Urgent message: A pretravel consultation assesses the patient’s fitness for travel in the context of anticipated risks associated with their journey. This individualized counseling takes into account not just age or destination, but also general health and other factors such as past travel experience. Given the proliferation of single-specialty travel medicine clinics, with appropriate training and preparation, these assessments can easily be performed in the urgent care setting.
Benjamin Silverberg, MD, MSc, FAAFP, FCUCM
Citation: Silverberg B. Pretravel consultations in the urgent care setting. J Urgent Care Med. 2021;15(7):13-20.
INTRODUCTION
| A Word About the COVID-19 Pandemic The ever-changing issue of the COVID-19 pandemic is outside the purview of this article. However, it should be noted that at this time both domestic and international travel is beginning to “open up” more for Americans. Urgent care patients should be encouraged to receive the COVID-19 vaccine, and counseled to investigate updated requirements (such as those issued by the Centers for Disease Control and Prevention) for vaccination status, quarantine, and testing related to the virus before traveling to any destination in the U.S. or abroad. |
People travel for vacation and tourism, school or work, for adventure, and for volunteer and religious purposes. Of those who travel internationally, 36% seek advice from a medical provider; among those, approximately 40% receive counseling from someone other than their primary medical provider. Health risks abroad are not limited to infectious diseases; indeed, the journey itself can pose risk (eg, DVT, unsafe vehicles). Unclean food and water, environmental exposures (eg, altitude, heat/cold, pollution, animals), and other stressors (eg, unsafe sexual contact, culture shock) can sour a traveler’s experience. Unfortunately, upwards of 8% of international travelers need medical attention either during or after their trip.1,2 As such, it is important that urgent care providers are able to counsel travelers on the risks they may face abroad and how to reduce the chance of succumbing to illness, injury, or death.
BACKGROUND
A travel medicine consultation assesses the client’s fitness for travel in the context of the anticipated risks associated with their journey.3 This requires an individualized approach. For example, by age alone, a 61-year-old traveler hiking the Inca Trail in Peru might be expected to have a more difficult experience than a 21-year-old—unless the 61-year-old is a marathon runner and the 21-year-old has uncontrolled asthma, in which case your concern for their welfare will likely shift. Your role as a consultant is to give the traveler the appropriate and necessary immunizations, medications, and knowledge to prepare them to go abroad safely.
INTAKE FORMS
Ideally, pretravel consultations are scheduled 4-6 weeks prior to departure. Nevertheless, even last-minute consultations can be helpful. Either way, they require preparation. An intake form—preferably completed and reviewed in advance of the actual clinical visit—should review key elements of the traveler’s own health: age, gender, chronic medical conditions, allergies, medications, immunization history, prior travel experience, and special conditions or circumstances (eg, pregnancy, breastfeeding, immune-compromise, physical disability). This form should also query the proposed itinerary: destination country/countries (in chronologic order), duration abroad, reason for travel (eg, business or leisure), travel “style” (eg, visiting traditional tourist sites or going off the beaten path, types and quality of accommodations, modes of transportation), and any anticipated risky activities (eg, high altitude, contact with animals).
VACCINATIONS
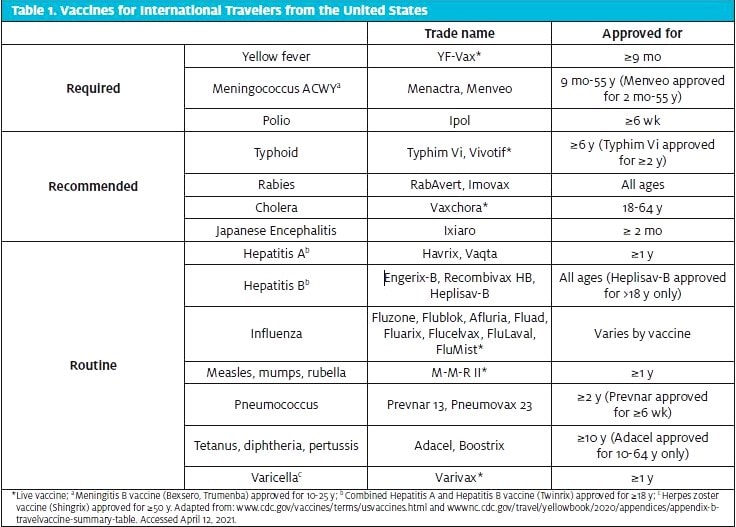
It is not uncommon for travelers to forget to bring documentation of their past immunizations, or to be uncertain of what they have received. With regard to travel, there are three categories of vaccines: required, recommended, and routine (see Table 1).1 Live vaccines are not recommended for immunocompromised patients or pregnant women. Some vaccines have oral formulations (eg, Vivotif, Vaxchora). Depending on the traveler’s itinerary, only yellow fever, meningitis, and/or polio vaccines may be required for entry into (or exit from) a foreign country. Typically, though, vaccination against typhoid, hepatitis A, and tetanus are also recommended. The information in Table 1 is current as of April 2020 and should serve as a starting point for your reference.
