Urgent message: Be on the lookout for periostitis in patients with syphilis who present with extremity pain.
MAY MOHTY, MD, FAAP, FAAUCM, and CASEY PHILIPSBORN, MSIV
Syphilis (from the Greek word Syphlos, meaning crippled) is an infectious disease caused by the spirochete species Treponema pallidum. Patients can present with manifestations of any of the three stages of syphilis, ranging from a painless ulcer to an asymptomatic rash, to general paresis and dementia, among a myriad of other clinical findings. Secondary syphilis can present with a diverse range of symptoms including fever, malaise, headache, and rash. Uveitis, periostitis and osteomyelitis are less common.
Although syphilis was a rare finding at the turn of the 21st century, in the past 8 years, syphilis rates have almost doubled in the United States, particularly in men.1 This highlights the need for physicians to recognize the variety of signs and symptoms of syphilis in the outpatient setting so that it can be diagnosed and treated in a timely manner. This case emphasizes the importance of a thorough history and physical as well as the pursuit of additional laboratory and imaging studies.
Case Presentation
A 62-year-old white male was referred to an urgent care center by his primary care physician for “fatigue and dizziness.” The patient noted these symptoms had been progressively worsening for 2 months, during which time he said he had been hospitalized twice for “severe diarrhea and dehydration.” The patient reported weight loss of 60 lb over the preceding 6 months. Review of systems was positive for shortness of breath on exertion, a rash and significant pain in his shins and ankles. At that time, the patient was on furosemide, spironolactone, sildenafil, carvedilol, aspirin, clopidogrel, and simvastatin. He reported no history of smoking, admitted to drinking socially, and denied illicit drug use. The patient is in a homosexual relationship and stated that he was tested for sexually transmitted diseases, including HIV, and all results were negative.

Physical Exam
On initial presentation, vital signs were:
- BP: 105/73
- Pulse: 91
- Respiratory Rate: 20
- Temperature: 97.9°F
- SpO2: 98%
The patient’s physical exam was significant for a single non-bleeding ulceration of the lower left buccal mucosa and an extensive maculopapular rash over the entirety of his trunk, back, arms, legs, and palms bilaterally (Figures 1-3). There was significant tenderness to light palpation of bilateral shins and ankles. Orthostatic vitals were negative and there were no cardiopulmonary findings on examination. The rash, particularly being present on the palms of the hands, and significant bone pain warranted further investigation.
Labs/Imaging
- CBC
- BMP
- RPR
- IgM and IgG Coccidioides antibodies
- EKG
- Right and left tibia-fibula x-rays
The patient’s chief complaint of dizziness in light of a cardiac history warranted an electrocardiogram, which was read as sinus rhythm. The CBC and BMP, reported in Table 1, did not demonstrate significant aberrancies, except for slightly low sodium at 132. Both lower extremity x-rays were read by the radiologist as normal, with no abnormalities in the bony structures, soft tissues, or articulations. At this point in time, the patient was discharged home on lower doses of antihypertensive medications. Spironolactone was discontinued. The patient was informed that results of send-out tests would be reported to him via phone and was instructed to follow up within the week with his primary care physician.
The laboratory results of coccidiodes antibodies were negative. RPR titer resulted positive (1:1024) and FTAAbs were positive as well. The patient was notified of the results and instructed to return to the urgent care center for treatment with penicillin G benzathine. Given continued, severe shin pain, the patient was also sent for a bone scan to rule out spirochete bone involvement.
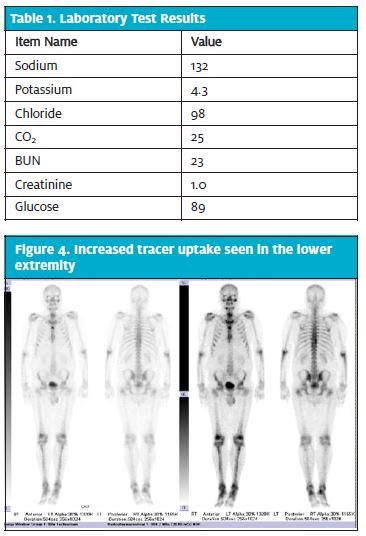
The decision was made to treat the patient with a daily dose of penicillin G benzathine, 2.4 million units, until bone scan results returned. Seven days after initial presentation and 3 days after diagnosis, a three-phase bone scan was performed after intravenous administration of Tc-99mMDP. The bone scan results were significant for mild, diffuse increase in tracer activity involver the lower extremities from the knees to the feet, indicative of mild periostitis (Figure 4).
The patient continued treatment with daily penicillin G benzathine for a total of 10 doses. By day 5 of treatment, the pain in the patient’s legs began to improve and, by day 10 of treatment, the pain was minimal.
It should be noted that in a subsequent visit with his primary care physician, the patient discussed a recent potential exposure to syphilis. HIV tests were repeated and found to be reactive both with ELISA screening and Western Blot results. The patient was referred to an infectious disease specialist for treatment of HIV.
Diagnosis
Secondary syphilis with bilateral tibial periostitis.

