures are of no use acutely, but will likely be done when the patient arrives at the hospital. Synovial fluid analysis is the gold standard, but not 100% diagnostic. A combination of clinical findings, lab studies, and clinical judgment are needed to make the diagnosis more likely.
Arthrocentesis can be performed in the urgent care center if the provider feels comfortable doing the procedure and the results can be obtained in a timely fashion. If this is not possible, the patient should be sent to the emergency department. Since all suspected cases should be admitted for orthopedic evaluation, IV antibiotics, and/or OR debridement, it may make more sense to avoid the procedure in the urgent care center and simply send the patient to the hospital. Only in cases when the diagnosis can be reliably ruled out, or another diagnosis (such as gout) is more likely, should the patient be sent home.
Joint fluid should be sent for a manual cell count, gram stain, culture, and evaluation for crystals if gout is suspected. The exam for crystals needs to be specifically requested in most institutions. Gram stain can be done in the clinic if you have the equipment available. Spare tubes for additional testing may be sent to the lab to hold. The fluid should be hand carried to the lab by a trusted person to be sure the sample is not lost, as it is not easily replaced.
Although there is no specific cutoff for synovial WBC count, any count >50,000 is considered a septic joint until the culture proves otherwise. Counts <25,000 are generally not infected, leaving 25,000 to 50,000 a gray area. The bottom line is that the culture is key to proving or disproving joint infection, which may take several days. Glucose, LDH, protein, and lactate have all been measured and are parts of various criteria, but have never been diagnostic on their own for joint sepsis. The old wives’ tale of being able to read through a tube of fluid excluding infection has also been debunked in recent years.11
Imaging is not useful acutely in most cases, although preexisting injuries or chronic degenerative disorders that may predispose to septic arthritis may be identified. Acute findings of septic arthritis on x-ray may only be a joint effusion. The risk for marginal bone erosion increases with the amount of time elapsed before treatment is initiated. Gas may be seen in the joint and soft tissues in infections with E coli, Enterobacter liquefaciens, and Clostridium. Late changes show bone destructions. Findings with crystal-induced arthropathies may include deposition of crystals or joint destruction, but are frequently normal. Bone erosions and tophi associated with gout are rarely seen.
Ultrasound may be useful to identify smaller effusions, distinguish bursitis from arthritis (as in shoulders or elbows), or to assist in arthrocentesis.
Treatment and Disposition
In the urgent care center, any patient suspected of having septic arthritis should be sent to the hospital for definitive care. These patients need urgent orthopedic evaluation and IV antibiotics.
For gout or pseudogout, nonsteroidal anti-inflammatory drugs (NSAIDs) should be given at their maximum recommended dosage until symptoms improve, then tapered gradually over several days. Indomethacin is a good first choice, but may be limited by adverse effects in some patients. Other NSAIDs with short half-lives can also be used; no specific NSAID is any more effective than the other and it is often a matter of personal choice.12
Colchicine may also be effective. At the first sign of attack, 1.2 mg should be given followed by 0.6 mg in 12 hours. Colchicine should be used cautiously in patients with renal insufficiency.
Steroids are a good alternative to NSAIDs and colchicine in patients with advanced age, renal insufficiency, CHF, and inability to take oral medication. Long-acting injectable forms such as triamcinolone acetonide or methylprednisolone acetate may be used, or prednisone 20-30 mg per day tapered over 7-10 days. Intraarticular cortisone injection may also be used.
Without treatment, acute attacks of gouty arthritis typically last a week or less. Unfortunately, the risk of a second attack within a year is greater than 50%. Pseudogout is treated similarly to gout.
Patients with suspected disseminated gonococcal infection should be admitted to the hospital and evaluated by an infectious disease specialist. Laboratory studies should be obtained before antibiotics are initiated. Intravenous ceftriaxone is the antibiotic of choice plus a single dose of azithromycin 1 g. Patients generally respond dramatically to treatment.
Treatment of Lyme arthritis and the acute rheumatological disorders are beyond the scope of the urgent care provider.
Case Resolution
The patient was transferred to the emergency department, where he underwent joint aspiration, revealing a WBC count of >50,000 WBC that was mostly poly’s. There were no crystals. He was seen by orthopedics, who took the patient to the operating room the same day and washed out the joint. He was placed on IV ceftriaxone and vancomycin. The cultures were eventually negative, but antibiotics were continued for 1 week. He was discharged home shortly thereafter.
Citation: Loeb M. The red-hot joint. J Urgent Care Med. July-August 2017. Available at: https://www.jucm.com/red-hot-joint/.
References
- Burton JH, Fortuna TJ. Joints and bursae. In: Tintinalli JE, Stapczynski O, Ma J, et al, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 8th New York, NY: McGraw Hill; 2016:chapter 284.
- Horowitz DL, Katzap E, Horowitz S, Barilla-laBarca M-L. Approach to septic arthritis. Am Fam Phys. 2011;84(6):653-660.
- Rosenberg R. Hip tendonitis and bursitis. Medscape. Updated December 14, 2016. Available at: http://emedicine.medscape.com/article/87169-overview. Accessed June 14, 2017.
- Carpenter CR, Schuur JD, Everett WW, Pines JM. Evidence-based diagnostics: adult septic arthritis. Acad Emerg Med. 2011;18(8):781-796.
- Askew KL. Septic arthritis. In: Sherman SC, Weber JM, Patwari RG, Schindlbeck MA, eds. Clinical Emergency Medicine. New York, NY: McGraw-Hill; 2014:410-413.
- Kaandorp CJ, Van Schaardenburg D, Krijnen P, et al. Risk factors for septic arthritis in patients with joint disease. A prospective study. Arthritis Rheum. 1995;38(12):1819-1825.
- Chen CJ, Shi Y, Hearn A, et al. MyD88-dependent IL-1 receptor signaling is essential for gouty inflammation stimulated by monosodium urate crystals. J Clin Invest. 2006;116(8):2262-2271.
- Richette P, Bardin T. Gout. Lancet. 375(9711):318–328.
- Courtney P, Doherty M. Joint aspiration and injection and synovial fluid analysis. Best Pract Res Clin Rheumatol. 2013;27(2):137-169.
- Dieppe P, Swan A. Identification of crystals in synovial fluid. Ann Rheum Dis. 1999;58(5):261–263.
- Lee KH, Choi ST, Lee SK, et al. Application of a novel diagnostic rule in the differential diagnosis between acute gouty arthritis and septic arthritis. J Korean Med Sci. 2015;30(6):700-704.
- Qaseem A, Harris RP, Forciea MA, Clinical Guidelines Committee of the American College of Physicians. Management of Acute and Recurrent Gout: A Clinical Practice Guideline from the American College of Physicians. Ann Intern Med. 2017;166(1):58–68.
- Becker JA, Daily JP, Pohlgeers KM, et al. Acute monoarthritis: diagnosis in adults. Am Fam Physician. 2016;94(10):810-816.
Tracey Q. Davidoff, MD and Michael Loeb, MD