Yellow Fever (YF)
Potentially fatal mosquito-borne virus
The yellow fever vaccine is probably one of the more complicated topics you’ll cover with the traveler. The risk of side effects increases with age (>60 years old), and it’s not always easy to balance out the risk of vaccination vs the risk of getting infected. Typically, African countries require vaccination for border entry, whereas Latin American ones just recommend it. Unfortunately, there has been a nationwide shortage of YF-Vax since 2016, which has led to importation of Stamaril from France. Only designated yellow fever vaccination centers can administer the vaccine. The patient then receives a literal yellow card with documentation of their vaccination and an official stamp. Though this card can be replaced if lost, a valid, physical card is necessary for travel—a photocopy or scanned image will not suffice. As per the CDC and ACIP, a single dose of yellow fever vaccine is thought to provide lifelong coverage, with some exceptions (eg, HIV-positive individuals). There is, however, a chance that an immigration official will not know (or honor) this. In general, while revaccination typically is not necessary, it might be “required” with certain international aid organizations. If the patient tolerated the shot the first time, it should be fine to readminister. Immunity starts developing within 10 days of vaccination and usually is complete within 1 month. Contraindications to vaccination include infants younger than 6 months of age and immunosuppressed travelers. These individuals will need a signed and stamped waiver. Since this paper affords no actual medical protection, counseling against travel is, of course, an option.
Hepatitis A
Fecal/oral-transmitted virus
Younger travelers are likely to have already received vaccination against hepatitis A, but older travelers may not have. Since the vaccine affords lifelong protection, checking titers is unnecessary if vaccination dates can be confirmed. If not, repeating the series may be appropriate. This vaccine is strongly recommended for travel to most developing countries and even some domestic regions due to disease outbreaks (eg, Central Appalachia). A common error in administration is forgetting that Twinrix, which confers protection against hepatitis A and B, contains a pediatric dose of hepatitis A (equivalent to half that of an adult dose). Thus, to complete the hepatitis A series, either a total of three doses of Twinrix or two doses of Havrix or Vaqta are needed.
Typhoid
Fecal/oral-transmitted bacterium
The oral vaccine (Ty21a, brand name Vivotif) is taken every other day for four doses and must be kept refrigerated. Travelers should try to get this started at least 2-3 weeks before going abroad, as the oral vaccine takes a week to administer, and it takes 7-10 days to build an immune response. Since it is a live vaccine, it can cause some GI upset and, separately, it cannot be taken simultaneously with antibiotics (eg, if the patient has a concomitant UTI). Vivotif provides protection for 5 years.
The injectable vaccine (Vi polysaccharide, brand name Typhim) is attenuated and affords protection for 2-3 years. It, too, should be given ≥7-10 days prior to travel.
The oral formulation can be given to travelers starting at 6 years of age and is typically less expensive than the intramuscular vaccine, though the latter can be given to children as young as age 2 years.
Vaccination in either form provides imperfect protection; reports generally range from 48% to 80% efficacy.4 Since immunity against typhoid does wane over time, this vaccine is often included on a traveler’s yellow card, if they have one. (Note that some patients of foreign birth or heritage decline this vaccine on the basis that they are going back “home” to visit friends or relatives [VFRs], and in fact may not be inclined to take as many precautions. However, their immunity may have either faded or never developed in the first place. These patients must be reminded they are indeed at risk.)