Discussion
With the reemergence of syphilis over the past decade, it is critical that health care providers are cognizant of the invariable versatile symptomatology and presentation of syphilis and its various stages. Diagnosis of early syphilis, including primary, secondary, and early latent syphilis, is key so that treatment can be initiated, thereby preventing further progression to tertiary syphilis and neurologic involvement of the disease. Furthermore, because syphilis facilitates the transmission of HIV, it is very important to diagnose and treat it in a timely manner to decrease HIV transmission.
Epidemiology
The number of syphilis cases peaked in the United States in the late 1980s and early 1990s. Following that, the nation reached an all-time low number of cases, prompting the Centers for Disease Control and Prevention (CDC) to discuss eradicating the disease, ultimately having fewer than 1,000 cases of the disease in the country by 2005.2 Unfortunately, since that time, the number of cases per 100,000 has significantly increased, particularly in men. The majority of cases in the United States occur in men who have sex with men (MSM) and these account for 65% of the cases. Up to 60% of such patients are also coinfected with HIV.3 That said, in the 21st century, the number of cases of syphilis in heterosexual patients has also risen.4 There is a recent increase in this diagnosis among women and infants. From ages 20 to 24, incidence of syphilis infection is much higher in black men, followed by Hispanic men, in comparison to white males of the same age group.1,3 Across the United States, the western regions have the highest rate of syphilis, totaling 6.5 cases/100,000 in 2013.1
Clinical Presentation
Syphilis is classically referred to as the “great imitator” of diseases.3 Infection with T pallidum is a multi-phasic disease, occurring in progressive stages if left untreated. Transmission of the spirochete infection occurs via direct contact with active lesions, often during intercourse. The initial stage of infection often presents within 3 weeks of exposure as a painless ulcer at the site of inoculation, usually on the genitalia or other mucosal surface. If left untreated, 4 to 8 weeks after initial infection, the disease will progress into secondary syphilis, which can present in a protean fashion.5 Patients may present with systemic complaints of fatigue, malaise, fever or weight loss. They may also experience pruritus, sore throats or headaches.6 On physical exam, nearly all patients with secondary syphilis will have dermatologic findings, although up to 25% may be unaware of any rash (source). The morphologic features of cutaneous lesions of secondary syphilis also greatly vary. They are often symmetric, macular, papular, follicular, or pustular, covering large portions of the trunk and extremities, including the palms and soles.7 Mucosal ulcerations are often common, and can be present in both primary and secondary syphilis, with overlap occurring more often in HIV-infected patients.8 Bone and joint pain is a recognized finding in congenital syphilis (known as saber shins), but it is a far less common finding in acquired disease.9 Bone involvement often occurs in the long bones and can also be found in the skull.9 Patients present with pain over the bony regions. Plain radiographs are often found to be negative, but bone scintigraphy demonstrates increased uptake in areas of disease involvement.9
Treatment
The standard treatment for primary syphilis is well documented, studied, and clinically proven to be a single intramuscular dose of penicillin G benzathine, 2.4 million units given intramuscularly. While there are case studies that suggest treatment should be extended (ranging from 2 to 10 days) for bone involvement, there are no extended studies validating these efforts.3,5-8 The CDC recommendation for treatment of tertiary syphilis is daily doses of penicillin G benzathine for 3 weeks.10 Patients coinfected with HIV should be treated according to staging of syphilis and given a one-time dose for early stages and 3 weeks of treatment for later stages of disease.10 Improvement in bone pain has been reported within weeks and resolution of bone scan abnormalities is achieved within 3 to 4 months.3,11 In this case, the patient reported improvement in bone pain after 1 week of daily treatment. Follow-up repeat bone scan has not been done yet and will be left to the discretion of the patient’s primary care physician and infectious disease specialist.
References
- Patton M, Su J, Nelson, R, Weinstock H. Primary and Secondary Syphilis – Unites States, 2005-2013. MMWR. 2014;63(18);402-406.
- Mitka M. US Effort to Eliminate Syphilis Moving Forward. JAMA. 2000;283(12):1555-1556.
- Fabricius T, Winther C, Ewertsen C, Kemp M, Nielsen S. Osteitis in the dens of axis caused by Treponema pallidum. BMC Infect Dis. 2013;13:347.
- McNabb S, Jajosky RA, Hall-Baker P, et. al. Summary of Notifiable Diseases – United States, 2006. MMWR. 2012;59(53):1-95.
- French P. Syphilis. BMJ. 2007;334 143-147.
- Chapel T. The Signs and Symptoms of Secondary Syphilis. Sex Trans Dis. 1980;7(4)161- 164.
- Pleimes M, Hartschuh W, Kutzner H, et al. Malignant Syphilis with Ocular Involvement and Organism-Depleted Lesions. Clin Infect Dis. 2009;48:83-85.
- Zetola N, Engleman J, Jensen T, Klausner J. Syphilis in the United States: An Update for Clinicians With an Emphasis on HIV Coinfection. Mayo Clin Proc. 2007;82(9):1091-1102.
- Gurland I, Korn L, Edelman L, Walach F. An Unusual Manifestation of Acquired Syphilis. Clin Infect Dis. 2001;32:667-669.
- Centers for Disease Control and Prevention. 2010 STD Treatment Guidelines. 16 December 2010.
- Veerapen K, Halsey JP, Davidson F, et al. Periostitis in secondary syphilis: a place for bone scintigraphy. J Royal Soc Med. 1985;78:721.

