Published on
Urgent message: Fractures are common among pediatric patients. Familiarity with the growth process and the unique properties of the immature skeleton—as well as immediate identification of conditions requiring emergent referral—are necessary for appropriate care and avoidance of long-term sequelae. The first of two parts.
Justin Kunes, MD, Shane R. Hanzlik, MD, Allison Gilmore, MD
Injuries that ultimately prove to be fractures are a common cause of visits to the emergency room and urgent care among pediatric patients. Approximately 20% of children who seek attention for an injury will have a fracture.1 From birth to age 16, the chance of sustaining a fracture is 42% in boys and 27% in girls, with the most common sites being, in order, the distal radius, clavicle, hand, elbow, and tibia.2
Anatomy
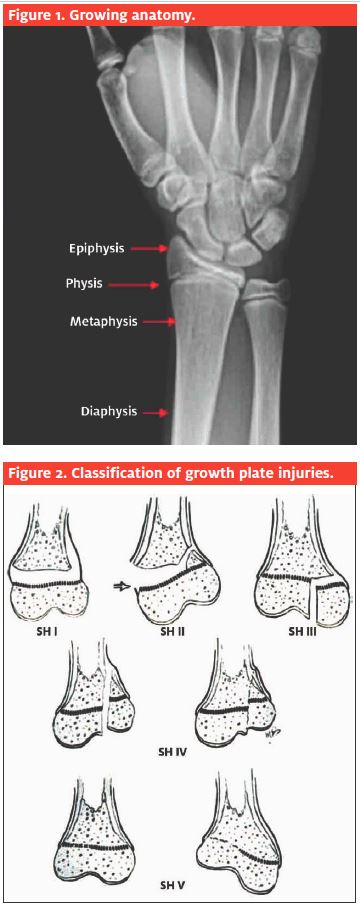
Growing bones (Figure 1) differ from skeletally mature bones in that their inherent nature allows for increasing length and diameter. Such “growing bones” includes the epiphysis, physis, metaphysis, diaphysis, and the periosteum.
The importance of the physis
As children’s bones are different from adult bones, care of their fractures also differs. Where adult fractures must be aligned perfectly, many children’s fractures can be left angulated.
This is because the growing child’s bone, when fractured at or near the growth plate, can remodel even severe deformities.3-5
However, fractures that do occur at the growth plate may cause a physeal arrest with subsequent growth disturbance. The physis is injured in as many as 27% of all fractures in children.6
The most prevalent classification system for growth plate injuries is the Salter-Harris classification system (Figure 2), which divides the injury anatomically by
describing which direction the fracture line propagates.7
The fact that immature bone is more resilient to stressful conditions (and therefore more likely to “bounce back” to its original shape) is evident in the following injury patterns in growing bones:
- Plastic deformation. Immature bones break differently than adult bones. In fact, they actually bend more than they break; when a bone is bent but no fracture line is evident, this is referred to as “plastic deformation.” The deformity can be straightforward (Figure 3) and can be gently manipulated into anatomic alignment with the child medically sedated.
- This injury may also be more complex, such as when plastic deformations of the ulna shaft in the fore- arm causes a radial head dislocation. Therefore, when plastic deformation is noted, it is important to look at the joint above and below the injury. If the ulna is bowed and the radial head is not aligned with the capitellum, then a Monteggia variant is suspected; if this is confirmed, it must be reduced immediately.8
- Torus fracture. Torus (buckle) fractures are among the most common types of fractures in children (Figure 4). These fractures are quite stable, result from a compressive force to the bone, and usually heal uneventfully. However, they still require immobilization in a splint, followed by a cast.
- Repeat x-rays in a few weeks will show callus formation, indicating the body’s healing response by forming new bone.
- Greenstick fracture. Greenstick fractures (Figure 5) occur when the causative force results in a break in one side of the bone while the opposite side just bends. This is due to the thick, flexible nature of immature bone.
Unique Properties of the Immature Skeleton
Fractures in children tend to heal faster than those in adults. This presents a distinct advantage in the form of shorter periods of immobilization.
The disadvantage is that misaligned fragments be- come “solid” sooner. Mild angular deformities remodel themselves if a child has more than two years of growth remaining.
Rotational deformities require reduction and do not remodel in children or adults.
Fractures in children may stimulate longitudinal growth, and sometimes the injured extremity becomes longer than the unaffected limb.
Often, children do not become as stiff as adults after immobilization and may return to sports and activities of daily living at earlier rates.

Upper Extremity Physical Examination
The upper extremity exam in a child with a suspected fracture may be somewhat difficult (especially in the very young), if for no other reason than the child will be in pain and may be too frightened to help with localizing the injury.
After an appropriate history, begin the exam by looking at the position of the extremity.
If there is an unstable fracture, usually the child will not move the involved extremity.
If a child is actively using the extremity, it is unlikely (though not impossible) that the injury is actually a fracture.
Note swelling, redness, open wounds, and/or deformity.
If the child can localize the area of pain, then start the exam away from the noted area of pain.
Even if you are fairly certain the child has a wrist injury, make sure to gently squeeze the forearm, elbow, and shoulder since multiple fractures at varying locations are often missed. Palpate the area that hurts gently. Check to see if the range of motion is decreased, compared with the opposite side.
Vascular assessment
Vascular assessment includes checking for palpable pulses (radial and ulnar arteries) and making sure the fingers are warm and pink.
Check capillary refill at the tips of the fingers.
If there is no pulse, do a Doppler exam. If there is still no pulse, then immediate transfer to the emergency room is needed so an orthopedic surgeon and vascular surgeon can get the patient to the operating room.
Begin the sensory exam by assessing light touch sensation over the dorsal aspect of the thumb (radial nerve), tips of the fingers (median nerve), and ulnar side of the ring finger and radial and ulnar side of the little finger (ulnar nerve).