Influenza
Droplet-transmitted virus
The guidelines for seasonal influenza vaccination are basically the same for patients staying stateside as those traveling abroad. The classic “flu season” is protracted around Equatorial countries and “flipped” in the Southern Hemisphere (ie, a traveler to Australia in July should give some foresight to the flu). Avian and swine flu are beyond the scope of this review.
Hepatitis B
Blood-borne virus
Most individuals who have attended public school have been immunized against hepatitis B as a child, but immunity does wane. Unless specifically required, a titer to prove (or disprove) immunity is unnecessary, as the patient is typically paying out-of-pocket for their travel visit anyway. When in doubt, it’s better to reimmunize, either as a single booster or the whole series (day 0, 1-2 months after that, and 6 months after the first dose). Since there is no vaccine against hepatitis C at the present time, when you discuss hepatitis B, it may also be a good time to bring up safer sex practices while abroad.
Measles, Mumps, and Rubella (MMR)
Droplet-transmitted viruses
Again, most Americans born in 1957 or later have had this two-shot series. Like hepatitis B, drawing titers is usually unnecessary.
Polio
Fecal/oral-transmitted virus
Only a handful of countries will require a recent poliomyelitis adult booster for exit (eg, travelers staying >4 weeks in Pakistan or Afghanistan), but if the traveler is not an American national, there may be other requirements.
Rabies
Fatal virus transmitted through animal bites
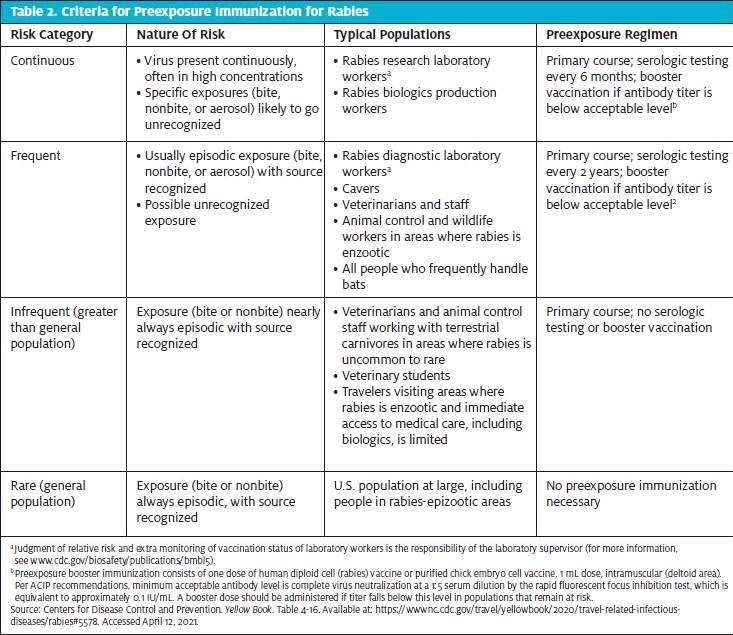
Vaccination is costly, uncomfortable, and doesn’t necessarily preclude cutting travel short if one gets bitten while abroad. Generally, rabies vaccination is only recommended for travelers who will be at an increased risk: veterinary clinic workers or people involved in animal rescue, spelunkers (who may come into contact with bats), or people researching the rabies virus itself. The CDC’s Yellow Book has an excellent table to help you risk-stratify (see Table 2). Higher-risk areas include South and Southeast Asia, Tropical Africa, and Central America. If you do vaccinate, it is offered on days 0, 7, and 21 (or 0, 7, and 28). Antibody levels should be checked every 2 years and a booster given if needed. Since even a vaccinated person who is exposed will require some medical treatment, it is advisable to also discuss medical evacuation insurance and to differentiate it from travel and health insurance.
Japanese Encephalitis (JE)
Mosquito-borne virus
Vaccination against JE is expensive. It is usually dosed at days 0 and 28, though the FDA has approved an expedited dosing schedule at days 0 and 7 for adults 18-65 years of age, with similar efficacy and without increased side effects. Ixiaro is recommended for travelers to rural agricultural areas in Asia (eg, Chiang Mai Valley in Thailand) who will be abroad for >1 month during transmission season (usually May through October). Expatriates may also need vaccination. A booster may be needed after 1-2 years if there is ongoing risk.
