Urgent message: Patients present to urgent care with a variety of complaints, many of which are common—even if they are the result of an uncommon condition. It is important that the provider develop a broad differential diagnosis as they approach these problems.
Richard A Ginnetti, MD, MBA, CPE and Justin Holschbach, MD
CASE PRESENTATION
History
A 52-year-old male presents to urgent care with the chief complaint of new lower posterior neck and right shoulder pain of 5 days’ duration. He describes the pain as “aching.” It is aggravated by movement of his neck or shoulder. He feels that he may have “slept on it wrong.” There is no history of trauma. He denies headache, fever, numbness, or weakness in the right arm and neck. His is right hand dominant. His past medical history is significant for left nephrectomy for T1b Grade 2 renal cell carcinoma 9 years ago. He takes no chronic medications and has no known drug allergies.
Physical Examination
Physical exam reveals a slightly overweight male in no apparent distress. Vital signs:
- Blood pressure 156/98
- Pulse 90/min
- Respiratory Rate 16/min
- Temperature 97.9° F
- Weight 257 lbs
- Height 73 inches
The patient’s head was normocephalic and atraumatic. He has tenderness in the right posterior neck and shoulder. He has pain with normal range of motion (NROM) of the neck, but the neck was supple. Shoulders demonstrated NROM. He had normal strength in the upper extremities. There was no rash.
Follow-Up
The patient presented to the emergency department 3 days later after lack of response to methylprednisolone and cyclobenzaprine prescribed initially. Cervical spine x-rays demonstrated straightening of the cervical lordosis. He was discharged on oral medication. Three weeks later he presented to his primary care provider. Examination at that time was significant for Spurling’s test with pain in the neck without radiation to the right arm. Radial pulses and temperature of hands were normal. He had 4/5 strength in the right biceps; otherwise, no weakness was noted. He had an MRI of the cervical spine with mild spinal stenosis and mild broad-based disc herniation at C4-C5 and C5-C6. He was referred for electromyography (EMG) and nerve conduction study, but symptoms resolved prior to his consultation. He was diagnosed with Parsonage-Turner syndrome (PTS). He made a full recovery over the subsequent months.
The Clinical Entity
PTS, also known as neuralgic amyotrophy and brachial plexus neuritis, is an uncommon cause of upper extremity pain and weakness. A series of 136 case was described in 1948 by M.J. Parsonage and J.W. Turner.1 The common presentation is severe pain in the shoulder and arm that is followed by the development of weakness, which can occur over days or weeks.2,3 This condition has been noted to wake patients up from sleep.2 This clinical entity is often misdiagnosed as a cervical radiculopathy.
Etiology and Epidemiology
Idiopathic and hereditary forms of neuralgic amyotrophy have been identified. The exact cause of the idiopathic form has not been identified but potential triggers include infection, antecedent immunization, Hepatitis B, and strenuous exercise.2,4,5
This condition most commonly occurs in males between 20 and 60 years of age.2 Classically, the incidence of brachial plexus neuritis was thought to be approximately two cases per 100,000 persons.2,4 In recent years it is felt to be more common than previously recognized and a significant proportion of cases have been known to recur. 6
Differential Diagnosis
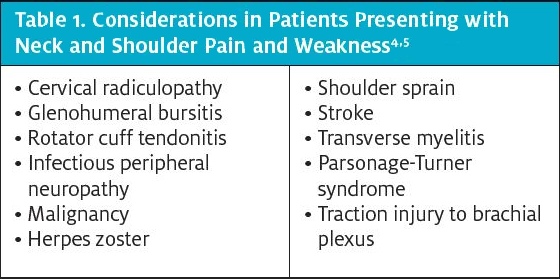
Diagnosis of Parsonage-Turner syndrome is mainly clinical and made by exclusion of other conditions that can present in a similar fashion. It is often confused with more common conditions involving the cervical spine and rotator cuff disease. (See Table 1 for conditions to consider with patients presenting with neck and shoulder pain and weakness.)