Begin the motor exam by observing active wrist and finger flexion (median nerve) and extension (radial nerve).
Have the patient make an “O sign” with the index finger and thumb (anterior interosseous branch of the median nerve).
Have the child abduct and his or her fingers (ulnar nerve).
Perform all of these assessments prior to infiltration with local anesthetics, as both neurologic and vascular examinations will be affected.
Do not use epinephrine in a digit, due to the theoretical risk of distal ischemia.
As touched on previously, it is important to also assess the elbow joint with a wrist injury (and vice versa). The forearm is an interlinked structure that can be thought of as two main parts interconnected to and by multiple structures. Injuries include dislocation and supracondylar, lateral, and medial condyle fractures.
The carpal bones should also be assessed. An easily overlooked, common site for fractures is the scaphoid (the radial-most proximal row carpal bone). Left untreated, such a fracture can result in significant disability with early-onset arthritis.
If a patient is tender in the “anatomic snuffbox” (formed at the base of the thumb metacarpal between the extensor pollicis longus and abductor pollicis longus and extensor pollicis brevis tendons), wrist radiographs should be obtained; obtain four views, including a specialized PA view with the wrist ulnarly deviated.
The thumb should be included in the immobilization, even if this fracture is not clearly visualized until the patient can be reassessed by an orthopedist and their radiographs reviewed.
Special Complication: Compartment Syndrome
Compartment syndrome is defined by in- creased tissue pressure within the non- distensible fascial compartments of a limb (forearm, arm, leg, thigh), resulting in ischemia to the tissues and, ultimately, muscle death.
If children have significant pain that is not improving following reduction and splinting, they must be monitored clinically with serial hourly physical examinations.
In adults, pain with passive extension of the fingers or toes is the most reliable early symptom of compartment syndrome in adults. However, this is often unreliable in children, and the only indicator may be increasing narcotic requirements. Splints must be removed and the site examined for tight compartments. Neurologic and vascular examination should be compared with those obtained prior to intervention.
Suspected compartment syndrome warrants immediate surgical evaluation by any available surgical consultant.
It is important to note that transfer time to a tertiary care center is a critical factor; the more time that elapses, the more significant the risk that the child will suffer ischemic insult. Once this occurs, permanent injury happens in a matter of hours.
If a compartment syndrome is suspect- ed, the child must be taken to the operating room and fasciotomies performed; this can be limb-saving.
Compartment pressures in awake children are not always indicated, and physical exam alone may be enough.

Conclusion
Nearly 20% of children coming to the urgent care center with an injury will have a fracture. It is important to remember that physeal injuries are very common and may present with no radiographic findings.
Occult injuries are also possible in the shaft of the bone in kids. Even if you are in doubt as to the correct diagnosis, it is advis- able to splint a suspected fracture in a child. If a fracture displaces, a physeal arrest may occur.
A thorough history and exam, adequate radiographs, and a good splint with care to avoid pressure over bony prominences will help patients and their families get through the healing process with as little discomfort as possible.
With appropriate and efficiently administered care, children heal more quickly than adults and, barring complications, usu- ally return to full pre-injury activity level. n
References
- Buckley SL, Gotschall C, Robertson W Jr, et The relationships of skeletal injuries with trauma score, injury severity score, length of hospital stay, hospital charges, and mortality in children admitted to a regional pediatric trauma center. J Pediatr Orthop. 1994;14(4):449-453.
- Landin Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950-1979. Acta Orthop Scand Suppl. 1983;202:1-109.
- Friberg Remodeling after distal forearm fractures in children. III. Correction of residual angulation in fractures of the radius. Acta Orthop Scand. 1979;50(6, Pt 2):741-749.
- Friberg Remodeling after distal forearm fractures in children. II. The final orientation of the distal and proximal epiphyseal plates of the radius. Acta Orthop Scand. 1979;50(6 Pt 2):731-739.
- Friberg Remodeling after distal forearm fractures in children. I. The effect of residual angulation on the spatial orientation of the epiphyseal plates. Acta Orthop Scand. 1979. 50(5):537-546.
- Lopez WA, Rennie A survey of accidents to children aged under 15 years seen at a district hospi- tal in Sydney in one year. Med J Aust. 1969;1(16):806-809.
- Salter RB, Harris Injuries involving the epiphyseal plate. J Bone Joint Surg Am. 1963;4 (3):587-622.
- Mabrey JD, Fitch Plastic deformation in pediatric fractures: mechanism and treatment. J Pediatr Orthop. 1989;9(3):310-314.