Tick-Borne Encephalitis (TBE)
Virus spread by arthropods or in unpasteurized dairy products
Unfortunately, the vaccine against TBE (given as three intramuscular injections over 6 months) is only available in Europe and Australia. If a traveler is going to a country affected by this illness, encourage use of bug spray and performance of “tick checks,” even in urban areas.
Meningococcus
Potentially fatal droplet-transmitted bacterium
The clinical entity of meningitis can have bacterial, viral, fungal, and parasitic etiologies.
Routine childhood vaccination against bacterial meningitis is common in many countries. Apart from providing preventative care, and unless the traveler is a healthcare professional or an immunocompromised patient at increased risk, one of the only times you’ll have to worry about meningitis vaccination is when someone is traveling to the so-called Meningitis Belt of sub-Saharan Africa during the dry season (December to June). Most of the countries in this region only have a section of their territory affected, so knowing the traveler’s exact destination is important. Travelers to this area risk infection with the A, C, W, and Y strains of bacterial meningitis. The B strain is extremely rare in this area, and the meningitis B (MenB) vaccine is not currently recommended for travelers except those going to areas with an active outbreak.
In addition, Saudi Arabia requires proof of vaccination against the A, C, W, and Y strains for travelers going there for Hajj or Umrah pilgrimage.
Travelers between 2 and 55 years of age should get MenACWY. Though MenACWY is not licensed in the United States for vaccination of individuals 56 years-old and above, the polysaccharide vaccine (MPSV4, brand name Menomune) was discontinued in 2017, so MenACWY is used by default.
Cholera
Water-borne bacterium
In theory, this ranks with hepatitis A and typhoid in terms of health impact, but vaccination with Vaxchora is usually only recommended for aid and refugee workers (eg, UN relief workers). The classic presentation of this acute diarrheal illness is “rice water stool.” Dukoral, which is not available in the United States, is a two-dose, inactivated vaccine that also affords some protection against enterotoxigenic Escherichia coli (ETEC).
Tetanus, Diphtheria, and Pertussis (Tdap)
Droplet-transmitted bacteria (Clostridium tetani spores are also found in soil and animal manure)
For international travelers, Tdap, which includes protection against whooping cough, is preferred over the “plain” Td booster. Most adolescents will be up to date on their tetanus vaccination, but older adults may need a booster. It is typically given to women just after giving birth—which can help narrow down the administration date for some travelers—but is often forgotten for other close household contacts. Regardless, after the initial childhood series, a tetanus booster should be given every 10 years.
Pneumococcus
Droplet-transmitted bacterium
The guidelines changed within the last few years to advise Prevnar (PCV13) at age 65 and Pneumovax (PCV23) 6-12 months later. Individuals who received Pneumovax without Prevnar preceding it (ie, before the guideline changed) are becoming fewer and fewer. Pneumococcal vaccine can be given earlier than age 65 if the traveler has certain comorbidities such as asthma or diabetes.
Varicella
Droplet-transmitted virus
Similar to MMR, Americans born after 1979 should have already been vaccinated (and those born prior probably already had the illness). For older adults, consider immunization against herpes zoster (shingles) with Shingrix, which effectively replaced Zostavax in 2018.
OTHER PHARMACOPROPHYLAXIS AND TREATMENT
Malaria
Parasite transmitted by mosquitoes that bite from dusk to dawn
Along with yellow fever, hepatitis A, typhoid, and potentially rabies, this is one of the most important topics to cover with travelers.
Some countries are plagued with the disease and some only have spotty areas of transmission. Elevation matters (eg, tropical lowlands are particularly at risk). As such, this is another instance in which you need to know the traveler’s exact destination(s). A visitor to Brazil, for instance, may go in and out of endemic regions during their travel to popular tourist spots, and/or the risk may change by season. A visitor to Ghana will need continual prophylaxis.
