Q.Recently we removed a tampon that was retained for one week. What is the code for removing a foreign body from the vagina?
A.Although this procedure involves significant work, and the resultant foul odor can leave an exam room unusable for hours, the procedure is considered to be a part of the E/M. Of course, this is hard to understand, since there is a code for removing a foreign body from the external ear canal (69200) or the nares (30300). But coding is not always logical. One would hope that a code to compensate for the inconvenience and time spent on removing a vaginal foreign body will be developed. Until then, the procedure is not
Q.Recently, a woman presented with a fractured ring finger. The finger was quite swollen, and we had to cut off her ring with a ring cutter. What is the code for removing a ring from the finger?
A.Once again, cutting off a ring from a finger is considered to be a part of the evaluation and management (E/M) code. Of course, if you provide definitive treatment for the finger fracture, you should use the appropriate CPT code for treatment of the finger fracture, which will include 90 days of routine follow-up care.
These codes depend on documentation of whether the fracture was open (i.e., had an associated break in the skin) or closed and whether the fracture was or was not manipulated by the treating physician, so make sure that you have a separate and identifiable procedure note that documents these aspects of the treatment.
If you refer the patient to another physician for the definitive treatment of the finger fracture, you can still code for the appropriate E/M level, the supply code for a finger splint (Q4049), and code for finger splint application (29130).
Q.What is the code for simply removing a splinter with a forceps?
A.With a few exceptions, if the removal requires no incision and if you simply remove the splinter with a forceps, then there is no specific CPT code for the splinter removal and the removal is included in the E/M code.
In the case of larger splinters, I have personally seen several abscesses complicate supposedly simple splinter removal procedures. These abscesses occurred because the initial foreign body removal left a small retained splinter fragment.
Thus, it is good clinical practice—when possible without risk to deeper structures and especially with splinters from older wood—to make an incision and visualize the entire splinter prior to removal. This practice helps ensure that the entire splinter is removed and no splinter fragments are retained in the wound.
If the foreign body is located in the skin (epidermis and dermis) and has not penetrated the subcutaneous tissues, then the removal of a foreign body never warrants a procedure code separate from the E/M code.
Q.We had a patient step on a one-inch splinter and the doctor removed the splinter from the foot with a forceps. No incision was made. What code is appropriate?
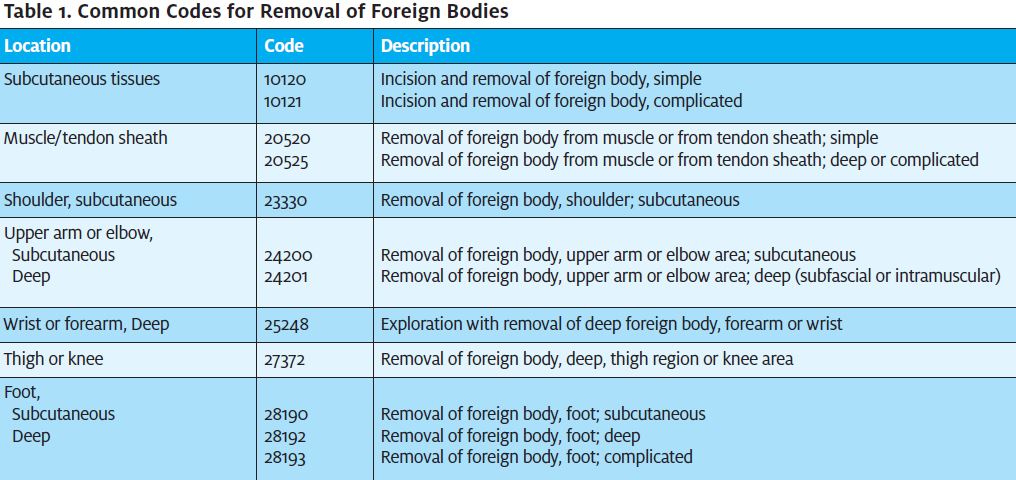
A.Here is where coding gets a little tricky and knowledge of the fine print can allow for better reimbursement. Unlike the generic code for simple foreign body removal from subcutaneous tissue (10120), the code for removing a foreign body from the subcutaneous tissue of the foot does not specifically require incision as part of the removal to use the specific code for “removal of foreign body, foot; subcutaneous” (28190). Several other codes for foreign body removal from subcutaneous tissue also do not require the physician to perform an incision (Table 1). (Note: Although we are unaware of an official statement on this issue by CMS or the AMA, some payors and some coding authorities do consider an incision to be necessary to bill for these codes, so check with your payor.)
Q.We had a patient with a fish hook and barb in the palm of his hand. The doctor pushed the hook forward and advanced the barb through the skin. She then cut off the rest of the hook and then slid the hook out of the skin. How is this coded?
A.Some coders argue that since no incision was made, the hook removal is included in the E/M code. Others may hold that since the advancing of the hook made its own incision (howbeit less than 1 mm), one can use the code for subcutaneous foreign body removal with incision. This may be a semantic distinction, as the so called “incision” is really just an iatrogenic puncture wound.
Prior to being aware of the coding implications, I generally made an incision in the skin to allow the tip of the advancing hook to slide though the skin. This technique makes the procedure simpler and less traumatic to the patient. In addition, the incision removes any controversy about whether the foreign body removal is compensable with the code 10120 (incision and removal of foreign body, simple).
Q.Several foreign body removal and incision and drainage codes distinguish between simple and complicated procedures. Does CPT or CMS give any guidelines to help the physician determine whether the procedure is simple or complicated?
A.To quote from CPT Assistant (December, 2006), “No. The choice of code is at the physician’s discretion, based on the level of difficulty involved in the incision and drainage procedure.” Of course, to help avoid disagreements with payors, the procedure note should always contain information to help support the physician’s deter mination that the procedure was complicated.
Q.Our physician spent an hour exploring for a foreign body in a foot. I had to make an incision of about 4 cm to explore for the foreign body. May I add the code for the simple wound repair (12002) to the code for the complicated subcutaneous foreign body removal (10121)?
A.No. The wound repair would be considered to be included in the foreign body removal code. You may, however, use the code for deep foreign body removal from the foot (28192) or the code for complicated foreign body removal from the foot (28193) as appropriate (Table 1). Typically, these codes have significantly higher reimbursement than the code for a simple subcutaneous foreign body removal.
Note: CPT codes, descriptions, and other data only are copyright 2007 American Medical Association. All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the American Medical Association (AMA).
Disclaimer: JUCM and the author provide this information for educational purposes only. The reader should not make any application of this information without consulting with the particular payors in question and/or obtaining appropriate legal advice.
DAVID STERN, MD (Practice Velocity)