Evaluation
Laboratory abnormalities associated with neuralgic amyotrophy are unremarkable. Blood tests may show mildly abnormal liver function tests but inflammatory markers such as erythrocyte sedimentation rate and C-reactive protein are often normal.4,6. Evaluation on the cerebrospinal fluid could be normal but may show a mildly elevated protein.7
Patients may typically start an imaging evaluation with plain cervical spine x-rays, shoulder x-ray, and possibly a chest x-ray to rule out a Pancoast tumor of the lung. MRI exams are typically obtained in the evaluation of these patients for not only the evaluation of the condition but more frequently for exclusion of some of the conditions already listed in Table 1. With the advancement of MRI and ultrasound technology, structural peripheral nerve abnormalities called hourglass constrictions have been identified in some patients with Parsonage-Turner syndrome.8,9
The use of nerve conduction studies and EMG are essential in confirming the diagnosis of PTS and excluding other causes of the patient’s condition. EMG findings may vary from mild to extensive denervation of the affected muscle group.10
TREATMENT
Treatment in the acute phase of neuralgic amyotrophy involves adequate pain control. Pain can be severe and may require multimodal analgesia. One unblinded uncontrolled retrospective study suggested early corticosteroids may improve pain and speed up recovery in a few patients.11 In patients that have failed conservative therapies, surgical options may be considered.8
CONCLUSION
Cervical and shoulder conditions are common chief complaints of patients presenting to urgent care. Although the complaint is common, the underlying cause may not be clear, and it is imperative to develop a broad differential diagnosis. As noted in this case, a common complaint was caused by an uncommon condition.
The patient described in this case experienced a fairly typical course for a patient with PTS. He presented with idiopathic pain and then progressed to weakness in his upper extremity. He made a full recovery; unfortunately, this is not the case for all patients. One large study showed 60% of patients still experienced pain 6 to 24 months in the clinical course and 80% had difficulty performing overhead tasks.6
Take-Home Points
This case brings to light a few key concepts that are important for urgent care clinicians to consider:
- Things may not be as they appear; keep your differential diagnosis broad.
- Have a higher index of suspicion when a patient presents for the second time.
- This patient has a history of cancer. Although not a factor in this case, this is something to consider in your evaluation of the patient at hand.
- Post visit instructions must be thorough and specific. This patient was instructed to follow up not only for his chief complaint but also his elevated blood pressure.
REFERENCES
- Parsonage MJ, Turner JW. Neuralgic amyotrophy; the shoulder-girdle syndrome. Lancet. 1948;1(6513):973-978.
- Miller JD, Pruitt S, McDonald TJ. Acute brachial plexus neuritis: an uncommon cause of shoulder pain. Am Fam Physician. 2000;62(9):2067-2072.
- Stutz CM. Neuralgic amyotrophy: Parsonage-Turner syndrome. J Hand Surg Am. 2010;35(12):2104-2106.
- Sathasivam S, Lecky B, Manohar R, Selvan A. Neuralgic amyotrophy. J Bone Joint Surg Br.
2008;90(5):550-553. - Fransz DP, Schönhuth CP, Postma TJ, van Royen BJ. Parsonage-Turner syndrome following post-exposure prophylaxis. BMC Musculoskelet Disord. 2014;15:265.
- van Eijk JJ, Groothuis JT, Van Alfen N. Neuralgic amyotrophy: an update on diagnosis, pathophysiology, and treatment. Muscle Nerve. 2016;53(3):337-350.
- van Alfen N, van Engelen BG. The clinical spectrum of neuralgic amyotrophy in 246 cases. Brain. 2006;129(Pt 2):438-450.
- Gstoettner C, Mayer JA, Rassam S, et al. Neuralgic amyotrophy: a paradigm shift in diagnosis and treatment. J Neurol Neurosurg Psychiatry. 2020;91(8):879-888.
- Sneag DB, Rancy SK, Wolfe SW, et al. Brachial plexitis or neuritis? MRI features of lesion distribution in Parsonage-Turner syndrome. Muscle Nerve. 2018;58(3):359-366.
- Feinberg JH, Nguyen ET, Boachie-Adjei K, et al. The electrodiagnostic natural history of parsonage-turner syndrome. Muscle Nerve. 2017;56(4):737-743.
- van Alfen N, van Engelen BG, Hughes RA. Treatment for idiopathic and hereditary neuralgic amyotrophy (brachial neuritis). Cochrane Database Syst Rev. 2009;2009(3):CD006976.