Chloroquine (Aralen) resistance is prevalent outside of Central America, so normally one’s options for prophylaxis include atovaquone-proguanil (Malarone), doxycycline, tafenoquine (Arakoda), and mefloquine (Lariam). Doxycycline can be photosensitizing, but the bigger drawback is gastrointestinal upset. Additionally, it must be taken for a full month upon exiting the endemic region. Nonetheless, it is a relatively cost-effective option for long-term exposure. Tafenoquine is a newer drug that is taken weekly after a loading dose. Mefloquine, which is also taken weekly, is a reasonable option for the long-term traveler or expatriate, but it can cause vivid dreams or nightmares and carries a black-box warning for drug-induced psychosis. The risk is much higher in individuals with any kind of psychiatric history—even mild anxiety or depression. If a traveler would like to use mefloquine for malaria prophylaxis, offer a trial period of taking the medication starting at least 1 month before going abroad. That way, if the patient finds it intolerable, there is still time to switch to a different medication. Travelers with G6PD should not use chloroquine, primaquine, mefloquine, or tafenoquine.
Many travelers opt for atovaquone-proguanil, which is taken daily and starts 1-2 days before entering the endemic region, daily while there, and for 7 days upon exit. A little buffer in pill count (eg, rounding up to the next even number) may be helpful in the event of travel delays. Long-term travelers to remote areas may wish to bring a malaria self-treatment regimen of either atovaquone-proguanil or artemether-lumefantrine (Coartem) in case they become infected.
Discussion about malaria chemoprophylaxis offers a good opportunity to talk to patients about counterfeit medications that may be found abroad. Proclaimed antimalarial prophylaxis is not something travelers should take a gamble on. (It is noteworthy to mention that a person cannot safely ingest enough tonic water to protect them from malaria—something some patients still ask about.)
Regarding insect repellent, 20%-50% DEET provides coverage for about 4-6 hours per application and is safe for pregnant women and children as young as 2 months of age. If used with sunblock, it should be applied second (ie, after the sunblock), though it is important to note it may reduce the sunblock’s efficacy.5 Appropriate alternative insect repellents include 20% picaridin and permethrin-impregnated clothing and/or bed nets. Bottles of permethrin can be purchased for self-treatment of clothing and linens, but it is usually easier to buy pretreated items because permethrin can wear out clothing more quickly and can only endure a few laundry washes before retreatment must be performed.
Traveler’s Diarrhea
Common illness among travelers, with multiple different etiologies
Traveler’s diarrhea is defined by the sudden onset of abnormally loose, frequent stools (three or more episodes in a 24-hour period). The safety of the local water supply should be a constant consideration. Is the tap water potable? To be safe, travelers should use bottled water, even when brushing their teeth. Counsel them about food safety (ie, the old adage “cook it, boil it, peel it, or forget it”). Avoid ice cubes, “street meat,” and hard-to-wash foods (eg, strawberries).
Mild diarrhea
For mild diarrhea, fluid repletion with clean water or a sports drink like Gatorade is important (though Coca-Cola will work in a pinch). Travelers may consider bringing packets of oral rehydration salts, though this still requires access to clean water. When in doubt, fizzy water (ie, tonic or seltzer water) is typically safer than still, as one can more easily tell if the container has been tampered with.
Loperamide, an antimotility agent, will certainly stanch diarrhea—but can cause constipation instead. This double-edged sword may be fine if there is an important meeting, wedding, or other event that cannot be missed (or if the patient will be traveling long distances without easy access to a sanitary bathroom facility), but it also theoretically keeps the causative agent inside them longer. It may be better to have the traveler just excrete whatever is making them sick and replete fluid losses. Bismuth subsalicylate (Pepto-Bismol or Kaopectate) helps with cramping and bloating without causing constipation. These medicines can cause darker-colored stool and shouldn’t be used if the traveler can’t take aspirin.
Moderate diarrhea
“Moderate diarrhea” is more than just some loose stool due to a change in diet. Rather, it is an illness that includes fever, stomach cramps, and muscle aches. Since it presupposes a bacterial etiology, there is significant debate in the medical community about supplying travelers with antibiotics for self-treatment prior to them even falling ill. Due to increasing resistance and the risk of spontaneous tendon rupture, fluoroquinolones (namely, ciprofloxacin) are no longer the preferred agent for self-treatment. Instead, azithromycin (500 mg taken daily for up to 3 days if symptoms do not resolve sooner) is the current standard, regardless of destination. Depending on the length of time abroad, you may prescribe multiple courses. Unfortunately, azithromycin interacts with some SSRIs. In the case of drug allergies or interactions, rifaximin may be a reasonable, albeit expensive, alternative.
While these medications can be dosed for children, parents often find the regimen inconvenient. As such, they may opt to be aggressive with hydration and rehydration, and to seek out proper medical care early if needed.
Severe diarrhea
Lastly, severe diarrhea (noted by treatment failure with 3 days’ worth of azithromycin, intractable vomiting, and/or bloody diarrhea [dysentery]) should prompt medical evaluation as well. The patient could be suffering from a parasitic infection like Entamoeba histolytica.
Though travelers may tell you they have received prescriptions for antiemetics, antiparasitics, or other antibiotics from other providers, there is no evidence to support this practice. Only if the traveler is going to be on their own in a remote location and has medical training might this be reasonable.
OTHER COUNSELING TOPICS
Access to Medical Care Abroad
Many pretravel consults do not include a thorough physical exam. Instead, the patient is often taken at their word regarding medical and psychiatric comorbidities. If strenuous activities are planned, however, consider a more formal assessment of the traveler’s fitness (eg, cardiac risk stratification). These activities (eg, hiking Mount Kilimanjaro) should only be pursued in consultation with a reputable tour company and guides. Similarly, travelers should know where they can access appropriate medical care abroad (eg, a decompression chamber, if going diving), as well as the location of their embassy or consulate. The International Society of Travel Medicine (ISTM, www.istm.org) and the International Association for Medical Assistance to Travelers (IAMAT, www.iamat.org) both maintain listings of international clinics on their respective websites.
Environmental Hazards
Remind travelers to stay fluid hydrated, especially during airplane travel. Where appropriate, dress in layers. Allow time to acclimatize to altitude. If this is not possible, or for those who report being particularly sensitive to high elevations, consider acetazolamide (Diamox) or dexamethasone. Consider anticipated exposure to air pollution, especially for travelers with respiratory conditions. Travelers should use caution when swimming in the ocean (eg, undertow/riptide, aquatic life) as well as in fresh water (eg, schistosoma). Avoid walking barefoot. Use sunblock.
Interpersonal Risks
Travelers should not draw unnecessary attention to themselves. Do not bring flashy jewelry or other markers of wealth (eg, expensive electronics). Do not use unlicensed taxis (“gypsy cabs”). Avoid using bank ATMs that are not well lit or protected from the street (eg, without a security guard standing by). Travelers should take care that no one is observing their PIN code or following them afterwards. Backpacks and purses should remain within one’s direct line of sight, especially in crowded buses, trains, restaurants, and bars. A money belt and/or a “decoy” wallet/purse should be considered. As in the domestic setting, sexual contact should include undamaged latex condoms.
Airplane Travel
Nearly two-thirds of in-flight medical emergencies are related to preexisting health issues. Individuals traveling with medical devices (eg, pneumatic splints, feeding tubes, cuffed endotracheal/tracheostomy tubes, urinary catheters) should use caution due to pressurization of the airplane cabin. If a traveler has a resting oxygen saturation <92% at sea level, they should probably travel with a portable oxygen concentrator.6These devices require preflight approval by the airline, and the paperwork between airlines varies.
Similarly, individual airlines have their own policies regarding medical “clearance” prior to air travel. The International Air Transport Association (IATA) recommends completion of a Medical Information Form (MEDIF) if an individual’s fitness for travel is in doubt due to recent illness, injury, hospitalization, surgery, or instability of acute or chronic medical condition, or if special services (eg, portable oxygen) are required.7 Medical clearance is generally not required for wheelchairs or other assistive devices.
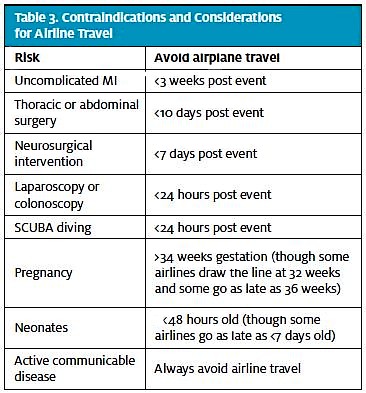
Specific contraindications for airplane travel are outlined in Table 3.8-10
TRAINING AND CERTIFICATION
Many universities have training programs in tropical medicine. The ISTM offers a Certificate of Knowledge for medical providers who take and successfully pass their comprehensive exam in Travel Medicine. The American Society of Tropical Medicine and Hygiene (ASTMH), the National Health Service (NHS), and CDC Training and Continuing Education Online (TCEO) offer other opportunities for education and scholarship.
TAKE-HOME POINTS
- A travel medicine consultation is an assessment of possible health risks abroad, viewed through the lens of the patient’s own fitness for travel.
- Yellow fever—and depending on the destination, meningitis and/or polio—are the only “required” vaccines for international travel, though typically typhoid, hepatitis A, and tetanus vaccinations are also recommended.
- Where appropriate, travelers should use oral prophylaxis against malaria as well as DEET-containing insect repellent and mosquito nets.
| Resources Advances in prophylaxis and treatment can quickly render previous regimens obsolete. Thus, it is important to stay up to date with current recommendations. The following resources may help inform recommendations you make to patients for whom you are performing a pretravel consultation: – The Centers for Disease Control and Prevention’s Yellow Book—so named because it is indeed yellow—is available for free online at wwwnc.cdc.gov/travel/page/yellowbook-home. A print version is updated at least every other year and can be purchased through various retailers. The travel vaccine summary (Appendix B) and summary of immunization of immunocompromised adults (Chapter 5) are particularly useful references. – The U.S. Department of State maintains a helpful website at travel.state.gov/content/travel/en/international-travel.html. Though it is certainly possible to review health information through a country’s own consulate, this information may intentionally or unintentionally minimize risks. – Shoreland’s Travax (www.travax.com) is a subscription-based third-party company that provides location-specific travel guidance on international health risks, including infectious diseases, natural disasters, and interpersonal violence. |
- Travelers should also consider OTC medications and oral antibiotics for self-treatment of traveler’s diarrhea.
References
- Sanford C, McConnell A, Osborn J. The pretravel consultation. Am Fam Physician. 2016. 15;94(8):620-627.
- Noble LM, Wilcox A, Behrens RH. Travel clinic consultation and risk assessment. Infec Dis Clin N Am. 2012;20:575-593.
- Gheradin T. The pre-travel consultation – an overview. Austral Fam Physician. 200736(5): 300-303.
- Jackson BR, Iqbal S, Mahon B. Updated recommendations for the use of typhoid vaccine—ACIP, US, 2015. MMWR. 2015;64(11):305-308.
- Yellow Book 2020, chapter 3
- Edvardsen A, Akerø A, Christensen CC, et al. Air travel and chronic obstructive pulmonary disease: a new algorithm for pre-flight evaluation. BMJ Thorax. 2012;67(11):964-969.
- Martin-Gill C, Doyle TJ, Yealy DM. In-flight medical emergencies: a review. JAMA. 2018;320(24):2580-2590.
- Bourell L, Turner MD. Management of In-flight medical emergencies. J Oral Maxillofac Surg. 2010;68(6):1377-1383.
- Donner HJ. Is There a doctor onboard? Medical emergencies at 40,000 Feet. Emerg Med Clin N Am. 2017;35(2):443-463.
- Aerospace Medical Association. Available at: www.asma.org. Accessed March 23, 2020.
The author thanks Kevin Bernstein, MD, MMS, CAQSM, FAAFP and Gregory Juckett, MD, MPH, FAAFP, for their thoughtful feedback during the development of this manuscript.
Author affiliations: Benjamin Silverberg, MD MSc FAAFP, FCUCM Departments of Emergency Medicine and Family Medicine, West Virginia University; Division of Physician Assistant Studies in the Department of Human Performance, West Virginia University. The author has received a Certificate in Travel Health from the International Society of Travel Medicine. He reports no relevant financial relationships with any commercial interests.
Adapted for the urgent care provider from the American Academy of Family Physicians’ Practice Management Handbook (2020).

